What causes a widened QRS complex?
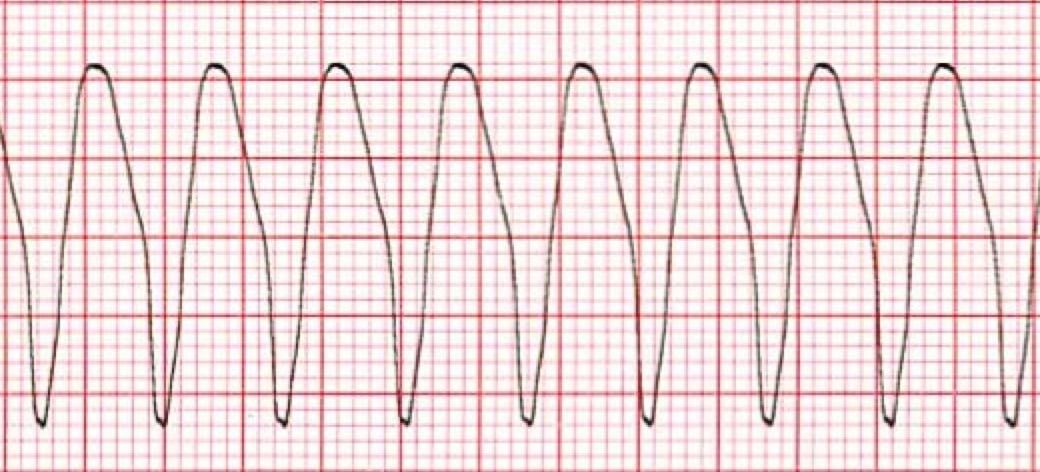
Aug 09, 2019 · VTach is often easy to recognize, however, a few notable characteristics on EKG include a broad QRS complex (often >160) with positive precordial QRS complexes (seen below). Management depends on stabilization with electricity vs. antiarrhythmic drugs as well as treatment of underlying cause.
What are the symptoms of wide complex tachycardia?
Jun 30, 2021 · Patients with suspected pacemaker mediated tachycardia (PMT) can be easily treated by temporarily applying a magnet to the device. The magnet will activate “magnet mode”, which will disable sensing and revert pacemaker function to asynchronous fixed-rate mode (usually 80 bpm).
What is the treatment for narrow complex tachycardia?
A wide QRS complex tachycardia that cannot be immediately identified, and which on clinical grounds requires prompt treatment, should be converted electrically. Drug management can be time consuming, and agents that block AV transmission, that is, verapamil and propranolol, may be life-threatening. Wide complex tachycardia: diagnosis and treatment
What is the normal range for tachycardia?
Mar 09, 2020 · A. Amiodarone would be the best long-term antiarrhythmic to suppress further arrhythmias such as this. B. For immediate treatment, intravenous (IV) esmolol is a reasonable option. C. For immediate treatment, a 0.5 mg IV dose of digoxin is a reasonable option. D. Immediate cardioversion is necessary. E.

What medication should not be given when treating wide complex tachycardia?
It is so very critical to choose the right kind of medication once the decision is made to treat a patient with wide complex tachycardia. Calcium channel blockers (Diltiazem and verapamil) are strongly advised not to be used for fear of hemodynamic collapse, hypotension and cardiac arrest [4].
Do you Cardiovert wide complex tachycardia?
Remember, with regular monomorphic tachycardias, wide or narrow, if they're symptomatic and showing signs of shock, we cardiovert them—synchronized cardioversion. With wide-complex polymorphic tachycardias, we have to defibrillate them, usually because it won't sync up with that.Feb 24, 2020
Is wide complex tachycardia fatal?
Despite hemodynamic stability in some patients with ventricular tachycardia, incorrect or untimely diagnosis can be dangerous, if not fatal.
What is considered a wide complex tachycardia?
A wide complex tachycardia (WCT) is simple enough to define: a cardiac rhythm with a rate >100 beats per minute and a QRS width >120 milliseconds (ms).
Can you give adenosine for Vtach?
Adenosine is safe and effective for differentiating wide-complex supraventricular tachycardia from ventricular tachycardia.Oct 9, 2009
When do you use adenosine vs amiodarone?
Adenosine—while a proven treatment for PSVT—can be fatal to the patient if the underlying tachyarrhythmia is incorrectly identified. Amiodarone is not the first-line treatment for many narrow complex tachyarrhythmias but it is a proven appropriate alternative that is safe across a wide range of underlying rhythms.Dec 2, 2020
What are 2 common cause of wide complex tachycardia?
Most commonly, wide-complex tachycardia or ventricular tachycardia originates from coronary artery disease. The presence of cardiomyopathies with or without left ventricular dysfunction are often already known.Apr 18, 2018
What is the first line treatment for unstable tachycardia?
Patients with unstable tachycardia should be treated immediately with synchronized cardioversion. If a pulseless tachycardia is present patients should be treated using the cardiac arrest algorithm. The AHA no longer provides specific shock dose recommendations for synchronized cardioversion.
Is tachycardia a heart disease?
Tachycardia is an increased heart rate for any reason. It can be a usual rise in heart rate caused by exercise or a stress response (sinus tachycardia). Sinus tachycardia is considered a symptom, not a disease. Tachycardia can also be caused by an irregular heart rhythm (arrhythmia).Jan 8, 2022
Can you have wide complex SVT?
When a patient with a bundle branch block experiences SVT the result is a wide complex tachycardia. Can you differentiate between SVT with aberrant conduction and VT? The short answer is yes, but it can be very difficult, and even experienced clinicians can misdiagnose VT as SVT with aberrancy!Jun 8, 2016
How long to repeat a lidocaine bolus?
Most commonly used, as clinicians are most familiar with it. Lidocaine: Dose: 1-1.5 mg/kg bolus, can repeat a 0.5-0.75mg/kg bolus q5-10 minutes (for a maximum dose of 3mg/kg), then follow by a continuous infusion at 1-4mg/minute.
Does adenosine block VT?
Very helpful diagnostically to distinguish VT from SVT. Adenosine will result in a transient AV block, which may terminate some re-entrant SVTs, or block conduction to the ventricles to reveal atrial activity (such as atrial tachycardia). Adenosine generally has no effect on VT.
Is a WCT considered a VT?
Since a large majority of WCTs are VT (80%), especially in patients with ischemic or structural heart disease, and VT therapies are effective for both VT and SVT, it is more than reasonable to treat all WCT as VT if the diagnosis is uncertain.
Is midazolam good for blood pressure?
Generally midazolam (+/- fentanyl) is preferred in this case due to minimal effects on blood pressure. Ketamine is also an option, but is less frequently used due to emergence reactions. ***IMPORTANT NOTE: Electrical cardioversion should never be performed on a conscious patient.
Can IC cause aberration of SVT?
Medications: Class IA and IC can cause aberration of SVT (by their property of use dependency) QTc prolonging agents can predispose to polymorphic VT. Digoxin most commonly causes VT (monomorphic or bidirectional) Symptoms and hemodynamic status are not helpful in establishing the diagnosis in WCT. Physical Exam:
Is VT a cause of WCT?
When facing a WCT, it is important to remember that VT is the cause in 80% of the cases. If the patient has ischemic heart disease, then VT is the cause in 90% of the cases. General Approach: Misdiagnosing SVT as VT would lead to treating with cardioversion and amiodarone. This is aggressive treatment for SVT, but it’s not harmful.
What is the treatment for Wolff-Parkinson-White syndrome?
This is a classic Wolff-Parkinson-White syndrome ECG. The treatment of choice is IV procainamide, probably the only time you'll reach for this agent. Amiodarone would not be the agent to use long term given its side effects.
What is the best antiarrhythmic?
Which of the following is the best course of action? 1 A. Amiodarone would be the best long-term antiarrhythmic to suppress further arrhythmias such as this. 2 B. For immediate treatment, intravenous (IV) esmolol is a reasonable option. 3 C. For immediate treatment, a 0.5 mg IV dose of digoxin is a reasonable option. 4 D. Immediate cardioversion is necessary. 5 E. For immediate treatment, IV procainamide should be given.
What is wide complex tachycardia?
A wide-complex tachycardia can arise from a ventricular or a supraventricular origin with a regular or irregular QRS complex (table 1). Brugada criteria and the Vereckei algorithm or the simplified avR algorithm [3] are helpful in correctly identifying ventricular tachycardia. Nonetheless, 10% of cases remain misdiagnosed.
What are the first steps in tachycardia?
The first steps are maintenance of the patient’s airway with assisted breathing if necessary, cardiac monitoring to identify the heart rhythm, monitoring of blood pressure and oximetry, and establishing intravenous access [4, 5].
Is tachycardia polymorphic or polymorphic?
The morphology of the tachycardia also give hints concerning the origin. If a wide-complex tachycardia is monomorphic , its origin can be ventricular tachycardia in a structurally abnormal heart, most commonly scar re-entry in coronary artery disease or cardiomyopathies such as hypertrophic or dilated cardiomyopathy, or arrhythmogenic right ventricular cardiomyopathy (table 2). In polymorphic wide-complex tachycardia, the QT interval has to be analysed firstly. If it is normal ( cave: the Bazzet formula is not valid for correcting the QT interval during tachycardia), ischaemia or electrolyte imbalance should be considered. Torsade des pointes tachycardia results from QT interval prolongation and originates from inherited long QT syndrome, drugs, intoxication or electrolyte imbalance, to name the most common causes.
Can tachycardia be detected in the ED?
Patients with wide-complex tachycardia can present at the emergency department (ED) haemodynamically stable or unstable. ECG algorithms, as well as knowledge about pre-existing cardiac diseases, can help to identify ventricular tachycardia.
Is tachycardia considered ventricular tachycardia?
In the emergency setting, a wide-complex tachycardia always should be considered as ventricular tachycardia unlike proven otherwise, as treatment has to be initiated immediately to avoid degeneration into ventricular fibrillation.
Is tachycardia a wide complex condition?
Regular wide-complex tachycardia can be either ventricular tachycardia or supraventricular tachycardia. Ventricular tachycardia originates from the left ventricle, the left ventricular outflow tract, the right ventricle or the right ventricular outflow tract.
What causes WCT?
Three main possible causes of WCT should be considered: VT. SVT with aberrancy (i.e. reentry tachycardia with a Bundle Branch Block) Antidromic AVRT (requires an accessory pathway) There are multiple criteria to differentiate VT from SVT with aberrancy.
Is VT tolerated by a patient with a cardiac history?
One important reason this should be our train of thought is that VT is less likely to be tolerated by a patient with a cardiac history or structural heart disease compared to a younger individual without these mitigating factors.
Is adenosine good for tachycardia?
Adenosine can be used initially for stable regular wide complex tachycardia. This is because a WCT caused by SVT with aberrancy (and right ventricular outflow tract ventricular tachycardia) are responsive to adenosine. Synchronized Cardioversion is the preferred treatment for unstable WCT.