How long is the wait time for cancer treatment in Canada?
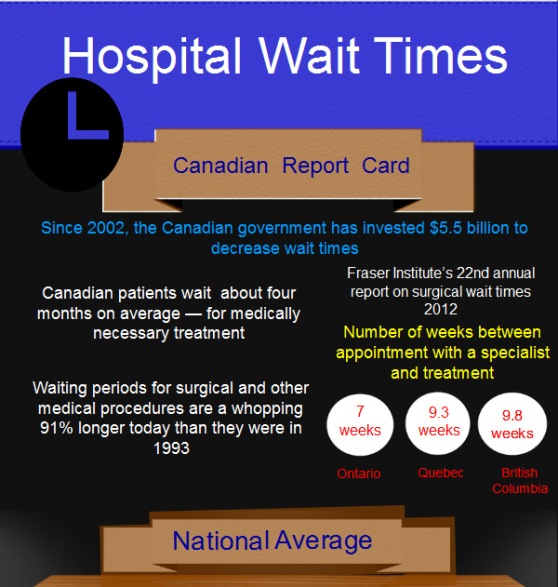
Dec 16, 2021 · The median wait time for treatment in Canada for the year 2021 was 25.6 weeks, up from 20.9 weeks wait time in 2019. Fraser Institute has been studying wait times across Canada by surveying specialist physicians across 12 specialties and 10 provinces since 1993.
How many Canadians are waiting for medical treatment this year?
Dec 15, 2021 · Ontario reports the shortest total wait—18.5 weeks—while Nova Scotia reports the longest—53.2 weeks. There is also a great deal of variation among specialties. Patients wait longest between a GP referral and neurosurgical procedures (49.2 weeks), while those waiting for radiation treatments begin treatment in 3.7 weeks.
Are wait times for specialist care in Canada getting worse?
Dec 10, 2020 · Ontario reports the shortest total wait—17.4 weeks—while Prince Edward Island reports the longest—46.5 weeks. There is also a great deal of variation among specialties. Patients wait longest between a GP referral and ophthalmic procedures (34.1 weeks), while those waiting for medical oncology begin treatment in 4.2 weeks.
How long does it take to get treatment in Ontario?
We recommend setting a maximum 6-month wait time benchmark for nonurgent referrals in Canada, 16, 31 a suggestion aligned with the Canadian Medical Protective Association’s recommendation. 17 However, we note that a 6-month wait time exceeds the 3-month period considered acceptable by patients. 5 – 8 Our results also show that, even if the observed …
How long do Canadians wait for treatment?
Do Canadians have to wait for medical treatment?
Why does Canada have such long wait times for healthcare?
How long are hospital wait times in Canada?
How long is the wait for an MRI in Canada?
How long does it take to be seen by a doctor in Canada?
Which country has the best healthcare?
Is Canadian health care good?
Why do surgeries take so long in Canada?
Is Canada's healthcare really free?
What's wrong with Canadian health care?
How long is the wait for medically necessary treatment?
Specialist physicians surveyed report a median waiting time of 22.6 weeks between referral from a general practitioner and receipt of treatment—longer than the wait of 20.9 weeks reported in 2019. This year’s wait time is the longest wait time recorded in this survey’s history and is 143% longer than in 1993, when it was just 9.3 weeks.
How many provinces are there in Canada for waiting for treatment?
In order to document the queues for visits to specialists and for diagnostic and surgical procedures in the country, the Fraser Institute has—for over two decades—surveyed specialist physicians across 12 specialties and 10 provinces.
How long does it take to get a CT scan in Canada?
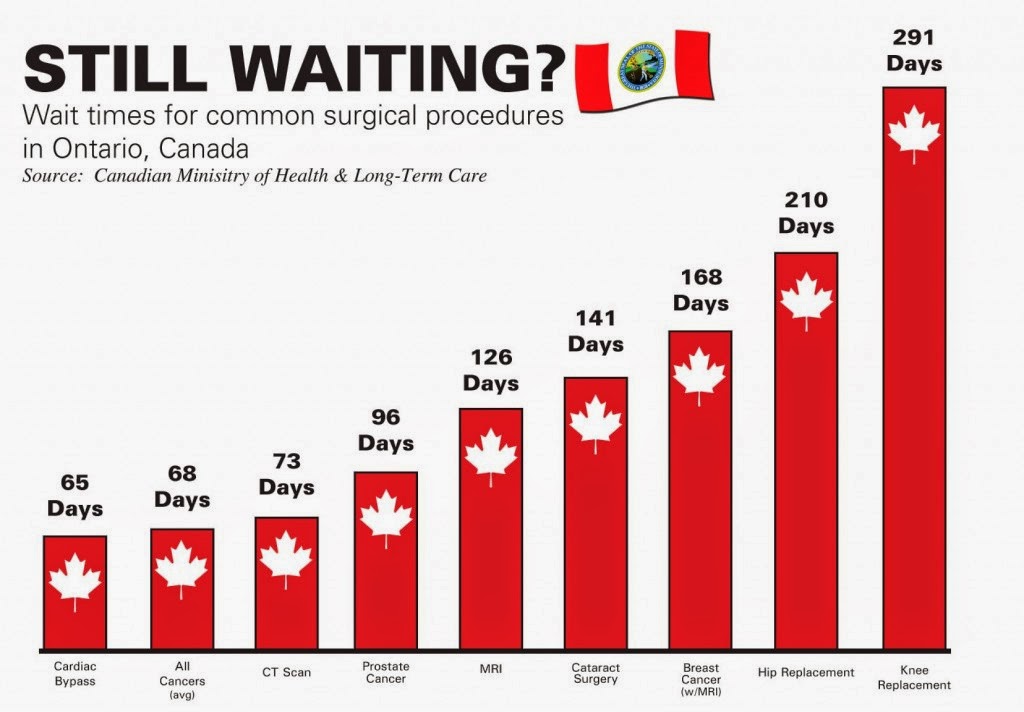
Patients also experience significant waiting times for various diagnostic technologies across the provinces. This year, Canadians could expect to wait 5.4 weeks for a computed tomography (CT) scan, 11.1 weeks for a magnetic resonance imaging (MRI) scan, and 3.5 weeks for an ultrasound.
How long is the wait for a specialist?
The waiting time in this segment increased from 10.8 weeks in 2019 to 12.1 weeks this year. This wait time is 116% longer than in 1993 when it was 5.6 weeks, and 4.3 weeks longer than what physicians consider to be clinically “reasonable” (7.8 weeks). The shortest specialist-to-treatment waits are found in Ontario (8.7 weeks), while the longest are in Nova Scotia (30.1 weeks).
How many people are waiting for treatment in Canada in 2020?
This means that, assuming that each person waits for only one procedure, 3.2% of Canadians are waiting for treatment in 2020. The proportion of the population waiting for treatment varies from a low of 1.97% in Quebec to a high of 9.97% in Nova Scotia. It is important to note that physicians report that only about 12.39% of their patients are on a waiting list because they requested a delay or postponement.
How many segments of wait time are there?
The total wait time that patients face can be examined in two consecutive segments.
Is waiting for medical treatment bad?
Research has repeatedly indicated that wait times for medically necessary treatment are not benign inconveniences. Wait times can, and do, have serious consequences such as increased pain, suffering, and mental anguish. In certain instances, they can also result in poorer medical outcomes—transforming potentially reversible illnesses or injuries into chronic, irreversible conditions, or even permanent disabilities. In many instances, patients may also have to forgo their wages while they wait for treatment, resulting in an economic cost to the individuals themselves and the economy in general.
What are the consequences of waiting for treatment in Canada?
These consequences may include poorer medical outcomes, increased or prolonged pain, and negative impacts on mental health. In dire circumstances, prolonged waits can even transform potentially curable illnesses and injuries into irreversible chronic conditions or permanent disabilities.
How long do you have to wait to get a CT scan in Alberta?
In Alberta, you’ll be waiting 7 weeks to receive a CT-Scan compared to Saskatchewan where you’ll only be waiting 2.5 weeks.
How is Canada's healthcare system broken up?
Still, the truth is that Canada’s healthcare system is broken up into pieces — one health plan per province and territory. With no federal healthcare system in place (that’s what national pharmacare might provide), Canadians in each province or territory have varying health plans, coverages, and access to practitioners.
Will the wait time for elective surgery increase in Canada?
Thousands of elective surgeries were postponed and as a result, wait times in Canada over the next few years are likely to increase even further as hospitals and doctors deal with their backlogs.
Why are there so long wait times for specialists in Canada?
Several factors have been identified as contributing to the excessive wait times for access to specialists in Canada, including limited specialty care resources, inconsistency in family physicians’ abilities to order advanced diagnostic tests, and higher demands on the health care system at large.18 Improved communication between providers and streamlining patient flow from primary to specialty care have been identified as critical requirements for improved access to specialty care in the Canadian Medical Association policy statement, which highlighted a few promising innovations as ones that “should be adopted throughout the country.”19These include the RACE (Rapid Access to Consultative Expertise) service, which allows primary care providers (PCPs) to reach specialists by telephone for urgent issues, and the Champlain BASE (Building Access to Specialists through eConsultation) eConsult Service, a secure online application connecting PCPs and specialists for nonurgent issues. Results from analyses of these services report prompt response time,20cost effectiveness,21and high levels of patient and provider satisfaction.22Building on this success, the RACE and BASE services have joined forces with the Canadian Foundation for Healthcare Improvement, the College of Family Physicians of Canada, Canada Health Infoway, and the Royal College of Physicians and Surgeons of Canada in the Access and Connected Medicine collaboratives, which culminated in a 15-month initiative supporting the launch of one or both services in 8 provinces and territories across Canada.23,24Part of this initiative included conducting a series of chart abstractions in clinics from participating regions to determine the wait time for medical specialist consultations.
How many clinics participated in the national wait time 1 study?
Distribution of the 22 clinics participating in the national wait time 1 study
How was data collected in the clinic?
Chart abstractors were trained through a webinar tutorial and given a chart abstraction manual prepared specifically for this project. Our research team monitored all data collection. The data collected included the date the referral was created, the characteristics of the referral, the date of the specialist appointment, whether there was communication between the specialist and the PCP, patient demographic data, and health care use during the waiting period. Data were collected in the clinic and uploaded to a secure server online.
How long does it take to get a specialist in Canada?
Long wait times have become a defining characteristic of the Canadian health care system. In 2016, the Commonwealth Fund ranked Canada last among 11 countries surveyed on wait times for specialist care.1Roughly one-fifth of Canadians report being negatively affected by wait times, citing experiences of stress, anxiety, pain, lost income, delays in diagnosis and treatment, duplications of tests, and deterioration in their conditions.2–4In general, patients consider 3 months to be the maximum acceptable wait time for a specialist appointment.5–8
How many primary care clinics are there in Canada?
A total of 22 primary care clinics across 7 provinces and 1 territory.
Does Canada have a long wait for health care?
Although Canada has made considerable investment s in its effort to address excessive wait times,9,10it has been argu ed that long wait times are the necessary price for its universal, publicly funded health care system .11Yet, Canada has been shown to spend more on health care than most high-income Organisation for Economic Co-operation and Development countries with universal health care systems,12and the Commonwealth Fund’s survey results show that other universal health care systems (eg, the Netherlands, Switzerland, Germany, Australia, and France) have much shorter wait times than Canada does.1What these countries do differently than Canada is they allow the private sector to provide core health care insurance and services, require patients to share in the cost of treatment, and fund hospitals based on activity (rather than the global budgets that are the norm in Canada).13In England and Scotland, a maximum wait of 18 weeks from referral by a general practitioner to start of specialty treatment for nonurgent conditions (including specialist consultations and diagnostic testing) is guaranteed in the English National Health Service Constitution.14The guarantee is monitored by the Department of Health and Social Care, and any breach of these targets results in reduction of up to 5% of revenue for the relevant specialty in the month in which the breach occurs. Other countries with publicly funded health care systems have initiated benchmarking as a policy tool. For example, Sweden suggests 60 days and New Zealand 6 months as the maximum acceptable length of time between referral and first specialist assessment.15In Canada, recommendations include a maximum 6-month wait time benchmark from a family doctor’s referral to the provision of any medically required service.16Nonetheless, conflicting measurement methodologies leave the process open to criticism.17The Canadian Medical Protective Association notes a lack of clarity as to “who is responsible for what,” resulting in a lack of comprehensive action to address the problem.17
Patient wait times guarantees
Find out about the defined time frame for patient wait times in Canada. Also learn about other options of care if you have to wait longer than the time frame.
10-Year Plan to Strengthen Health Care: Reducing Wait Times (2004)
Learn about the First Minister’s meeting on the future of health care. Access information on the 10-year plan to strengthen health care.
Canadian Institute for Health Information – wait times reporting
Access reports on wait times by the Canadian Institute for Health Information.
How long is the wait for medical care in 2020?
The annual survey noted that in 2020 the average wait time is now 22.6 weeks. The longest ever since 1993 when the national survey for medically necessary elective treatments began. That first year, average wait time was 9.3 weeks. Fraser Inst. Health care wait times survey 2020.
What are the consequences of waiting times?
The report itself notes, “Wait times can, and do, have serious consequences such as increased pain, suffering, and mental anguish. In certain instances, they can also result in poorer medical outcomes—transforming potentially reversible illnesses or injuries into chronic, irreversible conditions, or even permanent disabilities.
