Medicare may cover partial hospitalization and inpatient mental health treatment if your doctor deems it as medically necessary. Part D prescription drug plans must cover antidepressant and antipsychotic medications. Growing older brings along with it a whole new set of physical and emotional challenges.
How much does Medicare pay for mental health care?
Medicare Part B (Medical Insurance) helps pay for these outpatient mental health services: One depression screening per year. The screening must be done in a primary care doctor’s office or primary care clinic that can provide follow-up treatment and referrals.
What services does Medicare cover?
Aug 09, 2018 · Coverage: Medicare helps pay for mental health care in a psychiatric hospital up to 190 days. After this time, Medicare may pay for care in a general hospital. Out-of-pocket costs for a psychiatric hospital are the same as any other hospital for …
Does Medicare pay for Psychotherapy services?
May 05, 2022 · Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered for mental health services through Medicare. Mental health services are a system of care that aim to assess, diagnose, treat, and counsel in an individual or group setting anyone who needs help alleviating mental or emotional illness, symptoms, conditions, and disorders.
Does Medicare cover outpatient mental health services?
Mental health care includes services and programs to help diagnose and treat mental health conditions. These services and programs may be provided in outpatient and inpatient settings. Medicare helps cover outpatient and inpatient mental health care, as well as prescription drugs you may need to treat a mental health condition.
Does Medicare cover treatment for depression?
What treatments are not covered by Medicare?
- Long-Term Care. ...
- Most dental care.
- Eye exams related to prescribing glasses.
- Dentures.
- Cosmetic surgery.
- Acupuncture.
- Hearing aids and exams for fitting them.
- Routine foot care.
Does Medicare take care of mental health?
Which of the following expenses would be paid by Medicare Part B?
Why do doctors not like Medicare Advantage plans?
Does Medicaid cover psychiatrist?
Does Medicare cover dental?
Who is Medicare through?
Does Medicare cover mental health?
Medicare Coverage of Mental Health Services. A person’s mental health refers to their state of psychological, emotional, and social well-being – and it’s important to take care of it at every stage of life , from childhood to late adulthood. Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered ...
Does Medicare cover marriage counseling?
Medicare does not cover other types of relationship counseling, such as marriage counseling. You’re only covered for mental health services from a licensed psychiatrist, clinical psychologist, or other health care professional who accepts Medicare assignment.
Does Medicare cover depression screening?
Coverage: A yearly depression screening and preventive visit does not cost anything if your doctor or health care provider accepts assignment.
What is Medicare Part B?
Coverage: Medicare Part B helps pay for a psychiatric evaluation. Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the approved amount, the Part B deductible, and coinsurance costs.
Can you get help with Medicare if you have limited income?
If you have limited income and resources, you may be able to get help from your state to pay your Medicare costs (like premiums, deductibles, and coinsurance) if you meet certain conditions.
Does Medicare cover alcohol abuse?
Medicare covers one alcohol misuse screening per year for adults with Medicare (including pregnant women) who use alcohol, but don’t meet the medical criteria for alcohol dependency. If your health care provider determines you’re misusing alcohol, you can get up to 4 brief face-to-face counseling sessions per year (if you’re competent and alert during counseling). You must get counseling in a primary care setting (like a doctor’s oce).
What is Part B in psychiatry?
Part B covers partial hospitalization in some cases. Partial hospitalization is a structured program of outpatient psychiatric services provided to patients as an alternative to inpatient psychiatric care. It’s more intense than the care you get in a doctor’s or therapist’s oce. This type of treatment is provided during the day and doesn’t require an overnight stay.
What is coinsurance in insurance?
Coinsurance—An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Can mental health problems happen to anyone?
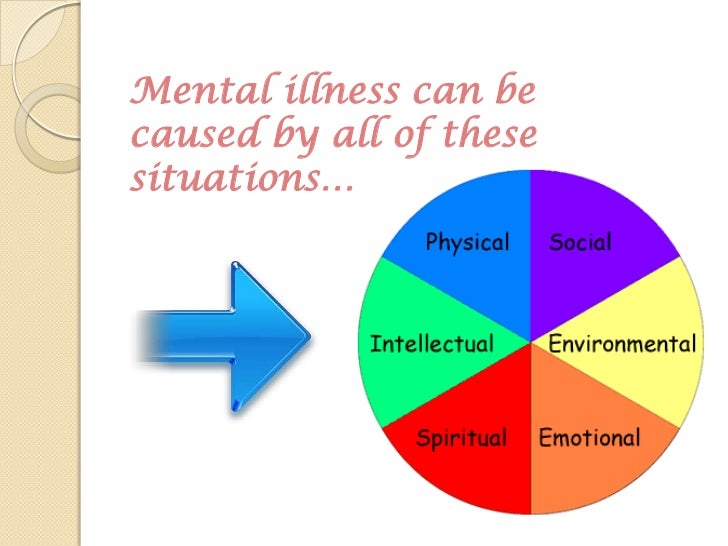
Mental health conditions, like depression or anxiety, can happen to anyone at any time. If you think you may have problems that affect your mental health, you can get help. Talk to your doctor or other health care provider if you have:
Does Medicare cover mental health?
Medicare Part A, your hospital insurance, covers mental health services that require your admission to a psychiatric or general hospital. If you’re in a psychiatric hospital, you’re covered for only up to 190 days of inpatient services over your lifetime. After that, you’d need to receive mental health services in a general hospital to be covered.
How much is the deductible for mental health?
What you’ll pay for inpatient mental health care. A deductible of $1,484 applies to inpatient psychiatric care for each benefit period. You will owe no coinsurance for the first 60 days of a hospital stay for psychiatric treatment. But you will owe copays of 20% of the Medicare-approved amount for mental health services you receive from doctors ...
How much is Medicare Part B deductible for 2021?
For outpatient mental health care, after you meet the Medicare Part B deductible, which is $203 in 2021, there are typically copayments of 20% for additional services. If you receive additional mental health services in hospital outpatient facilities, you may owe more.
What is Medicare Part B?
Medicare Part B, which pays doctor bills and related health care expenses, covers many mental health services rendered to patients not admitted to a hospital. Covered costs include: A “Welcome to Medicare” visit that includes a review of your risk factors for depression.
What is a welcome to Medicare visit?
A “Welcome to Medicare” visit that includes a review of your risk factors for depression. One depression screening per year, performed in the office of a primary care doctor or in a primary care clinic that provides follow-up treatment and referrals. Psychiatric evaluation to diagnose mental illness and prepare a care plan.
What is family counseling?
Family counseling that aids in your mental health treatment. Medication management and some prescription drugs that are not self-administered. Partial hospitalization, which typically includes many hours of treatment per week without admission to a hospital.
Who is John Rossheim?
About the author: John Rossheim is an editor and writer specializing in health care and workforce trends. His work has appeared in The Washington Post and on MSN, Monster and dozens of other websites. Read more
Medicare Part A
If your doctor gives an official order that you need inpatient care for your mental health, Medicare Part A covers your inpatient treatment.
Medicare Part B
Medicare Part B covers outpatient treatment for mental health concerns. This treatment is vital for managing chronic mental health conditions and addressing minor mental health problems before they become major concerns. You might receive this treatment at:
Medicare Part D
Medicare Part D can help pay for the medications commonly used to treat mental health conditions.
Medicare Advantage (Part C)
Medicare Advantage plans (also called Medicare Part C) offer the same mental health coverage as Original Medicare (Medicare Part A and Part B). They also usually have the same prescription drug coverage as Medicare Part D plans.
Medicare Supplement (Medigap)
Medicare Supplement plans are often called Medigap plans, and they can help cover some or all of the out-of-pocket costs of treating your mental health after Medicare Part A and Part B make their contributions.
Medicare Plus a Medicare Supplement Plan Can Help You Save Money for Mental Health Treatment
Navigating mental health problems can be challenging, but Medicare helps ensure you have one less thing to worry about.
Compare Medigap plans in your area
Zia Sherrell is a digital health journalist with over a decade of healthcare experience, a bachelor’s degree in science from the University of Leeds and a master’s degree in public health from the University of Manchester.
Commercial Insurance Reimbursement for Mental Health
Find out which insurance companies pay mental health providers the best in our interactive charts below:
Mental Health Credentialing Recommendations
In our experience, the higher the reimbursement rate, the higher your license level need be to become in-network with that company.
Tips on Avoiding Low Paying & Complex Plans
Avoid subcontracted plans if you don’t understand them. When a plan is subcontracted out to a different insurance provider, often times that network is smaller and offers different, lower rates. (This isn’t always the case!)
Medicare Psych Reimbursement Rates by CPT Code
Medicare pays well! Find the rate that Medicare pays per mental health CPT code in 2021 below.
Credentialing Advice for Mental Health Providers
Some companies require you to register a legal business, E-IN, and group NPI. You might decide you don’t want to bother with all of that added work.
Billing Advice
Try to avoid companies that require the use of taxonomy codes, license level modifiers, EDI enrollments, and prior authorizations. This does dramatically limit the companies you can work with, but it will save you time, headache, and frustration.
Reach Out
Consider hiring a service like TheraThink that exclusively does mental health insurance billing.