
Medication
Treatment for vaginal atrophy To undo some of the vaginal dryness, moisturizers like K-Y Liquibeads, or Replens are typically prescribed. If you’re sexually active, water-based lubricants like K-Y Jelly and Astroglide are helpful. These methods are simple, over-the-counter means of improving the condition.
Self-care
Some treatments are meant to treat the symptoms of atrophy. Others address the loss of estrogen, specifically, which will also act to relieve symptoms. Lubricants and moisturizers to add moisture and to loosen the vagina can treat dryness. This improves comfort during sex. The moisturizers won’t completely restore the health of the vagina.
Nutrition
Jul 31, 2018 · Abbreviation: VVA, vulvovaginal atrophy. The main therapeutic goal in managing VVA is to relieve symptoms and restore the vaginal environment to a healthy premenopausal state. However, despite the high prevalence and negative impact on the quality of life, VVA is under-reported by patients, undiagnosed by health care providers, and undertreated.
What are the best treatments for vaginal atrophy?
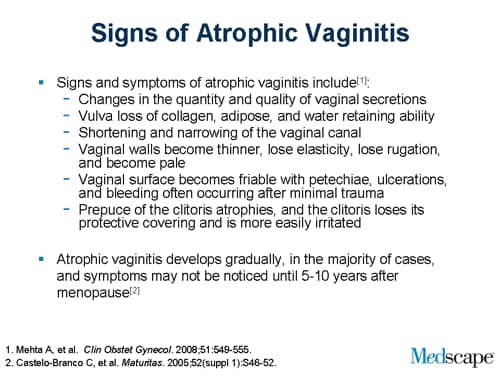
Vaginal atrophy also called “atrophic vaginitis”, “vulvar atrophy”, “labia atrophy” “vulvovaginal atrophy”, is said to occur when the walls of the vagina start getting thin, dry, and inflamed, which is a result of low estrogen in the body, hence leading to burning sensation when urinating, itching, painful sex, and urinary tract infections.
What helps vaginal atrophy?
Apr 08, 2022 · Until recently, treatments for vulvovaginal atrophy were limited to often insufficient or inappropriate oral estrogen therapies and over …
What medications are used for vaginal atrophy?
Can you treat vulvovaginitis at home?
What can be done for vulvar atrophy?
Topical estrogenVaginal estrogen cream (Estrace, Premarin). You insert this cream directly into your vagina with an applicator, usually at bedtime. ... Vaginal estrogen suppositories (Imvexxy). ... Vaginal estrogen ring (Estring, Femring). ... Vaginal estrogen tablet (Vagifem).Sep 17, 2021
Can vaginal atrophy be reversed?
Currently, estrogen replacement is the best way to reverse vaginal atrophy and GSM. Not every woman will be able to use this treatment option, however. Concerns about the long-term effects of increased estrogen sometimes discourage doctors from prescribing it.
Does vaginal atrophy need treated?
Estrogen therapy is considered to be the most effective. Some treatments are meant to treat the symptoms of atrophy. Others address the loss of estrogen, specifically, which will also act to relieve symptoms. Lubricants and moisturizers to add moisture and to loosen the vagina can treat dryness.Oct 27, 2020
What are symptoms of vulvar atrophy?
Vulvovaginal atrophy (VVA) is a common and underreported condition associated with decreased estrogenization of the vaginal tissue. Symptoms include dryness, irritation, soreness, and dyspareunia with urinary frequency, urgency, and urge incontinence.
What causes vulvar atrophy?
The most common cause of atrophic vaginitis is the decrease in estrogen after menopause. It can also occur after childbirth, and it can happen when anti-estrogen drugs are used to treat other conditions. The ovaries make estrogen until a woman experiences menopause.
What is vulvovaginal atrophy?
Vaginal atrophy, atrophic vaginitis, and urogenital atrophy are other terms used to describe this constellation of symptoms associated with decreased estrogenization of the vulvovaginal tissue.
How to treat whitened vulvovaginal area?
Apply low-dose estrogen cream to the vulvovaginal area and hydrocortisone cream to the whitened area. Apply hydrocortisone cream to the whitened area. Perform biopsy of the whitened area. Administer 1 dose of fluconazole (150 mg) orally, followed by application of low-dose estrogen cream to the vulvovaginal area.
What is a VVA?
Vulvovaginal atrophy (VVA) is a common and underreported condition associated with decreased estrogenization of the vaginal tissue. Symptoms include dryness, irritation, soreness, and dyspareunia with urinary frequency, urgency, and urge incontinence.
What happens if the pH in the vagina rises?
Without this cascade, the pH in the vagina rises, resulting in a loss of lactobacilli and an overgrowth of other bacteria, including group B streptococcus, staphylococci, coliforms, and diphtheroids12(Figure 1). These bacteria can cause symptomatic vaginal infections and inflammation.
Why does my vagina feel dry?
Vaginal spotting, due to small tears in the vaginal epithelium, may also occur.
Does topical estrogen cause dryness?
Although treatment with topical estrogen is effective in alleviating symptoms, women frequently do not report symptoms and thus go untreated.1,2. Common symptoms include vaginal dryness, irritation, postcoital bleeding, and soreness. These symptoms may be associated with vaginal discharge and dyspareunia.
Does estrogen cause VVA?
Even while taking systemic estrogen, 10% to 20% of women may still have residu al VVA symptoms . Breast cancer treatment increases the prevalence of VVA because the surgical, endocrine, and chemotherapeutic agents used in its treatment can cause or exacerbate VVA.
What is the best treatment for vaginal atrophy?
Treatment for vaginal atrophy. To undo some of the vaginal dryness, moisturizers like K-Y Liquibeads, or Replens are typically prescribed. If you’re sexually active, water-based lubricants like K-Y Jelly and Astroglide are helpful. These methods are simple, over-the-counter means of improving the condition. When you need something more, your OBGYN ...
When does vaginal atrophy occur?
As you might have guessed, vaginal atrophy typically happens to women as they age, most often during or after menopause, when estrogen production decreases within the body and the vagina loses its youthful elasticity. However, it can also happen in the years leading up to menopause (perimenopause), as estrogen levels also tend to drop ...
What is estrogen therapy?
Estrogen therapy comes in many forms. Topically, they include vaginal estrogen cream, a vaginal estrogen ring, and vaginal estrogen tablets. Systemically, estrogen therapy looks a bit different. Estrogen patches and pills, or an estrogen-progesterone patch may be prescribed.
What is it called when the vagina walls begin to thin?
Vaginal atrophy is just as it sounds — a deterioration of cells in the vagina. Also known as atrophic vaginitis, this condition occurs when the vagina’s walls begin to thin, dry out, and even become inflamed.
How do you know if you have vaginal atrophy?
You bleed lightly after sex. Your vagina may burn at times. It may also feel overly dry. You experience vaginal discharge.
What to eat to help vagina?
Eating to balance hormones can help support the health of your vagina. Locally grown organic fruits and vegetables, lots of pure drinking water, and high-fiber foods like avocados, berries, legumes, nuts and seeds are foods to eat regularly.
Does laser vaginal revitalization work?
Laser vaginal revitalization naturally increases blood flow and lubrication to help improve the natural function of the vagina. There is no anesthesia required, and many women report noticeable changes after just one session.
Why does vaginal atrophy occur during menopause?
Vaginal atrophy most often occurs during menopause, the “change of life.”. This happens because of a decrease in the hormone estrogen.
What is the difference between vaginal atrophy and genitourinary syndrome?
Vaginal refers to the vagina while atrophy means “a wasting away or diminution.”. Recently, the term vaginal atrophy has been replaced with the newer term, genitourinary syndrome of menopause (GSM).
How to tell if you have menopause or atrophy?
The healthcare provider can diagnose vaginal atrophy based on your symptoms and a pelvic exam to look at how the vagina appears. It will help to know whether or not you are in menopause. Classic signs of atrophy during a pelvic exam include: A shortened or narrowed vagina. Dryness, redness and swelling.
What is the difference between a yeast infection and a vaginal atrophy?
However, vaginal atrophy is caused by a lack of estrogen while a vaginal yeast infection is caused by a fungal infection.
What is the term for a condition where the lining of the vagina gets drier and thinner?
What is vaginal atrophy? Vaginal atrophy (also called atrophic vaginitis) is a condition where the lining of the vagina gets drier and thinner. This results in itching, burning and pain during sex, among other symptoms.
How to treat dryness in vagina?
Others address the loss of estrogen, specifically, which will also act to relieve symptoms. Lubricants and moisturizers to add moisture and to loosen the vagina can treat dryness.
What age is the most likely to have vaginal atrophy?
Women age 50 and over, in menopause, are the most likely to experience vaginal atrophy. Other factors that increase your likelihood of developing vaginal atrophy include: Lack of sexual intercourse. Decreased ovarian functioning due to chemotherapy or radiation. Immune disorders.
What is the term for thinning and drying of the vaginal walls?
Vaginal atrophy ( atrophic vaginitis) is thinning, drying and inflammation of the vaginal walls that may occur when your body has less estrogen. Vaginal atrophy occurs most often after menopause. For many women, vaginal atrophy not only makes intercourse painful but also leads to distressing urinary symptoms.
What is the term for menopause atrophy?
Because the condition causes both vaginal and urinary symptoms, doctors use the term "genitourinary syndrome of menopause (GSM)" to describe vaginal atrophy and its accompanying symptoms. Simple, effective treatments for GSM are available. Reduced estrogen levels result in changes to your body, but it doesn't mean you have to live with ...
Why does menopause cause genitourinary syndrome?
Causes. Genitourinary syndrome of menopause is caused by a decrease in estrogen production. Less estrogen makes your vaginal tissues thinner, drier, less elastic and more fragile. A drop in estrogen levels may occur: After menopause. During the years leading up to menopause (perimenopause)
How does sexual activity help menopause?
Regular sexual activity, either with or without a partner, may help prevent genitourinary syndrome of menopause. Sexual activity increases blood flow to your vagina, which helps keep vaginal tissues healthy.
Can you make an appointment for a vaginal spotting?
Make an appointment with your doctor if you have any unexplained vaginal spotting or bleeding, unusual discharge, burning, or soreness.
What is vulvovaginal atrophy?
Vulvovaginal atrophy is a frequently neglected symptom of menopause. While an estimated 10–40% of women are affected by the progressive symptoms of vaginal dryness, irritation, itching, dysuria and dyspareunia, only a quarter of symptomatic women are believed to seek medical attention. Until recently, treatments for vulvovaginal atrophy were limited to often insufficient or inappropriate oral estrogen therapies and over-the-counter lubricants and moisturizers. Currently, a broader range of treatments, which address symptom reduction and estrogen restoration to affected tissue, are being developed. Among these treatments are local estrogen, selective estrogen receptor modulators, tissue-selective estrogen complexes, local androgens, dehydroepiandrosterone, oxytocin, phytoestrogens and nonhormonal options. The aim of this article is to discuss current treatments for vulvovaginal atrophy. In addition, we will discuss alternative therapies and explore emerging strategies for care.
Is vulvovaginal atrophy a symptom of menopause?
Vulvovaginal atrophy is often described as a 'silent symptom' of menopause. While an estimated 10–40% of postmenopausal women are affected, only 25% of symptomatic women seek medical attention. This condition, which can have a large impact on quality of life and sexual function, is often underdiagnosed and undertreated.
Does vulvovaginal atrophy resolve?
Unlike vasomotor symptoms of menopause, which typically abate over time, vulvovaginal symptoms are usually progressive and less likely to resolve without effective treatment. [ 1, 2] Treatment approaches for vulvovaginal atrophy focus on symptom reduction and restoration of affected tissues. Options for care range from over-the-counter preparations ...
Treatment
Clinical Trials
Lifestyle and Home Remedies
Alternative Medicine
Specialist to consult
Preparing For Your Appointment
- To treat genitourinary syndrome of menopause, your doctor may first recommend over-the-counter treatment options, including: 1. Vaginal moisturizers.Try a vaginal moisturizer (K-Y Liquibeads, Replens, Sliquid, others) to restore some moisture to your vaginal area. You may hav…
Overview
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Symptoms
- If you're experiencing vaginal dryness or irritation, you may find relief if you: 1. Try an over-the-counter moisturizer.Examples include K-Y Liquibeads, Replens and Sliquid. This can restore some moisture to your vaginal area. 2. Use an over-the-counter water-based lubricant.A lubricant can reduce discomfort during intercourse. Examples include Astroglide, K-Y Jelly and Sliquid. 3. Allo…
Causes
- Some alternative medicines are used to treat vaginal dryness and irritation associated with menopause, but few approaches are backed by sufficient evidence from clinical trials. Interest in complementary and alternative medicine is growing, and researchers are working to determine the benefits and risks of various alternative treatments for genitourinary syndrome of menopaus…
Risk Factors
- You'll probably start by discussing your symptoms with your primary care provider. If you aren't already seeing a doctor who specializes in women's health (gynecologist or internal medicine women's health specialist), your primary care provider may refer you to one.
Complications
- Vaginal atrophy (atrophic vaginitis) is thinning, drying and inflammation of the vaginal walls that may occur when your body has less estrogen. Vaginal atrophy occurs most often after menopause. For many women, vaginal atrophy not only makes intercourse painful but also leads to distressing urinary symptoms. Because the condition causes both vaginal and urinary sympto…
Prevention
- Genitourinary syndrome of menopause (GSM) signs and symptoms may include: 1. Vaginal dryness 2. Vaginal burning 3. Vaginal discharge 4. Genital itching 5. Burning with urination 6. Urgency with urination 7. Frequent urination 8. Recurrent urinary tract infections 9. Urinary incontinence 10. Light bleeding after intercourse 11. Discomfort with intercourse 12. Decreased …