What are the treatment options for hepatitis C?
HCV = hepatitis C virus; PPI = proton pump inhibitor Go to: LEDIPASVIR/SOFOSBUVIR The approval of the combination of ledipasvir 90 mg and sofosbuvir 400 mg (LVD/SOF) (Harvoni, Gilead Sciences) as a single-tablet formulation in October 2014 ushered in …
What is the other name for hepatitis C?
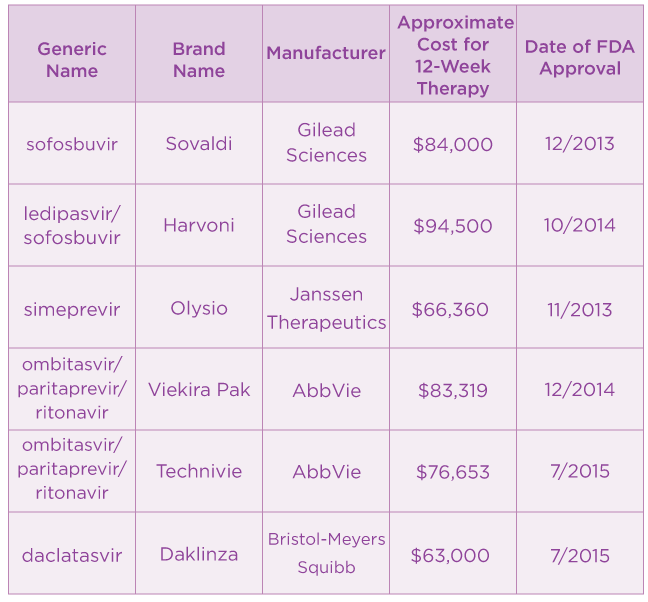
Dec 25, 2021 · One concern for people seeking treatment for hepatitis C is cost. When these medications were introduced, the cost of one full treatment course could reach about $100,000 per patient. Pharmaceutical companies began producing generic versions, which lowered the price to $24,000 still, a significant cost.
How often should you get tested for hepatitis C?
Hepatitis C drugs are pricey · Harvoni costs $94,500 for a 12-week treatment · Mavyret costs $39,600 for a 12-week treatment · Zepatier costs (1) … Nov 21, 2018 — A 28-day supply costs $22,120, and a 12-week supply costs $66,360. Sometimes a doctor will prescribe this along with the medication sofosbuvir, How much is it?
Is chronic hepatitis C life-threatening?
Drugs used to treat Hepatitis C. The following list of medications are in some way related to or used in the treatment of this condition. Select drug class All drug classes miscellaneous antivirals (2) purine nucleosides (5) antineoplastic interferons (4) antiviral combinations (12) antiviral interferons (4) inhaled anti-infectives (5) Rx. OTC.
What is the cost of treating hep C?
The cost of hep C treatment varies depending on the type of drug. However, an 8- to 12-week course can range from $54,000 to $95,000 (or higher). For example, the price of a 12-week course of Zepatier can be as much as $54,600, and a 12-week course of Harvoni can cost as much as $94,500.Sep 2, 2021
How much does Mavyret cost without insurance?
How much does Mavyret cost without insurance? Without insurance, the customers pay an average of $3,168.19 for a refill of Mavyret. However, when you claim your SingleCare savings, you pay a discounted retail price of $2,634.56 for this prescription drug at your neighborhood pharmacy.
How much do direct-acting antivirals cost?
Conclusions: Within the next 15 years, large-scale manufacture of 2 or 3 drug combinations of HCV DAAs is feasible, with minimum target prices of $100-$250 per 12-week treatment course. These low prices could make widespread access to HCV treatment in low- and middle-income countries a realistic goal.
How do you pay for hep C treatment?
Funding Resources Available to Hep C PatientsPharmaceutical Programs. ... The American Liver Foundation (ALF) ... NeedyMeds. ... Help-4-Hep. ... The HealthWell Foundation. ... The Pharmaceutical Research and Manufacturers of America (PhRMA) ... The Patient Access Network (PAN) Foundation. ... The Patient Advocate Foundation.Jun 9, 2021
Does MAVYRET make you sick?
Common side effects of Mavyret include nausea, headache, fatigue (lack of energy), and diarrhea. These side effects could make you feel unwell. While taking Mavyret, talk with your doctor if you feel sick or have side effects that become severe or don't go away.Jan 22, 2021
What is the success rate of MAVYRET?
Yes, Mavyret is a treatment that can clinically cure hepatitis C viral infection (HCV). The success rate for curing hepatitis C with Mavyret ranges from 95 to 99%.Jul 22, 2020
How much is hep C treatment in India?
The generic version of these drugs are available in cities such as Bengaluru Hyderabad and Chennai at the cost of Rs70000 or around $1000 USD for the entire treatment regimen.
What is the antiviral drug ribavirin?
Ribavirin, also known as tribavirin, is an antiviral medication used to treat RSV infection, hepatitis C and some viral hemorrhagic fevers. For hepatitis C, it is used in combination with other medications such as simeprevir, sofosbuvir, peginterferon alfa-2b or peginterferon alfa-2a.
What is DAA treatment?
Importance Direct-acting antiviral (DAA) drugs are highly effective in curing hepatitis C virus (HCV) infection. Previous simulations showed extended life as a key health advantage of DAA drugs, but real-world evidence on the association between DAA treatment and reduced mortality is limited.Jul 21, 2020
Will you always test positive for hep C?
A reactive or positive antibody test means you have been infected with the hepatitis C virus at some point in time. Once people have been infected, they will always have antibodies in their blood. This is true if they have cleared the virus, have been cured, or still have the virus in their blood.
How much does hep C treatment cost UK?
A 12-week course of treatment with elbasvir-grazoprevir usually costs £36,500 per patient, but the NHS will pay less than this as the company has offered a confidential discount. Taken once daily, the tablet could treat around 4,000 patients in the first year, alongside other options already available for hepatitis C.
How much is sofosbuvir cost?
Sofosbuvir (Sovaldi): This medication costs $1,000 per 400 mg pill. The total cost for a 12-week course is around $84,000, and doctors will typically prescribe it with other medicines, such as simeprevir.Nov 21, 2018
Drugs used to treat Hepatitis C
The following list of medications are in some way related to, or used in the treatment of this condition.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
How long does it take to get tested for hepatitis C?
Getting tested for hepatitis C is important, because treatments can cure most people with hepatitis C in 8 to 12 weeks.
How is hepatitis C spread?
Hepatitis C is spread through contact with blood from an infected person. Today, most people become infected with the hepatitis C virus by sharing needles or other equipment used to prepare and inject drugs.
Can you get hepatitis C if you don't have symptoms?
People with chronic hepatitis C can often have no symptoms and don’t feel sick. When symptoms appear, they often are a sign of advanced liver disease. There is no vaccine for hepatitis C. The best way to prevent hepatitis C is by avoiding behaviors that can spread the disease, especially injecting drugs.
What is cost effectiveness analysis?
Cost-effectiveness analysis (CEA) compares the relative costs and outcomes of 2 or more interventions. CEA explicitly recognizes budget limitations for healthcare spending and seeks to maximize public health benefits within those budgetary constraints. The core question that CEA addresses is whether to invest limited healthcare dollars in a new treatment/therapy or use that money to invest in another healthcare intervention that would provide better outcomes for the same monetary investment. The focus of CEA is, therefore, not simply cost or saving money but health benefits. It assumes that all available resources will be spent and provides a framework for prioritizing among available treatment options by formally assessing the comparative costs and health benefits accrued from a new treatment relative to current treatment.
What is the time horizon for CEA?
From a societal perspective, CEA uses a lifetime time horizon, meaning it considers lifetime costs and benefits, including those that occur in the distant future. Business budget planning, however, typically assumes a 1-year to 5-year perspective.
What does private insurance do?
Private insurance companies often have separate pharmacy and medical budgets, and use PBMs or directly negotiate drug pricing with pharmaceutical companies. Insurance companies determine formulary placement, which impacts the choice of regimens and out-of-pocket expenses for patients.
Is life expectancy a measure of benefit?
Life expectancy is a valuable measure of benefit but considering only mortality benefits fails to recognize the value of treatments that improve quality of life. The quality-adjusted life-year (QALY) provides a measure that integrates both longevity and quality of life and is the preferred outcome for CEA.
Is an intervention cost effective?
An intervention that is cost-effective is not necessarily affordable. Affordability refers to whether a payer has sufficient resources in its annual budget to pay for a new therapy for all who might need or want it within that year . Several characteristics of CEA limit its ability to speak to the budgetary impact of interventions being implemented in the real world.
Is HCV cost effective?
There is no formula that provides a good means of integrating the concerns of value and affordability. When new HCV therapies are deemed cost-effective, it indicates that these therapies provide good benefit for the resources invested and providing such therapy to more people would be a good long-term investment.
Is routine HCV testing cost effective?
Generally, routine HC V testing is cost-effective because the incidence and prevalence of HCV remain high in people who inject drugs with a notable rising prevalence in young adults who may not readily report their stigmatized risk behaviors.
How many genotypes of hepatitis C are there?
There are six genotypes, or strains, of the hepatitis C virus, and people with certain genotypes respond more quickly to medical treatment. For many years, the standard treatment for chronic hepatitis C consisted of the antiviral medications pegylated interferon and ribavirin.
How long does it take for hepatitis A to clear up?
Rest and Hydration. Most people with hepatitis A do not require treatment. This type of hepatitis usually clears up on its own after a few weeks or months. Your NYU Langone doctor may recommend getting lots of rest and drinking plenty of water. You should avoid alcoholic beverages because drinking alcohol can delay recovery.
What is the best treatment for hepatitis B?
Antiviral medication prevents the virus from replicating, or creating copies of itself, and may prevent progressive liver damage. Currently available medications can treat hepatitis B with a low risk of serious side effects.
How long does hepatitis B last?
Acute hepatitis B, a short-term illness that usually lasts a few months, also rarely requires treatment and may not cause symptoms. NYU Langone doctors recommend lots of rest, adequate fluids, and a nutritious diet to help your body fight the virus.
Is interferon free treatment for hepatitis C?
These medications, which include sofosbuvir, are very effective and have fewer side effects than older medications, particularly interferon. At NYU Langone, interferon-free treatment is now the standard of care.
Does NYU Langone prescribe antiviral medication?
NYU Langone hepatologists and infectious disease specialists prescribe medication when they have determined that without treatment, the hepatitis B virus is very likely to damage the liver over time. People with chronic hepatitis B may need to take antiviral medication for the rest of their lives to prevent liver damage.
How old do you have to be to get tested for hepatitis C?
The CDC recommends testing for hepatitis C virus in all adults aged 18 years and older, as well as many other groups.
When was Epclusa approved?
Epclusa was first approved by the FDA in June of 2016. It is approved for use in adults and pediatric patients at least 3 years of age with chronic hepatitis C virus (HCV) genotype 1, 2, 3, 4, 5, or 6 infection. Epclusa is used with ribavirin in patients with advanced liver disease (decompensated cirrhosis).
What are the side effects of Epclusa?
The most common side effects of Epclusa in adults and children 6 years and older include headache and tiredness. When used with ribavirin in advanced liver disease in adults, common side effects also include anemia (not enough red blood cells), upset stomach (nausea), trouble sleeping, and diarrhea. In children less than 6 years old, vomiting and ...
Is Epclusa a ribavirin?
Epclusa is used with ribavirin in patients with advanced liver disease (decompensated cirrho sis). In August 2017, the FDA also approved Epclusa to treat chronic HCV in patients co-infected with HIV. Gilead Science's Epclusa is a nucleotide analog polymerase inhibitor and pan-genotypic NS5A inhibitor fixed-dose combination for the treatment ...
Does Epclusa cure HCV?
Official Answer. Yes, Epclusa ( sofosbuvir and velpatasvir) can cure hepatitis C virus (HCV) in many patients and has a 98% overall cure rate in all 6 of the main types of hepatitis C. "Cure” means the Hep C virus is not detected in the blood when measured three months after treatment is completed. In studies, these cure rates were seen in patients ...
