Explore
The history of S. aureus treatment is marked by the development of resistance to each new class of antistaphylococcal antimicrobial drugs, including the penicillins, sulfonamides, tetracyclines, glycopeptides, and others, complicating therapy.
What are the treatment options for S aureus infection?
Despite the emergence of resistant and multidrug resistant S. aureus, five effective drugs for which little resistance has been observed are in clinical use: vancomycin, quinupristin-dalfopristin, linezolid, tigecycline, and daptomycin.
Why are US aureus isolates becoming more resistant?
This chapter reviews data on the treatment of infections caused by drug-resistant Staphylococcus aureus, particularly methicillin-resistant S. aureus (MRSA). This review covers findings reported in the English language medical literature up to January of 2013. Despite the emergence of resistant and …
What are the treatment options for methicillin-resistant Staphylococcus aureusbacteremia?
· There is no role for the use of linezolid, quinupristin-dalfopristin, tigecycline, or fluoroquinolones for treatment of S. aureus bacteremia. Linezolid has been found to be inferior compared to vancomycin in clinical trials.
What is the mechanism of resistance in Staphylococcus aureus?
· Vancomycin, a glycopeptide in clinical use for more than 50 years, still serves as the cornerstone of the treatment of drug-resistant Gram-positive infections. However, there are significant concerns owing to decreasing susceptibility to this agent among S. aureus. Furthermore, vancomycin is slowly bactericidal, which may be partly responsible for reported …
See more
Only approximately 20% of the strains remain sensitive to penicillin. Beta-lactamase stable penicillins such as flucloxacillin form the mainstay of treatment of staphylococcal infection. Meticillin-resistant S. aureus (MRSA) are resistant to all beta-lactam antibiotics. Glycopeptide antibiotics are effective against most MRSA strains but, in the last few years, isolates of MRSA …
How do you treat resistant Staphylococcus?
At home — Treatment of MRSA at home usually includes a 7- to 10-day course of an antibiotic (by mouth) such as trimethoprim-sulfamethoxazole (brand name: Bactrim), clindamycin, minocycline, linezolid, or doxycycline.
What is the most effective antibiotic against Staphylococcus aureus?
The antibiotics most effective against all S aureus cultures for outpatients were linezolid (100%), trimethoprim sulfamethoxazole (95%) and tetracyclines (94%). Linezolid (100%), trimethoprim sulfamethoxazole (100%) were most effective against MRSA isolates.
What is the best drug to treat Staphylococcus?
Linezolid is, to date, the best alternative in treating nosocomial pneumonia by methicillin-resistant Staphylococcus aureus. It is cost-effective; resistance levels are still very low but there are some concerns regarding its adverse events.
How can you reduce the risk of Staphylococcus aureus?
Keep your hands clean by washing them thoroughly with soap and water. Or use an alcohol-based hand sanitizer. Keep cuts and scrapes clean and covered with bandages until they heal. Avoid contact with other people's wounds or bandages.
How can Staphylococcus aureus be controlled?
A Staphylococcus aureus infection is usually treated with appropriate antimicrobial methods, such as removing the temporary medical devices (such as catheters) if possible, and therapeutic monitoring to stop bacterial growth as early as possible. Antibiotics may also be implemented.
What injection can cure Staphylococcus?
Such infections are often caused by bacteria called Staphylococci, and currently there are three antibiotic options used routinely....Ceftriaxone as Home IV for Staph Infections.Primary Purpose:TreatmentOfficial Title:Ceftriaxone as Home Intravenous Therapy for Deep-Seated Staphylococcal Infections, a Randomized Non-Inferiority Trial10 more rows•Oct 28, 2019
Can antibiotics cure Staphylococcus?
Staphylococcus aureus, the most common type of staph, is notorious for developing resistance to antibiotics. But luckily for those with staph infections, a number of antibiotics are still effective against it.
Can rifampicin cure Staphylococcus?
Abstract. Background: Rifampin has been used for the eradication of Staphylococcus aureus (S. aureus) colonization in various populations of healthy and sick people.
How can Staphylococcus be treated naturally?
Ginger and Manuka honey: A paste made of crushed ginger and salt in manuka honey is effective in treating a staph infection. It stops further bacterial growth and decreases infection. Apply it over the affected area 2-3 times a day to efficiently reduce the symptoms and speedy cure.
Is there a vaccine for Staphylococcus aureus?
There is no current vaccine to S. aureus infection. Studies in the past have relied on single antigen preparations, with current efforts weighted towards multiple antigens [10,11].
What herb can cure Staphylococcus?
Pineywoods geranium (Geranium caespitosum), rosemary (Rosmarinus officinalis), and bugle weed (Lycopus europaeus) all have inhibited antibiotic efflux pumps, thus reducing antibiotic resistance, in MRSA. Finally, garlic (Allium sativum) is recommended for patients with MRSA infections.
Can I get pregnant with Staphylococcus?
Some studies have suggested that a Staph infection might affect sperm and fertility. In general, exposures that fathers or sperm donors have are unlikely to increase the risk to a pregnancy.
What are the symptoms of Staphylococcus in a woman?
Skin: Most commonly, Staphylococcus aureus bacteria cause skin infection. This can produce boils, blisters, and redness on the skin. Breasts: Breastfeeding women can develop mastitis, which causes inflammation (swelling) and abscesses (collections of pus) in the breast.
Can ciprofloxacin cure Staphylococcus?
Ciprofloxacin appears to be safe and effective for a wide variety of clinical infections. In-vitro and animal studies point to high cure rates for both methicillin-sensitive and methicillin-resistant Staphylococcus aureus infections.
What is the MIC of Methicillin Resistant Staphylococcus Aureus?
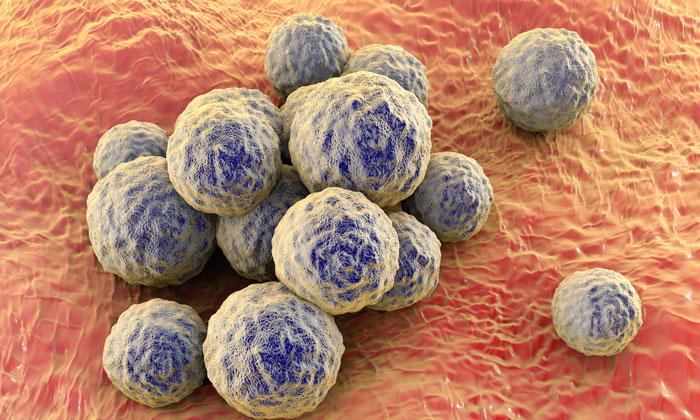
Methicillin Resistant Staphylococcus Aureus - StatPearls - NCBI Bookshelf. Based on the antibiotic susceptibilities, Methicillin resist ance in S. aureus is defined as an oxacillin minimum inhibitory concentration (MIC) of greater than or equal to 4 micrograms/mL. MRSA infection is one of the leading causes of hospital-acquired infections ...
What is the MIC of Methicillin in S. aureus?
Last Update: July 18, 2021. Continuing Education Activity. Based on the antibiotic susceptibilities, Methicillin resistance in S. aureus is defined as an oxacillin minimum inhibitory concentration (MIC) of greater than or equal to 4 micrograms/mL. MRSA infection is one of the leading causes of hospital-acquired infections ...
What is the etiology of methicillin resistance?
Etiology. Methicillin resistance has occurred in S. aureusby mutation of a penicillin-binding protein, a chromosome-encoded protein. This type of resistance is transferred between S. aureusorganisms by bacteriophages.
How does methicillin resistance occur?
Methicillin resistance has occurred in S. aureusby mutation of a penicillin-binding protein, a chromosome-encoded protein. This type of resistance is transferred between S. aureusorganisms by bacteriophages. This is one of the only medically relevant examples of chromosome-mediated drug resistance by phage transduction.
Can MRSA cause osteomyelitis?
MRSA can cause osteomyelitis of spine, long bones of upper and lower extremities by extension of local infection from a wound or as a part of hematogenous infection. Similarly, MRSA can cause septic arthritis of both native and prosthetic joints.
Can MRSA be confirmed with empiric antibiotics?
Confirmation of MRSA infection should not de lay treatment with empiric antibiotics against MRSA. Clinicians should send samples from suspected sources of infection for analysis including blood, sputum, urine, or wound scraping. [10][6][8] A positive Gram stain with cocci in clusters is suggestive of S. aureus.
How long does it take to treat MRSA?
The duration of therapy for treatment of MRSA SSTIs may range from 5 to 14 days depending on the extent of infection and response to treatment .
What is the best treatment for MRSA?
Vancomycin or daptomycin are the agents of choice for treatment of invasive MRSA infections [1]. Alternative agents that may be used for second-line or salvage therapy include telavancin, ceftaroline, and linezolid. Recent studies of treatment of MRSA bacteremia are reviewed. Vancomycin.
Is vancomycin good for MRSA?
Methicillin-resistant Staphylococcus aureus(MRSA) is a significant cause of health care-associated infections. Vancomycin remains an acceptable treatment option. There has been a welcome increase in the number of agents available for the treatment of MRSA infection.
Is MRSA a drug?
Methicillin- resistant Staphylococcus aureus(MRSA) is a common cause of serious nosocomial infections. Vancomycin, a glycopeptide in clinical use for more than 50 years, still serves as the cornerstone of the treatment of drug-resistant Gram-positive infections. However, there are significant concerns owing to decreasing susceptibility ...
Is Staphylococcus aureus resistant to penicillin?
Beta-lactamase stable penicillins such as flucloxacillin form the mainstay of treatment of staphylococcal infection. Meticillin-resistant S. aureus (MRSA) are resistant to all beta-lactam antibiotics.
Is MRSA resistant to beta-lactam?
Metici llin-resistant S. aureus (MRSA) are resistant to all beta-lactam antibiotics. Glycopeptide antibiotics are effective against most MRSA strains but, in the last few years, isolates of MRSA that have reduced susceptibility to glycopeptides (glycopeptide-intermediate S. aureus) have been isolated. Some strains exhibit frank resistance ...
Can glycopeptides be used for MRSA?
Glycopeptide antibiotics are effective against most MRSA strains but, in the last few years, isolates of MRSA that have reduced susceptibility to glycopeptides (glycopeptide-intermediate S. aureus) have been isolated. Some strains exhibit frank resistance to glycopeptides (vancomycin-resistant S. aureus). Infections due to these strains are ...
Why is staph infection so hard to treat?
Methicillin-resistant Staphylococcus aureus (MRSA) is a cause of staph infection that is difficult to treat because of resistance to some antibiotics. Staph infections—including those caused by MRSA—can spread in hospitals, other healthcare facilities, and in the community where you live, work, and go to school.
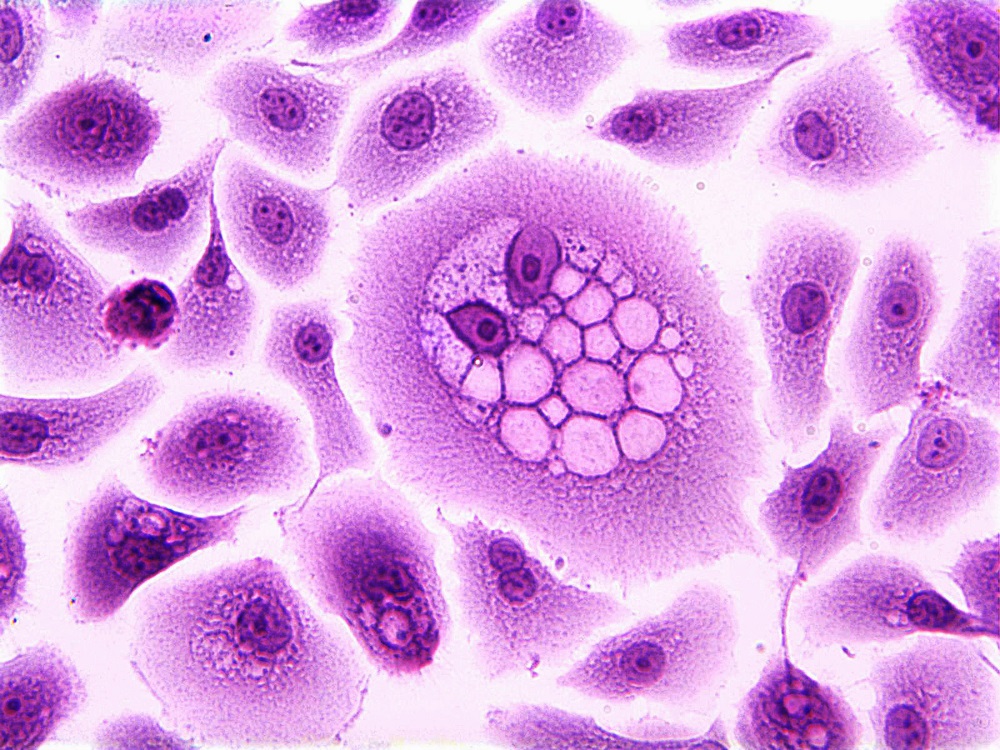
What is a staph?
minus. Related Pages. Staphylococcus aureus (staph) is a type of bacteria found on people’s skin. Staph bacteria are usually harmless, but they can cause serious infections that can lead to sepsis or death.
What is the best treatment for methicillin resistant S aureus?
Some experts recommend combination therapy with a penicillinase-resistant penicillin or cephalosporin (in case the organism is methicillin-sensitive S aureus [MSSA]) [ 8] and clindamycin or a quinolone. Others suggest use of clindamycin, trimethoprim-sulfamethoxazole (TMP-SMX), rifampin, doxycycline, or a quinolone.
What antibiotics are used for osteomyelitis?
Empirically, initiating a semisynthetic penicillin (eg, oxacillin [150 mg/kg/d]) and clindamycin (30-40 mg/kg/d) is a good choice for most cases of community-acquired osteomyelitis. In patients with allergy to penicillin, a first-generation cephalosporin and clindamycin (30-40 mg/kg/d) are an excellent alternative. Use vancomycin or linezolid when the other drugs mentioned are absolutely not tolerated or when resistance or the clinical course dictates. The duration of therapy is a controversial topic in the literature, but the consensus among multiple authors is that the minimum effective treatment time is 4-6 weeks. A switch to oral therapy is acceptable if the child is able to take oral antibiotics, is afebrile, and if he or she has demonstrated a good clinical response to parenteral antibiotics. [ 13]
How long does antistaphylococcal therapy last?
These antibiotics readily reach joint fluid, and the concentration in the joint fluid is 30% of the serum value. Therapy usually continues for at least 4 weeks. Duration of parenteral therapy is often debated. Some authors have demonstrated efficacy with 1 week of parenteral therapy followed with 3 weeks of oral therapy. Consider a switch to oral therapy based on the considerations mentioned above. Joint fluid that reaccumulates should be removed, and a sample should be cultured to assess the efficacy of therapy and to make the patient more comfortable.
Why is S. aureusis a pathogen?
aureusis perhaps the pathogen of greatest concern because of its intrinsic virulence, its ability to cause a diverse array of life-threatening infections, and its capacity to adapt to different environmental conditions (4, 5).
What antimicrobial agents are tested for sensitivity?
Isolates were tested for sensitivity to the following antimicrobial agents: gentamicin, tobramycin, amikacin, ciprofloxacin, clindamycin, erythromycin, chloramphenicol, trimethoprim-sulfamethoxazole, and vancomycin. Some hospitals did not test for all of the antibiotics.
When did doctors abandon their belief that all bacterial infections were treatable?
In the early 1970s, physicians were finally forced to abandon their belief that, given the vast array of effective antimicrobial agents, virtually all bacterial infections were treatable. Their optimism was shaken by the emergence of resistance to multiple antibiotics among such pathogens as Staphylococcus aureus, Streptococcus pneumoniae, ...
When did penicillin become resistant to staphylococci?
However, as early as 1942, penicillin-resistant staphylococci were recognized, first in hospitals and subsequently in the community (12). By the late 1960s, more than 80% of both community- and hospital-acquired staphylococcal isolates were resistant to penicillin.
Which subunit of topoisomerase is the most common site of resistance mutation?
The ParC sub unit (GrlA in S. aureus) of topoisomerase IV and the GyrA subunit in gyrase are the most common sites of resistance mutations; topoisomerase IV mutations are the most critical, since they are the primary drug targets in staphylococci (58, 60).
Is vancomycin used for staphylococcus?
The dramatic increase in use of vancomycin to treat infections caused by methicillin-resistant staphylococci (both coagulase-positive and -negative), Clostridium difficile, and enterococcal infections preceded the emergence of vancomycin-resistant staphylococci (65).
Can quinolones be used to treat bacterial infections?
When quinolones are used to treat infections caused by other bacterial pathogens, subjects colonized with S. aureus(e.g., on their skin or mucosal surfaces) are likely exposed to subtherapeutic antibiotic concentrations and are therefore at risk of becoming colonized with resistant mutants (58).
Is Staphylococcus aureus adaptive?
Abstract. Staphylococcus aureus can exemplify better than any other human pathogen the adaptive evolution of bacteria in the antibiotic era, as it has demonstrated a unique ability to quickly respond to each new antibiotic with the development of a resistance mechanism, starting with penicillin and methicillin, until the most recent, ...
What is the adaptive evolution of Staphylococcus aureus?
Staphylococcus aureus can exemplify better than any other human pathogen the adaptive evolution of bacteria in the antibiotic era, as it has demonstrated a unique ability to quickly respond to each new antibiotic with the development of a resistance mechanism, starting with penicillin and methicillin, until the most recent, linezolid and daptomycin. Resistance mechanisms include enzymatic inactivation of the antibiotic (penicillinase and aminoglycoside-modification enzymes), alteration of the target with decreased affinity for the antibiotic (notable examples being penicillin-binding protein 2a of methicillin-resistant S. aureus and D-Ala-D-Lac of peptidoglycan precursors of vancomycin-resistant strains), trapping of the antibiotic (for vancomycin and possibly daptomycin) and efflux pumps (fluoroquinolones and tetracycline). Complex genetic arrays (staphylococcal chromosomal cassette mec elements or the vanA operon) have been acquired by S. aureus through horizontal gene transfer, while resistance to other antibiotics, including some of the most recent ones (e.g., fluoroquinolones, linezolid and daptomycin) have developed through spontaneous mutations and positive selection. Detection of the resistance mechanisms and their genetic basis is an important support to antibiotic susceptibility surveillance in S. aureus.
