
What causes increased or decreased eosinophils?
- Whistling chest
- Thoracic oppression
- Cough
How to treat eosinophilic esophagitis naturally?
- eating whole organic foods
- making meals from scratch**
- Trying to eat well-balanced meals with lots of veggies
- Diffusing Essential oils to uplift my moods
When should high eosinophils be evaluated?
Sometimes such investigation is urgent (e.g., in cardiac failure or if the eosinophil count is extremely high). History The medical history of a patient with eosinophilia should first evaluate the presenting complaint, followed by a systematic review.
How can I reduce my eosinophil count?
- Boil a bowl of water, put a little eucalyptus oil in it. ...
- Drinking tea with some ginger juice or crushed ginger can be helpful in curing this problem.
- Mix some honey and pepper powder in water, and consume it twice a day to boost your immunity.
- Adding ½ tsp of turmeric powder in a glass of milk can be a valuable remedy to reduce high eosinophil count.
What is the best medicine for eosinophilia?
The most common medications associated with eosinophilia include antibiotics (penicillin, cephalosporins), non-steroidal anti-inflammatory medications (aspirin, ibuprofen), phenytoin (anti-seizure) and allopurinol (used to treat gout).
How do you clear eosinophilia?
Proton pump inhibitors (PPIs) can help control the amount of acid in your stomach and esophagus. They're used to treat acid reflux. Taking a PPI could decrease the number of eosinophils found in your esophagus and help bring down the inflammation.
What is the reason for eosinophilia?
Parasitic diseases and allergic reactions to medication are among the more common causes of eosinophilia. Hypereosinophila that causes organ damage is called hypereosinophilic syndrome. This syndrome tends to have an unknown cause or results from certain types of cancer, such as bone marrow or lymph node cancer.
Is eosinophilia serious?
Is eosinophilia serious? Depending on your eosinophil count, eosinophilia can be mild, moderate or severe. High eosinophil levels can indicate a mild condition such as a drug reaction or allergy, or a severe condition could cause it, including some blood disorders.
Can eosinophilia go away by itself?
Generally, no specific therapy is required as symptoms usually go away spontaneously without treatment. Simple pulmonary eosinophilia was first described in the medical literature in 1932. It is classified as a form of eosinophilic lung disease.
What is the symptoms of eosinophilia?
SymptomsDifficulty swallowing (dysphagia)Food getting stuck in the esophagus after swallowing (impaction)Chest pain that is often centrally located and does not respond to antacids.Backflow of undigested food (regurgitation)
What medications cause high eosinophils?
Asymptomatic eosinophilia has been associated most often with quinine, penicillins, cephalosporins, or quinolones. Pulmonary infiltrates with peripheral eosinophilia have been particularly associated with NSAIDs, sulfas, and nitrofurantoin.
How to treat eosinophilia?
Similar to what diagnostic tests may be needed, treatment is determined by the cause of eosinophilia. 1 Options include: 1 Observation: If your eosinophilia is mild, observation with repeat labs may be recommended. 2 If a medication is causing your elevated eosinophil count, it may be discontinued 3 Maximizing therapy for asthma, eczema, and allergies 4 Parasite infections are treated with anti-parasitic medications. 5 Steroids such as prednisone may be used to treat hypereosinophilic syndromes
What are the symptoms of eosinophilia?
If your eosinophil count is mildly elevated you may not have any symptoms. 1 Common symptoms include: Rash. Itching.
How many cells are in eosinophils?
Eosinophilia can be categorized by the number of eosinophils (absolute eosinophil count). 1 . Mild: 500 - 1500 cells/mL. Moderate: 1500 - 5000 cells/mL. Severe: > 5000 cells/mL. Determining the cause of your eosinophilia will be based on your symptoms.
What is the technical name for an increased eosinophil count?
Treatment. Eosinophilia is the technical name for an increased eosinophil count. Eosinophils are a type of white blood cells that destroy substances in the body like parasites and participate in allergic reactions. Verywell / Laura Porter.
Why is my eosinophil count elevated?
Causes. There are numerous reasons your eosinophil count may be elevated. Some of the causes are benign and require little treatment. It is not uncommon for the elevated count to be transient and resolve without treatment. Let's review some of the causes now. Parasite infections: Worldwide the most common cause of eosinophilia is ...
What percentage of people with EoE have elevated eosinophils?
About 50% of people with EoE will also have elevated eosinophil counts in the blood. 4 . Hypereosinophilic Syndromes: Hypereosinophilic syndromes (HES) are a group of disorders characterized by very high eosinophil counts and evidence of organ damage from a large number of eosinophils.
What is eosinophilia on CBC?
Eosinophils are one of the white blood cells and are found in the portion of the CBC called the differential . The differential reports how many of each type of white blood cells (neutrophil, lymphocyte, monocyte, eosinophil, and basophil) are present in the blood.
What is the goal of eosinophilic asthma?
The goal of treatment is to improve and control your asthma symptoms. Depending on your condition, ...
What is an eosinophil count?
What’s an Eosinophil Count? A Diagnosis and Questions for Your Doctor. Inhalers and Other Treatments. Take Care of Yourself. Because it's a rare condition, nailing down a diagnosis for eosinophilic asthma can take time. But once doctors reach a conclusion, they turn to treatments specifically focused on this kind of asthma.
Can you take corticosteroid pills with eosinophilic asthma?
But the inhaled versions may not work well in eosinophilic asthma, so you may need to take corticosteroid pills.
What is eosinophilia?
Eosinophilia: a pragmatic approach to diagnosis and treatment. Eosinophilia is associated with a wide variety of allergic, rheumatologic, infectious, neoplastic, and rare idiopathic disorders. Clinical manifestations range from benign asymptomatic presentations to life-threatening complications, including endomyocardial fibrosis and thromboembolism.
Is eosinophilia a prognosis?
The prognosis and choice of treatment depend not only on the degree of eosinophilia and severity of organ involvement, but also on the etiology of the eosinophilia. Unfortunately, despite recent advances in molecular and immunologic techniques, the etiology remains unproven in the overwhelming majority of cases.
Is eosinophilia a rheumatoid?
Eosinophilia is associated with a wide variety of allergic, rheumatologic, infectious, neoplastic, and rare idiopathic disorders. Clinical manifestations range from benign asymptomatic presentations to life-threatening complications, including endomyocardial fibrosis and thromboembolism.
What is the procedure to check for swelling in the esophagus?
Upper endoscopy. Your doctor will use a long narrow tube (endoscope) containing a light and tiny camera and insert it through your mouth down the esophagus. The doctor will inspect the lining of your esophagus for inflammation and swelling, horizontal rings, vertical furrows, narrowing (strictures), and white spots.
Why do doctors dilate the esophagus?
If you experience severe narrowing (strictures) of your esophagus, your doctor may recommend dilation (stretching) to help make swallowing easier. Dilation may be used if steroids are not helpful. Or dilation may be a choice to avoid ongoing use of medication.
What is the camera on the end of an endoscope?
A tiny camera on the end of the endoscope lets your doctor examine your esophagus, stomach and the beginning of your small intestine (duodenum). Your doctor will consider both your symptoms and test results to diagnose eosinophilic esophagitis. This will include determining whether you have gastroesophageal reflux disease (GERD).
What to do if you don't respond to PPI?
Topical steroid. If you do not respond to the PPI, your doctor will then likely prescribe a topical steroid, such as fluticasone or budesonide, which is a liquid that is swallowed to treat eosinophilic esophagitis.
How does an esophageal sponge test work?
Esophageal sponge. This test is performed in the doctor's office and involves swallowing a capsule attached to a string. The capsule will dissolve in your stomach and release a sponge that the doctor will pull out your mouth with the string.
Can eosinophilic esophagitis be detected by biopsy?
Some people with eosinophilic esophagitis will have an esophagus that looks normal. Biopsy. During an endoscopy, your doctor will perform a biopsy of your esophagus. A biopsy involves taking a small bit of tissue. Your doctor will likely take multiple samples from your esophagus and then examine the tissue under a microscope for eosinophils.
What is eosinophilia?
Eosinophilia, defined as peripheral blood eosinophil counts greater than 500 per microliter , may vary from mild-severe. Idiopathic hypereosinophilic syndrome has been identified as an unusual cause of moderate to severe eosinophilia. Progress in treatment of this condition has accompanied greater understanding about the basic biology of eosinophils.
What is the most common cause of eosinophilia?
By far the most common source of moderate to severe eosinophilia involves infectious diseases such as malaria, pseudomonas, borrelia infection including lyme disease and tissue infection with helm inthic infestations including schistosomiasis Fungal infection can also be associated with severe eosinophilia.
Where are eosinophils found?
Once these cytokines activate bone marrow precursors, the eosinophils can be found in a variety of tissues in participants, in either host defense or tissue remodeling in response to cell damage. This defines the potential for the pathogenesis of allergic response associated with hypereosinophilia.2,3.
Can eosinophilia cause cancer?
Many infectious causes can cause secondary eosinophilia that can be of the moderate to severe level. In addition, a variety of diseases including most prominently allergic disorders, drug allergy, autoimmune diseases, endocrine disorders such as Addison’s disease, and many different cancers can be associated with eosinophilia.
Can eosinophilia cause autoimmune disease?
Autoimmune diseases usually are not associated with eosinophilia, but can be under some circumstances.
Is eosinophilia a diagnosis of HES?
Finally, idiopathic eosinophilia is associated with a diagnosis of the hypereosinophilic syndrome (HES), in which moderate to severe eosinophilia is associated with none of the primary or secondary causes of eosinophilia, and no other diagnosis of secondary eosinophilia can be discerned. discerned. Table 1. Degrees of Eosinophilia.
What is eosinophilic esophagitis?
Eosinophilic esophagitis (EoE) is a Th2, antigen driven disease in which chronic, eosinophil rich inflammation causes symptoms of esophageal dysfunction.2Esophageal symptoms due to EoE can manifest in multiple ways including heartburn/regurgitation, vomiting, dysphagia, food impactions, and even abdominal pain.
What is EoE diagnosis?
The differential diagnosis for EoE is broad and can include gastroesophageal reflux disease (GERD), parasitic and fungal infections, inflammatory bowel disease, allergic vasculitis, connective tissue disease, and other disorders associated with esophageal eosinophilia.
What are the features of EoE?
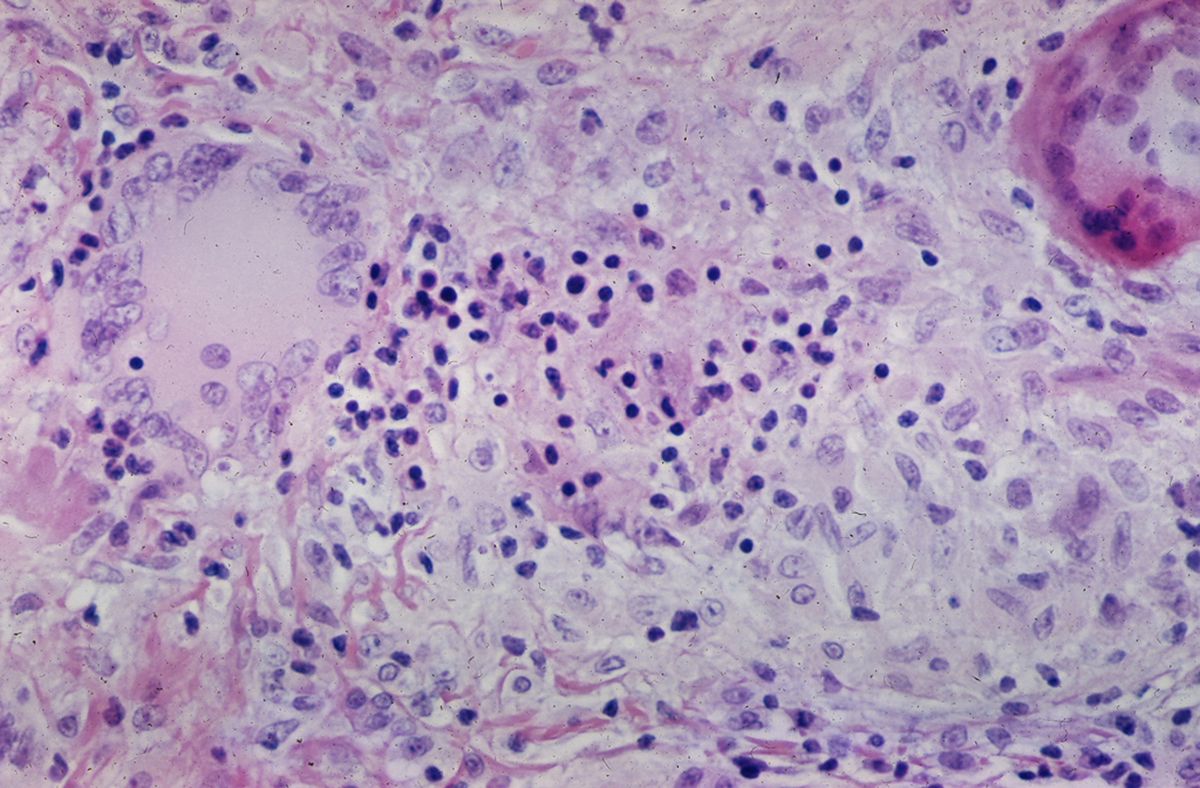
Other histologic features of EoE include superficial layering of the eosinophils, eosinophilic micro-abscesses (clusters of ≥4 eosinophils), epithelial hyperplasia, intercellular edema or spongiosis, and eosinophil degranulation.
Is IgE based testing valid for EoE?
As such, IgE based testing does not reflect the triggering mechanism in EoE and, although validated for anaphylaxis, is insufficient for guiding EoE therapy. Atopy patch testing, while reflecting the delayed type hypersensitivity mechanism of EoE, is not standardized or validated.
Does esophageal dilation help luminal patency?
Effective treatment canreverse tissue fibrosis in some patients as well as decrease the rate of food impactions. Esophageal dilation may be required to increase luminal patency. The chronic nature of EoE necessitates long-term therapy in order to avoid disease recurrence and complications.
What are the most common secondary eosinophilic conditions?
The most common secondary eosinophilic conditions requiring specific therapy are drug hypersensitivity, parasitic helminth infection, neoplasia (including lymphoma), and, in children, immunodeficiency disorders. Although a detailed discussion of the many and varied causes of secondary HE/HES is beyond the scope of this review and can be found in the published literature, 52, 53 a few points deserve mention. First, a detailed medical history is paramount, as it can provide valuable clues to the underlying diagnosis. This should include a complete list of all prescription and nonprescription drugs and supplements taken in the months preceding the onset of eosinophilia, recent and remote travel and exposures, family history of eosinophilic disorders, and a complete review of systems. Second, the time course of resolution of eosinophilia after successful treatment of secondary causes is variable. In fact, eosinophilia may resolve within days or persist for months after discontinuation of an offending drug, 54, 55 and transient exacerbation of eosinophilia is often seen following successful treatment of helminth infections. 56 Finally, lack of response to seemingly appropriate treatment should prompt assessment for other causes of HES.
How long does it take for eosinophils to decrease after corticosteroid treatment?
If the eosinophil count and symptoms do not improve after 1 to 2 days of high-dose corticosteroid therapy, a second agent should be added to rapidly lower the eosinophil count. To maximize the chance of response, selection of second-line agents should be guided by the clinical presentation.
What is the best treatment for L-HES?
Although corticosteroids are also first-line treatment of L-HES, many patients require moderate to high doses (30-60 mg prednisone equivalent daily) to induce and maintain clinical remission. When significant steroid side effects develop or eosinophilia and symptoms persist despite corticosteroid therapy, interferon-α is the preferred second-line agent due to its effects on both eosinophils and T cells. Although in vitro data suggest that interferon-α monotherapy may cause outgrowth of abnormal lymphocyte populations, 89 the utility of concomitant low-dose corticosteroid therapy to enhance apoptosis of these cells in patients with L-HES treated with interferon-α is controversial. As in idiopathic HES, other agents, including methotrexate, cyclophosphamide, cyclosporine, and alemtuzumab, have been used as steroid-sparing agents in L-HES with variable success. 16, 34
What is the AEC of a blood eosinophil?
Mild blood eosinophilia, as defined by an absolute eos inophil count (AEC) between 0.5 and 1.0 × 10 9 /L , is common, occurring in 3% to 10% of individuals depending on the population studied. 1, 2 Frequent causes include atopic disease, asthma, drug hypersensitivity, and helminth infection. In contrast, blood hypereosinophilia (HE), defined as an AEC of ≥1.5 × 10 9 /L, is relatively rare and should prompt a thorough evaluation for an underlying cause ( Table 1) and for evidence of end organ manifestations attributable to the eosinophilia, the defining feature of hypereosinophilic syndromes (HESs). Tissue HE is defined as (1) eosinophils >20% of all nucleated cells in a bone marrow aspirate; (2) tissue infiltration by eosinophils that, in the opinion of an experienced pathologist, is markedly increased; or (3) extensive extracellular deposition of eosinophil-derived proteins in tissue as demonstrated by immunostaining. 3
Do corticosteroids work for idiopathic HES?
Corticosteroids remain the mainstay of therapy for idiopathic HES. 14, 16 Although high doses are effective in most patients, dosing and duration should be individualized based on the clinical manifestations, comorbidities, and perceived risk of serious end organ damage.
