Therapy
You may receive these medicines for hypovolemic shock: Epinephrine (Adrenalin®). Norepinephrine (Levophed®). Dopamine. Dobutamine (Inotrex®). Complications/side effects of the treatment. Side effects of hypovolemic shock medicines include: Increase in blood pressure and heart rate. Difficulty breathing. Headache. Irregular heartbeat.
Nutrition
What is hypovolemic shock? Hypovolemic shock is the most severe form of hypovolemia that needs emergency treatment. This condition occurs when you lose a significant amount of fluid or blood, which prevents your heart from pumping blood throughout your body. Hypovolemic shock can cause your organs to stop functioning.
See more
Jan 31, 2022 · Treatments for hypovolemia. Because hypovolemia can quickly progress to hypovolemic shock and cause organ damage, prompt treatment for early signs of hypovolemia is critical. Treatments at this initial stage include: Oral rehydration drinks: Doctors may use this treatment in cases of mild hypovolemia.
What is hypovolemia and how is it treated?
May 08, 2017 · As for what causes hypovolemia, the answer is a few different things. 1. Loss of Fluids. The loss of fluids can cause a decrease in blood volume. The fluid loss can be caused by a number of things, such as severe burns, excessive or prolonged diarrhea, excessive sweating, and protracted and excessive vomiting.
What is the treatment plan for a patient in hypovolemic shock?
Feb 12, 2022 · Regardless, hypovolemia requires prompt attention and treatment to prevent permanent organ damage and death. Intravenous fluid resuscitation remains the most common intervention for patients in the acute setting. Much discussion has been held on the subject of specific intravenous fluids for resuscitation.
Is there a definitive blood test for hypovolemia?
Nov 15, 2021 · Treatment revolves around: controlling loss of fluid and blood; replacing what’s been lost; stabilizing damage that both caused and resulted from the hypovolemic shock
What is the most common manifestation of hypovolemia?
Jul 20, 2021 · For patients in hypovolemic shock due to fluid losses, the exact fluid deficit cannot be determined. Therefore, it is prudent to start with 2 liters of isotonic crystalloid solution infused rapidly as an attempt to quickly restore tissue perfusion.

What is the immediate treatment for hypovolemia?
What should treatment focus on when a patient is hypovolemic?
Which solution is best treatment for patient in hypovolemic shock?
What are nursing interventions for hypovolemia?
- Safe administration of blood. It is important to acquire blood specimens quickly, to obtain baseline complete blood count, and to type and crossmatch the blood in anticipation of blood transfusions.
- Safe administration of fluids. ...
- Monitor weight. ...
- Monitor vital signs. ...
- Oxygen administration.
What medications are given for hypovolemic shock?
How do you treat a patient in shock?
- Lay the Person Down, if Possible. Elevate the person's feet about 12 inches unless head, neck, or back is injured or you suspect broken hip or leg bones. ...
- Begin CPR, if Necessary. If the person is not breathing or breathing seems dangerously weak: ...
- Treat Obvious Injuries.
- Keep Person Warm and Comfortable. ...
- Follow Up.
Which of the following would be the first fluid of choice for a patient in hypovolemic shock?
What is the first step you should take for a patient with hypovolemic shock?
The first step is to get you to the emergency room as quickly as possible. Along the way, someone should try to stop any visible bleeding. Your medical team will try to: Get as much oxygen as possible to all parts of your body.Apr 30, 2020
How to treat hypovolemia?
Treatment of hypovolemia depends upon its severity. When severe, intravenous fluids and possibly blood transfusions may be necessary to rapidly raise blood volume. Medications may be used to increase blood pressure and stabilize heart rate and strength of heart contractions. Any underlying cause of hypovolemia, such as injury, must also be treated to prevent ongoing fluid losses.
What is the best treatment for hypovolemia?
Although oral rehydration with an electrolyte (salt) solution may be adequate in treating mild hypovolemia (particularly when caused by diarrhea or vomiting), intravenous fluids and blood products are preferred means of treatment for more severe hypovolemia. Additionally, oral fluids may be unsafe in treating hypovolemia resulting from injury or certain conditions requiring emergency surgery. Common treatments used to restore blood volume and circulation include:
What causes a decrease in blood volume?
Hypovolemia is a decrease in the volume of blood in your body, which can be due to blood loss or loss of body fluids. Blood loss can result from external injuries, internal bleeding, or certain obstetric emergencies. Diarrhea and vomiting are common causes of body fluid loss. Fluid can also be lost as a result of large burns, ...
What are the causes of hypovolemia?
Examples include: Decreased blood clotting ability. Diarrhea or vomiting. Excessive sweating (which can result from heat exposure) Extremes of age (infants and the elderly may be unable to take fluids)
What are the risk factors for hypovolemia?
Risk factors for hypovolemia include any of the medical conditions that may lead to hypovolemia, such as kidney disease or decreased blood clotting ability. The elderly have the highest risk of suffering complications of hypovolemia.
How does the body compensate for volume loss?
Initially, the body compensates for the volume loss by increasing the heart rate, increasing the strength of heart contractions, and constricting blood vessels in the periphery while preserving blood flow to the brain, heart and kidneys. With continuing volume loss, the body loses its ability to compensate and blood pressure drops.
Can diuretics cause hypovolemia?
Conditions that cause blood or body fluid loss can cause hypovolemia, as can inadequate fluid intake. If persistent or severe, diarrhea and vomiting can deplete body fluids. Fluids can also be lost as a result of large burns or excessive sweating. Use of diuretics can result in fluid loss by increasing urine output.
What happens if hypovolemia is not corrected?
If hypovolemia remains untreated and the cause is not corrected, the patient could become unconscious.
What is hypovolemia in the circulatory system?
This article will focus on hypovolemia as it pertains to the volume of blood relative to the available space inside the circulatory system . Each person's need for fluid is a little different and depends on lean muscle mass, cardiovascular health, body fat, and various other things.
How does hypovolemia affect shock?
As blood volume decreases, the body begins to compensate for the lack of volume by constricting blood vessels. Squeezing blood vessels makes the available space inside the cardiovascular system smaller, which means the relative volume of blood is adequate to create pressure and perfuse the tissues. 3
What are the effects of hypovolemia on the brain?
Sweating (stress response to the loss of perfusion) Lightheadedness (as loss of perfusion affects the brain) Confusion. Fatigue. Decreased blood pressure. If hypovolemia remains untreated and the cause is not corrected, the patient could become unconscious.
What are the symptoms of hypovolemia?
If the cause of the hypovolemia (see below) is not corrected and the body continues to lose fluid volume, the body responds by: 4 1 Sweating (stress response to the loss of perfusion) 2 Lightheadedness (as loss of perfusion affects the brain) 3 Confusion 4 Fatigue 5 Decreased blood pressure
How much fluid do you need to lose to get rid of hypovolemia?
There are clinical signs of hypovolemia, but it could be possible to lose up to 30% of total circulatory volume before any signs or symptoms of hypovolemia become apparent. 1
What is it called when the circulatory space is too large relative to the fluid that's available?
However, when the circulatory space is too large relative to the fluid that's available, it's known as hypovolemia. The lack of volume affects the ability of the body to adequately perfuse (fill) the tissues with blood, oxygen, and nutrients. Inadequate perfusion is a condition known as shock.
How quickly can hypovolemia be treated?
Treatment of hypovolemia should begin relatively quickly after a positive diagnosis, as the symptoms and the ailment itself can be very punishing to the body. If you are lucky and caught it at a fairly early stage, low blood volume can be treated rather swiftly.
What medications are needed for hypovolemia?
You will more than likely need intravenous fluids, and medications like dobutamine, epinephrine, dopamine, and norepinephrine may be necessary in order to get your heart rate back to normal.
How much blood volume does hypovolemia decrease?
If you are exhibiting symptoms, it’s best to get yourself checked out, because symptoms don’t usually appear until your blood volume has decreased by 10% to 20%. The doctor will take a look at you to see if your symptoms match up with those of hypovolemia.
What is hypovolemia in the body?
What is hypovolemia? Essentially, it is a decrease in the volume of blood in your body. As for what causes hypovolemia, the answer is a few different things.
What does it mean when your body has less blood?
Less blood in the body means the respiratory system needs to work harder to get more oxygen into the respiratory system. 5. Increased sweating. Your body thinks it is under attack when something like hypovolemia happens. In response, the body unleashes many defenses and warning systems.
What tests are done to confirm hypovolemia?
Those tests can include: Blood chemistry (these will also include blood tests to determine how well your kidney is functioning) Complete blood count (CBC)
Why is blood volume low?
With blood volume being low, there is less pressure in the circulatory system to move the remaining blood where it needs to go or to deliver the oxygen that the body needs.
How to manage hypovolemia?
Hypovolemia requires a multidisciplinary approach to management to improve patient outcomes. First, patients should be properly triaged by the severity of their presentation. Nurses should be properly trained and comfortable in the administration of intravenous fluids (IV) and other medications needed. Pharmacists should distribute and maintain an adequate supply of intravenous fluids readily available for fluid resuscitation. Finally, the physicians should be comfortable and astute in their management of hypovolemia, with the goal of identifying the underlying disorder and promptly treat it.
What is hypovolemia in medical terms?
Hypovolemia refers to a state of low extracellular fluid volume, generally secondary to combined sodium and water loss. All living organisms must maintain an adequate fluid balance to preserve homeostasis. This activity outlines the clinical manifestations, causes, and management of hypovolemia and highlights the interprofessional team's importance in evaluating and treating this pathology.
What is hypovolemia in the body?
Hypovolemia refers to a state of low extracellular fluid volume, generally secondary to combined sodium and water loss. All living organisms must maintain an adequate fluid balance to preserve homeostasis. Water constitutes the most abundant fluid in the body, at around 50% to 60% of the body weight. Total body water is further divided into the intracellular fluid (ICF), which comprises 55% to 75%, and the extracellular fluid (ECF), which comprises around 25-45%. The ECF is further divided into the intravascular and extravascular (interstitial) spaces. ECF is the more readily measured component as it can be estimated by arterial blood pressure.
What are dynamic hemodynamic parameters?
Dynamic hemodynamic parameters are more precise in determining the etiology of hypovolemia and response to fluid replacement. Using changes in preload and right atrium pressure, arterial blood pressure, pulse pressure, or stroke volume we can calculate the systolic pressure variation, pulse pressure variation, and stroke volume variation. It is important to specify some conditions that may decrease the reliability of these calculations:
What are the symptoms of hypovolemia?
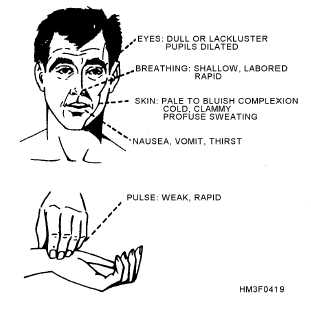
Symptoms are usually non-specific and include weakness, fatigue, dizziness, muscle cramps, and thirst. Physical examination findings are dry mucous membranes, decreased skin turgor, orthostatic tachycardia, and hypotension. Vital signs consistent with hypovolemia are hypotension and tachycardia. There is a risk of the patient's hypovolemia evolving into shock which would present with peripheral vasoconstriction, cyanosis, oliguria, and altered mental status. [2]
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Should fluids be stopped after resuscitation?
Once resuscitation targets have been met for hypovolemia, fluids administration should be stopped as excessive fluid resuscitation could lead to fluid accumulating beyond the intravascular space resulting in fluid overload and severe cardiac and pulmonary consequences. [8][9][10]
How to treat hypovolemic shock?
Once at a hospital, a person suspected of having hypovolemic shock will receive fluids or blood products via an intravenous line, to replenish the blood lost and improve circulation. Treatment revolves around controlling loss of fluid and blood, replacing what’s been lost, and stabilizing damage that both caused and resulted from the hypovole mic shock. This will also include treating the injury or illness that caused the shock, if possible.
How does hypovolemic shock affect your life?
The effects of hypovolemic shock depend on the speed at which you’re losing blood or fluids and the amount of blood or fluids you are losing. The extent of your injuries can also determine your chances for survival. Chronic medical conditions such as diabetes, previous stroke, heart, lung, or kidney disease, or taking blood thinners like Coumadin or aspirin can increase the likelihood that you’ll experience more complications from hypovolemic shock.
What happens when you lose more than 20 percent of your blood?
Hypovolemic shock is a life-threatening condition that results when you lose more than 20 percent (one-fifth) of your body’s blood or fluid supply. This severe fluid loss makes it impossible for the heart to pump a sufficient amount of blood to your body. Hypovolemic shock can lead to organ failure.
What is the most common type of shock?
Hypovolemic shock can lead to organ failure. This condition requires immediate emergency medical attention. Hypovolemic shock is the most common type of shock, with very young children and older adults being the most susceptible.
What causes a decrease in blood volume?
In addition to actual blood loss, the loss of body fluids can cause a decrease in blood volume. This can occur in cases of: excessive or prolonged diarrhea. severe burns. protracted and excessive vomiting. excessive sweating. Blood carries oxygen and other essential substances to your organs and tissues.
What to do if you have hemorrhagic shock?
If you have any signs of hemorrhaging or of hemorrhagic shock, seek medical attention immediately.
Is hypovolemic shock dangerous?
Hypovolemic shock is dangerous for everyone, but it can be particularly dangerous in older adults. Older adults who experience hypovolemic shock have higher mortality rates than their younger counterparts. They have less tolerance for the shock, and earlier treatment to prevent other complications is vital.
When etiology of hypovolemic shock has been determined, should replacement of blood or fluid loss be
When etiology of hypovolemic shock has been determined, replacement of blood or fluid loss should be carried out as soon as possible to minimize tissue ischemia. Factors to consider when replacing fluid loss include the rate of fluid replacement and type of fluid to be used. [1] Etiology.
What happens if you have hypovolemia?
If left untreated, these patients can develop ischemic injury of vital organs, leading to multi-system organ failure.
How does hypovolemic shock affect the heart?
Hypovolemic shock results from depletion of intravascular volume , whether by extracellular fluid loss or blood loss. The body compensates with increased sympathetic tone resulting in increased heart rate, increased cardiac contractility, and peripheral vasoconstriction. The first changes in vital signs seen in hypovolemic shock include an increase in diastolic blood pressure with narrowed pulse pressure. As volume status continues to decrease, systolic blood pressure drops. As a result, oxygen delivery to vital organs is unable to meet oxygen demand. Cells switch from aerobic metabolism to anaerobic metabolism, resulting in lactic acidosis. As sympathetic drive increases, blood flow is diverted from other organs to preserve blood flow to the heart and brain. This propagates tissue ischemia and worsens lactic acidosis. If not corrected, there will be worsening hemodynamic compromise and, eventually, death. [2]
Which is better for hypovolemic shock: crystalloid or colloid?
For patients with hypovolemic shock due to fluid loss, the crystalloid solution is preferred over colloid.
What causes hemorrhagic shock?
Other causes of hemorrhagic shock include gastrointestinal (GI) bleed, bleed from an ectopic pregnancy, bleeding from surgical intervention, or vaginal bleeding.
How much fluid loss can occur in a hot climate?
Skin Losses. Fluid loss also can occur from the skin. In a hot and dry climate, skin fluid losses can be as high as 1 to 2 liters/hour. Patients with a skin barrier interrupted by burns or other skin lesions also can experience large fluid losses that lead to hypovolemic shock.
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Why is hypovolemic shock important?
This is because hypovolemic shock can be caused by blood loss from traumatic injuries , internal bleeding, like a GI bleed or a surgical complication, and postpartum hemorrhage or fluid loss from burns, diarrhea and vomiting.
What is hypovolemic shock?
Pathophysiology. Hypovolemic shock is a loss of blood volume leading to decreased oxygenation of vital organs. The body’s compensatory mechanisms fail and organs begin to shut down.
How often should you give blood products during hypovolemic shock?
Usually, this would be every 15 minutes, times two, every 30 minutes times one in every hour after that. However, in hypovolemic shock, even blood products are given rapidly. Here is a look at the completed hypovolemic shock care plan. Let’s do a quick review. Hypovolemic shock is the loss of blood volume leading to decreased oxygenation of organs.
How often should you check blood for hypovolemic shock?
With the patient understanding possible reactions, send a type and crossmatch to determine the patient’s blood type. Before administration, the blood must be checked with another RN monitor using your facilities protocol. Usually, this would be every 15 minutes, times two, every 30 minutes times one in every hour after that. However, in hypovolemic shock, even blood products are given rapidly.
What happens when you lose blood volume?
This loss of blood volume results in the body’s compensatory mechanisms failing and organs therefore shutting down. Hypovolemic shock can be caused by any condition that causes a loss of circulating blood volume or plasma volume, which includes things like hemorrhage, traumatic injuries, burns, and even prolonged vomiting or diarrhea. The desired outcome is to restore circulating blood volume, preserve hemodynamics, and prevent any damage to those vital organs.
What does SVR mean in a fluid resuscitation?
SVR = Systemic Vascular Resistance. This measures afterload. We will expect this to be high because of the body’s attempts to compensate through vasoconstriction. If fluid resuscitation is effective, we will see this number return back down to normal
What does hemodynamics tell us?
Hemodynamic measurements will tell us the severity of the shock and how well the patient is responding to treatment.
What is hypovolemic shock?
Hypovolemic Shock – loss of blood volume leading to decreased oxygenation of vital organs
What happens to the body during hypovolemic shock?
After a large amount of volume loss, the body loses its ability to compensate, hence the progression into shock. We want to treat the cause and we want to replace the volume they’ve lost (and then some). We will need to support their perfusion during this process so we’ll monitor them closely and possibly start vasopressors if necessary – just remember to fill the tank first! Keep your priority nursing concepts in mind and intervene as needed. And of course remember that this is an emergency. Recognize it and act quickly!
Why do my organs not receive oxygen?
In hypovolemic shock, the initial insult, or the reason the organs aren’t receiving oxygen, is low blood volume. This could be because of a traumatic injury or hemorrhage, severe dehydration, or even burns can cause significant loss of circulating volume. If you guys can get the patho behind this, it will be easy to understand the symptoms. So if this is our circulatory system and this tank is our total blood volume, you can see here that the tank is low. So what happens is the blood that enters and fills the heart is decreased. Remember that’s called our preload. When our preload decreases, cardiac output also decreases and our body has mechanisms it uses to try to compensate. So you’ll see a lot of vasoconstriction in the body because it’s trying to push the blood back toward the heart – that means the pressure our heart has to pump against is increased – that’s our afterload. But it also means blood flow has shunted away from the non-vital organs like the skin – that’s why they get pale and cold. And then the heart rate will also increase to compensate for the lower stroke volume. After a while, we’ll begin to see our Blood pressure decrease because the body can only compensate for so long. Ultimately, there’s just not enough circulating blood volume to serve the whole system, and it will start to shut down.
What happens when your preload decreases?
When our preload decreases, cardiac output also decreases and our body has mechanisms it uses to try to compensate. So you’ll see a lot of vasoconstriction in the body because it’s trying to push the blood back toward the heart – that means the pressure our heart has to pump against is increased – that’s our afterload.
Why is there no oxygen in my body?
This could be because of a traumatic injury or hemorrhage, severe dehydration, or even burns can cause significant loss of circulating volume.