Full Answer
What is a vascular loop in the brain?
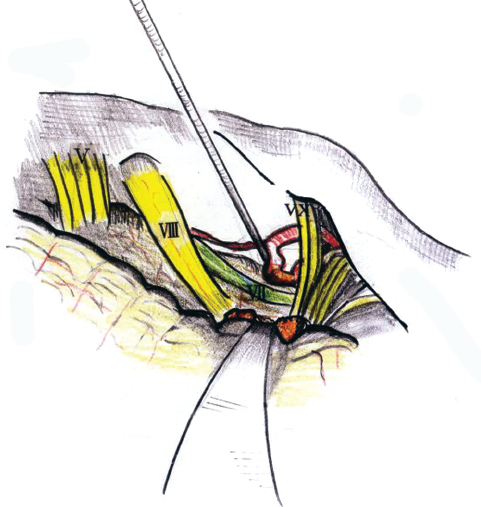
These vascular loops are suspected of causing hearing loss, tinnitus, and vertigo, and surgery has been advocated to separate the vascular loop from the eighth cranial nerve. Previous reports have described pathologic anatomy, surgical approaches, and results of treatment. In this study, we report the results of a uniform battery of audiometric and vestibular system test results …
What is a vascular loop in hearing loss?
Apr 25, 2015 · In some cases, it is believed that the etiology involves a vascular loop in the anterior inferior cerebellar artery (AICA), insinuating itself into the internal auditory meatus.
What is the treatment for tinnitus for vascular loop syndrome?
vascular loop, in which the loop compresses the nerve and the nerve compromises circulation to the inner ear. The findings of a cochlear type of hearing loss, excellent speech discrimination and normal caloric test results should raise the suspicion of a vascular loop [16]. A loop in contact with the vascular wall might cause pulsatile
What is the pathophysiology of vascular loop syndromes?
Feb 27, 2014 · Our patient has a vascular loop which originates from the AICA around the cisternal portion of the vestibulocochlear and facial nerves which may have explained her pulsatile tinnitus. In most reported cases, vascular loop around the seventh and eighth nerve would cause pulsatile tinnitus, hearing loss, vertigo and hemifacial spasm (Kim et al., 1990[ 6 ]; …

How is a vascular loop treated?
Conclusion: Vascular loops in the internal auditory canal may generate pulsatile tinnitus. It may be treated by placing Teflon between the cochlea and the intrameatal vascular loop. One then does not hear the pulsation of the carotids due to a dampening effect of a pericarotid venous plexus.
What is a vascular loop?
It passes the IAC outside the meatus (19%–40%), at the meatus (33%–56%), or within the IAC (25%–27%) [Van der Steenstraten et al., 2007]. Vascular loops are anatomical abnormalities that arise from the branches of the basilar artery (98%) or from the vertebral artery (2%) [Ensari et al., 2017].
Is vascular loop curable?
It is rarely performed for vestibular paroxysmia. The blood vessel is delicately separated from the nerve, and a piece of Teflon is then inserted between the blood vessel and the nerve. Although it may cure vertigo, it does not help with tinnitus.
Are vascular loops normal?
There is a diverse variability in vascular anatomy at CPA and IAC with nondependent association between location of the vascular loop and clinical profile. Therefore, the presence of vascular loops in contact with the 8th cranial nerve is not always considered pathological but likely to be a normal anatomical variant.Jul 7, 2020
Can a vascular loop cause hearing loss?
These vascular loops are suspected of causing hearing loss, tinnitus, and vertigo, and surgery has been advocated to separate the vascular loop from the eighth cranial nerve. Previous reports have described pathologic anatomy, surgical approaches, and results of treatment.
Can vascular loop causes vertigo?
Abstract. A vascular loop in the internal auditory canal pressing upon the vestibular nerve was found in a series of eight patients with episodic vertigo and severe motion intolerance. All patients had failed medical and surgical therapy for vestibular Meniere's disease, which this syndrome closely mimics.
Can vascular loop cause headaches?
Vascular loop in the cerebellopontine angle causing pulsatile tinnitus and headache: a case report.Feb 27, 2014
What is a Type 3 vascular loop?
The Chavda classification grades the vascular loops in the AICA as follows(8): grade I - when an AICA vascular loop borders the internal auditory meatus (internal acoustic pore); grade II - when the loop insinuates itself into the internal auditory meatus but occupies 50% or less of the canal; or grade III - when the ...
What is a small vascular loop?
Vascular loops are anatomical anomalies of the anterior inferior cerebellar artery (AICA). We mention that artery because it is the blood supply for the inner ear, which includes hearing and vestibular (balance) systems.May 30, 2017
What is a prominent vascular loop?
Vascular loops are anatomical anomalies of the anterior inferior cerebellar artery (AICA). We mention that artery because it is the blood supply for the inner ear, which includes hearing and vestibular (balance) systems.
What is Type 2 vascular loop?
Vascular loop of the AICA is classified into 1: type I: vascular loop within the cerebellopontine angle level. type II: vascular loop proximal to the IAC extends to less than 50% of the canal. type III: vascular loop distal to the IAC extends to more than 50% of the canal.Jan 24, 2019
What causes microvascular compression?
What is Microvascular Compression Syndrome? In microvascular compression syndrome (MCS), vertigo, tinnitus and motion intolerance is attributed to irritation of the 8th cranial nerve by a blood vessel.Jun 2, 2003
Why use CISS sequence?
Using CISS sequence can offer better visualization and further clarification of the relation between vascular and neurological structures in CPA and IAC. There is a diverse variability in vascular anatomy at CPA and IAC with nondependent association between location of the vascular loop and clinical profile. Therefore, the presence of vascular loops in contact with the 8th cranial nerve is not always considered pathological but likely to be a normal anatomical variant. Subsequently, this radiological finding alone should not be used to qualify patient for further invasive microvascular decompression surgery.
What is open access?
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author (s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
What are the vascular loops of the AICA?
The vascular loops of the AICA were graded as previously described by Chavda in McDermott et al. [ 16] as follows: grade I—when an AICA vascular loop borders the internal auditory meatus (internal acoustic pore), lying only in the CPA but not entering the IAC; grade II—when the loop insinuates itself into the internal auditory meatus but occupies 50% or less of the canal; or grade III—when the loop occupies more than 50% of the canal. In addition, we also categorized the presence of vascular contact with the 8th cranial nerve into type I—no contact, type II—contact without nerve angulation, and type III—contact with 8th cranial nerve angulation.
What is the triad of inner ear disease?
Tinnitus, sensorineural hearing loss (SNHL), and vertigo are common audio-vestibular symptoms and they are well-known classic triad in inner ear disease involving the membranous labyrinth [ 1 ]. However, in absence of inner ear disease, the exact cause is not always recognized. It has been proposed that compression of the vestibulocochlear nerve ...
What is the cause of vertigo and tinnitus?
Many diseases are associated with these symptoms; however, the exact cause is not always identified. Some studies show that the etiology could be related to the presence of a vascular loop in contact with the 8th cranial nerve.
Who suggested VCS?
Initially, the hypothesis of VCS was suggested by McKenzie in 1936 and later, discussed by Jannetta in 1975, to refer to cranial nerve dysfunction [ 2 ]. Various explanations were assumed to explain the impaired nerve’s function as an effect of vascular compression.
Is vascular loops pathological?
Therefore, presence of vascular loops in contact with the 8th cranial nerve is not certainly considered pathological but possibly to be a normal anatomical coincidental finding.
Why do you inject contrast dye into your vein?
In some cases a contrast dye is injected into a vein to look at the brain tissue in a different way, and to evaluate your blood vessels (magnetic resonance angiography or magnetic resonance venography).
Can a vascular malformation be treated with medication?
These are usually caused by other vascular malformations that can be found with a venous malformation. Doctors typically treat seizures with medications. Some hemorrhages require surgery, but many hemorrhages can be treated with medical management and observation in a hospital.
Can a doctor treat intracranial venous malformations?
Doctors usually don't treat intracranial venous malformations because they rarely cause symptoms. If you have unrelated symptoms, such as headaches, your doctor might prescribe medications. Rarely, people who have intracranial venous malformations have seizures or bleeding in the brain (brain hemorrhage).