What is the difference between XDR and MDR?
1. Garlic...
2. Bananas...
3. Drumstick...
4. Indian Gooseberry...
5. Oranges...
6. Custard Apple...
7. Black Pepper...
8. Walnuts...
Learn More...Can TB return after treatment?
How is TB spread?
- Shaking someone’s hand
- Sharing food or drink
- Touching bed linens or toilet seats
- Sharing toothbrushes
- Kissing
What is the treatment for drug resistant TB?
The treatment regimen is a lengthy one, but if you stick with it and take medications the way you should, you can beat the disease. Even with treatment, however, tuberculosis reinfection is becoming a problem. It's very common for people with tuberculosis to relapse during treatment.
Does tuberculosis ever go away?
Tuberculosis
- Diagnosis. During the physical exam, your doctor will check your lymph nodes for swelling and use a stethoscope to listen to the sounds your lungs make when you breathe.
- Treatment. ...
- Clinical trials. ...
- Coping and support. ...
- Preparing for your appointment. ...
Can XDR-TB be cured completely?
Can XDR TB be treated and cured? Yes, in some cases. Some TB control programs have shown that cure is possible for an estimated 30% to 50% of affected people.
How long is treatment for XDR-TB?
MDR- and XDR-TB need prolonged treatment duration, from 18 to 24 months after sputum culture conversion, as recommended by the World Health Organization (WHO) [2]. A prolonged duration of treatment may lead to poor adherence, higher cost and undue toxicity.
Are there new treatments on the horizon for XDR-TB?
Newly developed drugs such as Bdq and Dlm provide new treatment options for MDR/XDR-TB. If trials are successful, treatment for MDR/XDR-TB could be reduced to 6–9 months as standard. By 2022 best practice for managing MDR/XDR-TB will be informed by substantial clinical trial data.
Who is at risk of XDR-TB?
How do people get XDR-TB? People may get XDR-TB in one of two ways. It may develop in a patient who is receiving treatment for active TB, when anti-TB drugs are misused or mismanaged, and is usually a sign of inadequate clinical care or drug management.
What is XDR infection?
Extensively drug-resistant tuberculosis (XDR-TB) is a form of tuberculosis caused by bacteria that are resistant to some of the most effective anti-TB drugs. XDR-TB strains have arisen after the mismanagement of individuals with multidrug-resistant TB (MDR-TB).
What causes XDR-TB?
Extensively drug-resistant (XDR) TB refers to MDR-TB strains that are resistant to fluoroquinolones and second-line injectable drugs. The main causes of the spread of resistant TB are weak medical systems, amplification of resistance patterns through incorrect treatment, and transmission in communities and facilities.
What is the latest treatment for TB?
The usual treatment is: 2 antibiotics (isoniazid and rifampicin) for 6 months. 2 additional antibiotics (pyrazinamide and ethambutol) for the first 2 months of the 6-month treatment period.
Which is the best tablet for TB?
The most common medications used to treat tuberculosis include:Isoniazid.Rifampin (Rifadin, Rimactane)Ethambutol (Myambutol)Pyrazinamide.
What is the difference between XDR and MDR tuberculosis?
Multidrug-resistant tuberculosis (MDR-TB) is practically incurable by standard first-line treatment. However, extensively drug-resistant tuberculosis (XDR-TB) is resistant to both first- and second-line drugs due to drug misuse and mismanagement. Therefore, XDR-TB treatment becomes even harder.
What is pre XDR-TB?
Pre-XDR TB: caused by an organism that is resistant to isoniazid, rifampin, and a fluroquinolone OR by an organism that is resistant to isoniazid, rifampin, and a second-line injectable (amikacin, capreomycin, and kanamycin)
Can drug-resistant TB cured?
In most cases, TB is treatable and curable; however, people with TB can die if they do not get proper treatment. Sometimes drug-resistant TB occurs when bacteria become resistant to the drugs used to treat TB. This means that the drug can no longer kill the TB bacteria.
How do you know if TB treatment is working?
After taking TB medicine for several weeks, a doctor will be able to tell TB patients when they are no longer able to spread TB germs to others. Most people with TB disease will need to take TB medicine for at least 6 months to be cured.
What Is Extensively Drug-Resistant Tuberculosis (XDR TB)?
Extensively drug-resistant TB (XDR TB) is a rare type of multidrug-resistant tuberculosis (MDR TB) that is resistant to isoniazid and rifampin, plu...
Why Is XDR TB So Serious?
Because XDR TB is resistant to the most potent TB drugs, the remaining treatment options are less effective, have more side effects, and are more e...
Who Is at Risk For Getting XDR TB?
Drug-resistant TB (MDR or XDR) is more common in people who: 1. Do not take their TB medicine regularly 2. Do not take all of their TB medicines as...
How Can I Prevent Myself from Getting TB?
Avoid close contact for a prolonged period of time with known TB patients in crowded, enclosed environments like clinics, hospitals, prisons, or ho...
Can The TB Vaccine (BCG) Help Prevent XDR TB?
The TB vaccine is called Bacille Calmette-Guérin (BCG)(https://www.cdc.gov/tb/publications/factsheets/prevention/bcg.htm), and it is used in many c...
If I Have Drug-Susceptible Tb, How Can I Prevent Getting Drug-Resistant TB?
The most important thing is for you to continue taking all your TB medicines exactly as prescribed. No doses should be missed and treatment should...
Can XDR TB Be Treated and Cured?
Yes, in some cases. Some TB control programs have shown that cure is possible for an estimated 30% to 50% of affected people. Successful outcomes d...
What Are The Symptoms of XDR TB?
The general symptoms of TB disease include feelings of sickness or weakness, weight loss, fever, and night sweats. The symptoms of TB disease of th...
What Should I Do If I Have been Around Someone Who Has XDR TB?
If you think you have been exposed to someone with XDR TB disease, you should contact your doctor or local health department about getting a TB ski...
How Long Does It Take to Find Out If You Have XDR TB?
If TB bacteria are found in the sputum (phlegm), the diagnosis of TB can be made in a day or two, but this finding will not be able to distinguish...
How long does XDR-TB treatment last?
Extension of therapy to 24 months is the suggested minimum length of treatment for XDR-TB.
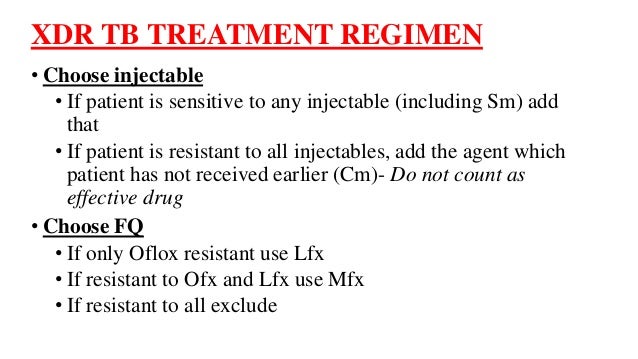
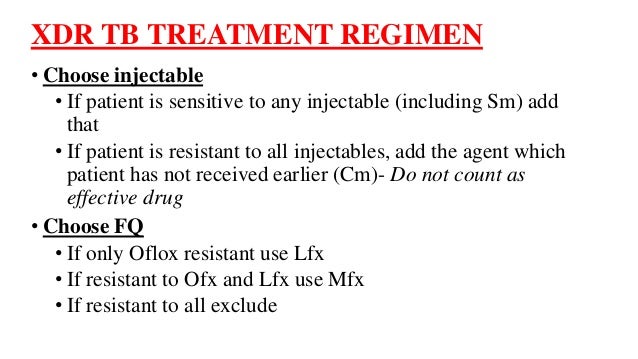
How long to use injectables?
1 - Consider a longer duration of use for the injectable agent (12 months or possibly the whole treatment). If the patient’s strain is resistant to all injectable agents, use one the patient has never used before 1 . 2 - Use a third-generation fluoroquinolone such as moxifloxacin.
Is XDR TB more difficult to treat than MDR TB?
XDR-TB is much more difficult to treat than other MDR-TB and extremely difficult to treat in HIV-infected patients 33, 34. While reports of HIV-infected patients being promptly diagnosed with XDR-TB and placed on adequate regimen are non-existent to date, a few reports of cohorts of HIV-negative patients have been shown to have cure rates ...
Is DST good for TB?
While the reproducibility and reliability of DST to injectables is good , there is little data on clinical relevance of the test. Options with XDR-TB are very limited and some strains may be affected in vivo by an injectable agent even though they are testing resistant in vitro.
Which group of drugs is the most effective in treating TB?
Group 3: Fluoroquinolones. Fluoroquinolones are often the most effective anti-TB drugs in an MDR-TB regimen. There are two important recommendations regarding fluoroquinolone use from the 2011 update of the Guidelines for the programmatic management of drug-resistant tuberculosis(1).
What is chapter 6 of the TB treatment guide?
This chapter provides guidance on the strategies for the treatment of multidrug- and extensively drug-resistant TB (M/XDR-TB), with emphasis on regimen design. The treatment of mono- and poly-drug-resistant TB is addressed in Chapter 6. The strategies described in this chapter are largely based on the recommendations from the 2011 update of Guidelines for the programmatic management of drug-resistant tuberculosis, which underwent systematic review and analysis of the evidence for best treatment practice (1).
What is empiric TB?
This Handbook uses the term “empiric” to refer to the initiation of treatment prior to determination of a firm diagnosis of drug-resistant TB. Empiric regimens can be used for both standardized and individualized treatment strategies. For example, an empiric XDR regimen refers to the use of a regimen designed to treat XDR-TB before the diagnosis of XDR-TB is made.
What is the best group of anti-TB drugs?
Group 1: First-line oral agents. Group 1 anti-TB drugs, the most potent and best tolerated, should be used if there is good laboratory evidence andclinical history that suggests that a drug from this group is effective. For patients with strains resistant to low concentrations of isoniazid but susceptible to higher concentrations, the use of high-dose isoniazid may have some benefit (when isoniazid is used in this manner it is considered a Group 5 drug, see below). The newer rifamycins, such as rifabutin, have very high cross-resistance to rifampicin.
What are the different classes of anti-TB drugs?
The classes of anti-TB drugs have traditionally been divided into first- and second-line anti-T B drugs with isoniazid, rifampicin, pyrazinamide, ethambutol and streptomycin being the primary first-line anti-TB drugs. While this classification is used in this document, it also uses a system that classifies the drugs into five different groups. The five-group system is based on efficacy, experience of use, safety and drug class. WHO will be reviewing this five-group system in the next update of the guidelines for the management of MDR-TB in view of the new drugs being introduced and the emerging evidence on its safety and efficacy. The different groups are shown in Table 5.1. Not all drugs in the same group come from the same “drug class” or have the same efficacy or safety. For more information, see individual descriptions of each group in this section. Individual detailed drug information for all anti-TB drugs is provided in the drug information sheets of Part 3.
What is standardized treatment?
Standardized treatment:DRS data from representative patient populations are used to base regimen design in the absence of individual DST. All patients in a defined group or category receive the same regimen (see Chapter 4for risk groups for MDR-TB). Suspected MDR-TB should be confirmed by DST whenever possible.
How early can you start anti-TB treatment?
Antiretroviral therapy (ART) is recommended for all patients with HIV and drug-resistant TB, irrespective of CD4 cell-count, as early as possible (within the first eight weeks) following initiation of the anti-TB treatment (strong recommendation) (1). The drug dosage is usually determined by age and weight.
What is XDR TB?
XDR TB is strains of TB that are resistant to rifampicin and isoniazid. They are also resistant to a fluoroquinolone and to at least one of the three injectable TB drugs, capreomycin, kanamycin and amikacin. 1“Extensively drug-resistant tuberculosis (XDR-TB): recommendations for prevention and control”, Weekly epidemiological record, WHO, Geneva, ...
What is the difference between MDR TB and XDR TB?
MDR TB is strains of TB that are resistant to rifampicin and isoniazid.
What is XDR in medicine?
XDR was defined, and was a helpful definition, when people with drug resistant TB were being treated with injectable drugs. But the injectable drugs are no longer recommended by the World Health Organisation (WHO), and WHO accepts that a new definition is needed.
What is the primary driver of the XDR TB epidemic in South Africa?
A study in KwaZulu-Natal which evaluated the social networks as well as clinical data from people with XDR TB concluded that transmission , in both hospitals and households, had been the primary driver of the XDR TB epidemic in the province. 4Auld, S, “South Africa’s XDR-TB epidemic is due to transmission rather then evolution of resistant strains”, CROI, March 2016, www.aidsmap.com This confirms what it is believed happened when the outbreak occurred earlier at Tugela Ferry.
What was the treatment for XDR in Peru?
In Peru care was provided to patients with XDR who were not infected with HIV. However they had received numerous previously unsuccessful anti TB treatments. The TB treatment they were provided with was aggressive, with the patients being given many drugs, at the highest doses they could tolerate.
How many people survived XDR?
Of the 53 patients with XDR TB diagnosed during the first year of surveillance only one survived. The average survival rate from time of diagnosis was just 16 days among the 42 patients with confirmed dates of death. More than half the patients with XDR TB had never been previously treated for TB. An additional third had either been cured or had completed treatment for previous TB illness.
Why are there no cases of TB in South Africa?
It is however believed that many cases are never diagnosed due to a lack of laboratory capacity to test for resistance to second line drugs. Many people may also die from what is thought to be multi drug resistant TB. It may be believed that they were not taking their drugs ...
What is XDR TB?
Extensively drug-resistant tuberculosis (XDR TB) is a relatively rare type of multidrug-resistant tuberculosis (MDR TB ). It is resistant to almost all drugs used to treat TB, including the two best first-line drugs: isoniazid and rifampin. XDR TB is also resistant to the best second-line medications: fluoroquinolones and at least one of three injectable drugs (i.e., amikacin, kanamycin, or capreomycin).
What should I do if I have been around someone who has XDR TB?
If you think you have been exposed to someone with TB disease, you should contact your doctor or local health department about getting a TB skin test or the QuantiFERON®-TB Gold test (QFT-G), a blood test. And tell the doctor or nurse when you spent time with this person.
How is XDR TB spread?
Drug-susceptible (regular) TB and XDR TB are spread the same way. TB germs are put into the air when a person with TB disease of the lungs or throat coughs, sneezes, speaks, or sings. These germs can float in the air for several hours, depending on the environment. Persons who breathe in the air containing these TB germs can become infected.
Why is XDR TB so serious?
Because XDR TB is resistant to the most powerful first-line and second-line drugs, patients are left with treatment options that are much less effective and often have worse treatment outcomes . XDR TB is of special concern for persons with HIV infection or other conditions that can weaken the immune system. These persons are more likely to develop TB disease once they are infected, and also have a higher risk of death once they develop TB disease.
How can I prevent myself from getting TB?
Avoid close contact or prolonged time with known TB patients in crowded, enclosed environments like clinics, hospitals, prisons, or homeless shelters.
How long does it take to find out if you have XDR TB?
Final diagnosis for TB, and especially for XDR TB, may take from 6 to 16 weeks.
How many cases of XDR TB have been reported in the United States?
In the United States, 49 cases of XDR TB have been reported between 1993 and 2006.
What is XDR TB?
The definition of extensively drug-resistant tuberculosis (XDR-TB) has been revised by the World Health Organization (WHO)’s Global TB Programme, who have also defined pre-XDR-TB for the first time, highlighting the seriousness of these forms of TB.
How many people die from TB in a year?
About 470,000 people fall ill with MDR/RR-TB and about 180,000 die from this form of TB each year, according to WHO estimates. Globally, in 105 countries with representative data, 20% of the people with MDR/RR-TB also have resistance to another potent drug for the treatment of drug-resistant TB – a fluoroquinolone. Extensively drug resistant TB is a more serious form of MDR-TB, with poorer treatment outcomes reported for those affected by this condition.
Is drug resistant TB a serious disease?
They may also stimulate the development of better treatment regimens for these dangerous forms of TB disease. “Drug resistant TB is a serious clinical condition and remains a global public health concern. The new definitions will enable access to more effective treatment options for patients with drug resistant TB.
Why is XDR TB so resistant to TB drugs?
Because XDR TB is resistant to the most potent TB drugs, patients are left with treatment options that are much less effective. XDR TB is of special concern for persons with HIV infection or other conditions that can weaken the immune system.
How to prevent MDR TB?
Another way to prevent getting MDR TB is to avoid exposure to known MDR TB patients in closed or crowded places such as hospitals, prisons, or homeless shelters. If you work in hospitals or health-care settings where TB patients are likely to be seen, you should consult infection control or occupational health experts.
What is MDR TB?
What is multidrug-resistant tuberculosis (MDR TB)? Multidrug-resistant TB (MDR TB) is caused by an organism that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. These drugs are used to treat all persons with TB disease.
What are the symptoms of TB in the lungs?
The symptoms of TB disease of the lungs may also include coughing, chest pain, and coughing up blood. Symptoms of TB disease in other parts of the body depend on the area affected. If you have these symptoms, you should contact your doctor or local health department.
What to do if you think you have been exposed to someone with TB?
If you think you have been exposed to someone with TB disease, you should contact your doctor or local health department about getting a TB skin test or TB blood test. And tell the doctor or nurse when you spent time with this person.
How is TB spread?
Drug-susceptible TB and drug-resistant TB are spread the same way. TB bacteria are put into the air when a person with TB disease of the lungs or throat coughs, sneezes, speaks, or sings. These bacteria can float in the air for several hours, depending on the environment. Persons who breathe in the air containing these TB bacteria can become infected.
What is resistance to anti-TB drugs?
Resistance to anti-TB drugs can occur when these drugs are misused or mismanaged. Examples include when patients do not complete their full course of treatment; when health-care providers prescribe the wrong treatment, the wrong dose, or length of time for taking the drugs; when the supply of drugs is not always available; or when the drugs are of poor quality.