The treatment options for Squamous Cell Carcinoma In Situ of Vulva may include:
- Surgery: Complete surgical excision can be curative
- Laser ablation: The use of laser to remove solid tumors or lesions
- Radiation therapy: The use of high-energy beams to kill cancer cells
- Close monitor and follow-up reviews of the condition are important
What is the best treatment for vulvar cancer?
Treatment options for carcinoma in situ and for small pre-cancerous changes ( vulvar intraepithelial neoplasia, or VIN) are the same. If left untreated, nearly all will progress to invasive vulvar cancer. Surgery, such as laser surgery, wide local excision, or a skinning vulvectomy may be used, depending on the size and location of the cancer.
What are the treatment options for vulvar intraepithelial neoplasia?
Abstract. Between January 1960 and December 1982, 142 patients with carcinoma in situ of the vulva were treated at Cedars-Sinai Medical Center and UCLA Medical Center. Primary treatment consisted of wide excision in 45 patients; vulvectomy in 23 patients; topical chemotherapy in 9 patients; and CO2 laser therapy in 42 patients.
What are the treatment options for vulvectomy?
Jan 15, 2019 · The treatment options for Squamous Cell Carcinoma In Situ of Vulva may include: Surgery: Complete surgical excision can be curative Laser ablation: The use of laser to remove solid tumors or lesions Radiation therapy: The use of high-energy beams to kill cancer cells Close monitor and follow-up ...
What are the treatment options for pelvis cancer?
Immunotherapy Surgery Radiation therapy Chemotherapy Immunotherapy
Is vulvar carcinoma in situ cancer?
Abnormal cells are found on the surface of the vulvar skin. These abnormal cells may become cancer and spread into nearby tissue. Also called VIN and vulvar intraepithelial neoplasia.
What is the treatment for VIN?
The main treatment for VIN is usually a small operation to remove the affected area from the vulva. This is called a wide local excision. Rarely, if the area is large or there are several areas, the whole vulva may be removed. This is called a vulvectomy.
What is the standard treatment for patients with vulvar cancer?
The main treatment for vulvar cancer is surgery. Radiation therapy and chemotherapy may be used if the cancer cannot be entirely removed with surgery, if the cancer has a high risk of coming back, and/or if the cancer is found in lymph nodes.
Does vulvar cancer require chemotherapy?
In more advanced disease, chemo might be given with radiation therapy before surgery. Chemotherapy helps the radiation work better, and this may shrink the tumor so it's easier to remove with surgery. At this time, chemo is most often used for vulvar cancers that have spread or have come back after surgery.Jan 16, 2018
What does vulvar VIN look like?
Burning, tingling or soreness in the vulva area. Change in appearance of the affected area, including areas of redness or white, discolored skin. Slightly raised skin lesions; some may appear darkened like a mole or freckle.
Is VIN serious?
With VIN the cells are not cancerous. However, in time, the cells of VIN in some affected women may become cancerous. So, VIN is classed as a pre-cancerous condition. (This is similar to the abnormal cells that are found in some women following cervical screening - previously called the cervical smear test.Mar 18, 2018
Can you get rid of vulvar cancer?
The main options are surgery, radiotherapy and chemotherapy. Many women with vulval cancer have a combination of these treatments. If your cancer is at an early stage, it's often possible to get rid of it completely.
Is vulvar cancer curable?
When vulvar cancer is found and treated early, the cure rate is more than 90%. The key to a cure is to tell your doctor about any warning signs early and to have a biopsy right away. After treatment, be sure to go to all follow-up appointments that your doctor recommends.Feb 18, 2021
Is vulvar squamous cell carcinoma curable?
These cancers have spread to lymph nodes in the pelvis or to organs and tissues outside the pelvis (like the lungs or liver). There is no standard treatment for them. Surgery is not expected to cure these cancers, but may be helpful in relieving symptoms, such as bowel or bladder blockages.Jan 16, 2018
How long does it take to recover from vulvar cancer surgery?
Do not put anything into the vagina. This includes tampons, douching or having sexual intercourse. Your doctor will advise you when this area is healed well enough. This is usually in about eight weeks.
How long does it take for a vulvar biopsy to heal?
Healing duration: After a vulvar biopsy, healing usually generally occurs in five to seven days, but it may take longer depending on the depth of deficit. Time taken for healing of the area depends on the care taken after the procedure, size of the incision, location of biopsy, and type of biopsy.Nov 10, 2020
What happens if vulvar cancer is not treated?
Untreated, vulvar cancer can eventually invade the vagina, the urethra, or the anus and spread into lymph nodes in the pelvis and abdomen and into the bloodstream.
How to prevent squamous cell carcinoma in situ of vulva?
Squamous Cell Carcinoma In Situ of Vulva may be prevented by following some of these measures: Use of condoms, avoiding multiple sexual partners, etc. to avoid sexually-transmitted infections. Undertake immediate treatment of ulcers in the genital region. Avoidance of smoking.
What causes SCC in situ of Vulva?
In case HPV infection is associated with SCC In Situ of Vulva, it is caused by alteration in the DNA by the human papilloma virus that results in uncontrolled cell proliferation. Other factors that may contribute to the condition include weak immune system, sexual promiscuity, poor hygiene, smoking, etc.
What are the symptoms of squamous cell carcinoma in situ?
Squamous Cell Carcinoma In Situ of Vulva signs and symptoms may include: The presence of a single patch-like red lesion (in most cases) on the vulva (entrance to the vagina) that is poorly-defined; they may be many in number, in some cases. Itching sensation may be felt around the red patch.
What is a squamous cell carcinoma?
Squamous Cell Carcinoma In Situ of Vulva is a malignant condition affecting the skin or mucosal membranes of the vulva (external vaginal opening). The carcinoma may be present as a well-defined red patch; it is frequently solitary, but sometimes are many in number. The lesion may itch, ulcerate, or even bleed.
What is the procedure used to examine the skin?
Examination by a dermatologist using a dermoscopy, a special device to examine the skin. Skin or tissue biopsy: A skin or tissue biopsy is performed and sent to a laboratory for a pathological examination, who examines the biopsy under a microscope.
Is squamous cell carcinoma invasive?
Without treatment (or a delay in treatment), squamous cell carcinomas may evolve to invasive carcinomas, which may have poor prognoses, depending on the stage of the carcinoma.
What are the treatments for vulvar cancer?
Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
How to treat stage III vulvar cancer?
Treatment of stage III vulvar cancer may include the following: Surgery ( modified radical vulvectomy or radical vulvectomy with removal of lymph nodes in the groin and upper thigh) with or without radiation therapy. Radiation therapy or chemotherapy and radiation therapy followed by surgery.
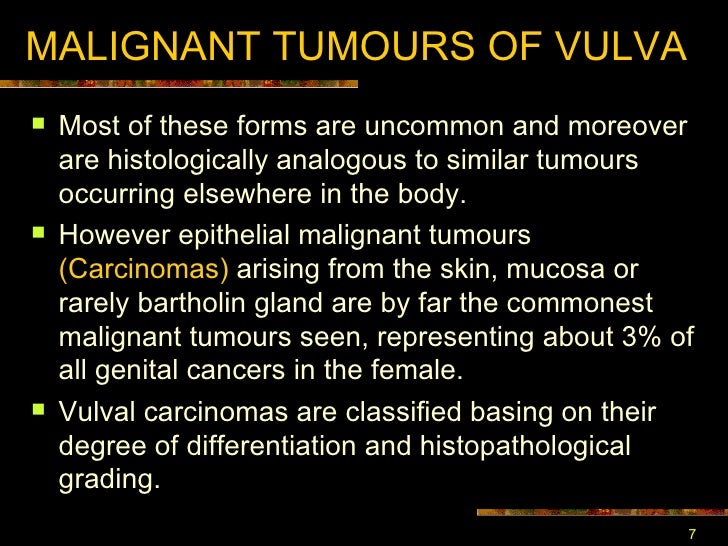
What is vulvar cancer?
Vulvar cancer is a rare disease in which malignant (cancer) cells form in the tissues of the vulva. Having vulvar intraepithelial neoplasia or HPV infection can increase the risk of vulvar cancer. Signs of vulvar cancer include bleeding or itching in the vulvar area.
Where does vulvar cancer grow?
Vulvar cancer usually forms slowly over many years. Abnormal cells can grow on the surface of the vulvar skin for a long time.
What is HPV test?
Human papillomavirus (HPV) test: A laboratory test used to check DNA or RNA for certain types of HPV infection. Cells are collected from the vulva and DNA or RNA from the cells is checked to find out if an infection is caused by a type of human papillomavirus that is linked to vulvar cancer.
Can vulvar cancer cause warts?
Vulvar cancer often does not cause early signs or symptoms. Signs and symptoms may be caused by vulvar cancer or by other conditions. Check with your doctor if you have any of the following: A lump or growth on the vulva that looks like a wart or ulcer. Itching in the vulvar area that does not go away.
Do clinical trials include patients who have not received treatment?
Some clinical trials only include patients who have not yet received treatment . Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
What is the treatment for vulvar cancer?
For vulvar cancers, there are 3 main types of treatment. Topical Therapy for Vulvar Pre- Cancer. Surgery for Vulvar Cancer. Radiation Therapy for Vulvar Cancer. Chemotherapy for Vul var Cancer.
What to do if you have vulvar cancer?
Treating Vulvar Cancer. If you've been diagnosed with vulvar cancer, your cancer care team will discuss your treatment options with you. It's important to weigh the benefits of each treatment option against the possible risks and side effects.
What do people with cancer need?
People with cancer need support and information, no matter what stage of illness they may be in. Knowing all of your options and finding the resources you need will help you make informed decisions about your care.
What are the services offered by the American Cancer Society?
These might include nursing or social work services, financial aid, nutritional advice, rehab, or spiritual help. The American Cancer Society also has programs and services – including rides to treatment, lodging, and more – to help you get through treatment.
Who are the specialists involved in cancer care?
Many other specialists may be involved in your care as well, including nurse practitioners, nurses, psychologists, social workers, rehabilitation specialists, and other health professionals. Health Professionals Associated with Cancer Care.
Can you continue cancer treatment?
Whether or not you continue treatment, there are still things you can do to help maintain or improve your quality of life.
Is treatment information given here official policy of the American Cancer Society?
The treatment information given here is not official policy of the American Cancer Society and is not intended as medical advice to replace the expertise and judgment of your cancer care team. It is intended to help you and your family make informed decisions, together with your doctor.
Screening
Detection of the disease simply requires a minimal level of awareness on the part of the patient and examination with a significant level of suspicion on the part of the physician.
Diagnosis
To the experienced clinician, the diagnosis of a frankly malignant process will be evident. A high level of suspicion of any new lesion is appropriate. The clinician is well-advised to biopsy any new growth or suspicious change in the vulvar epithelium.
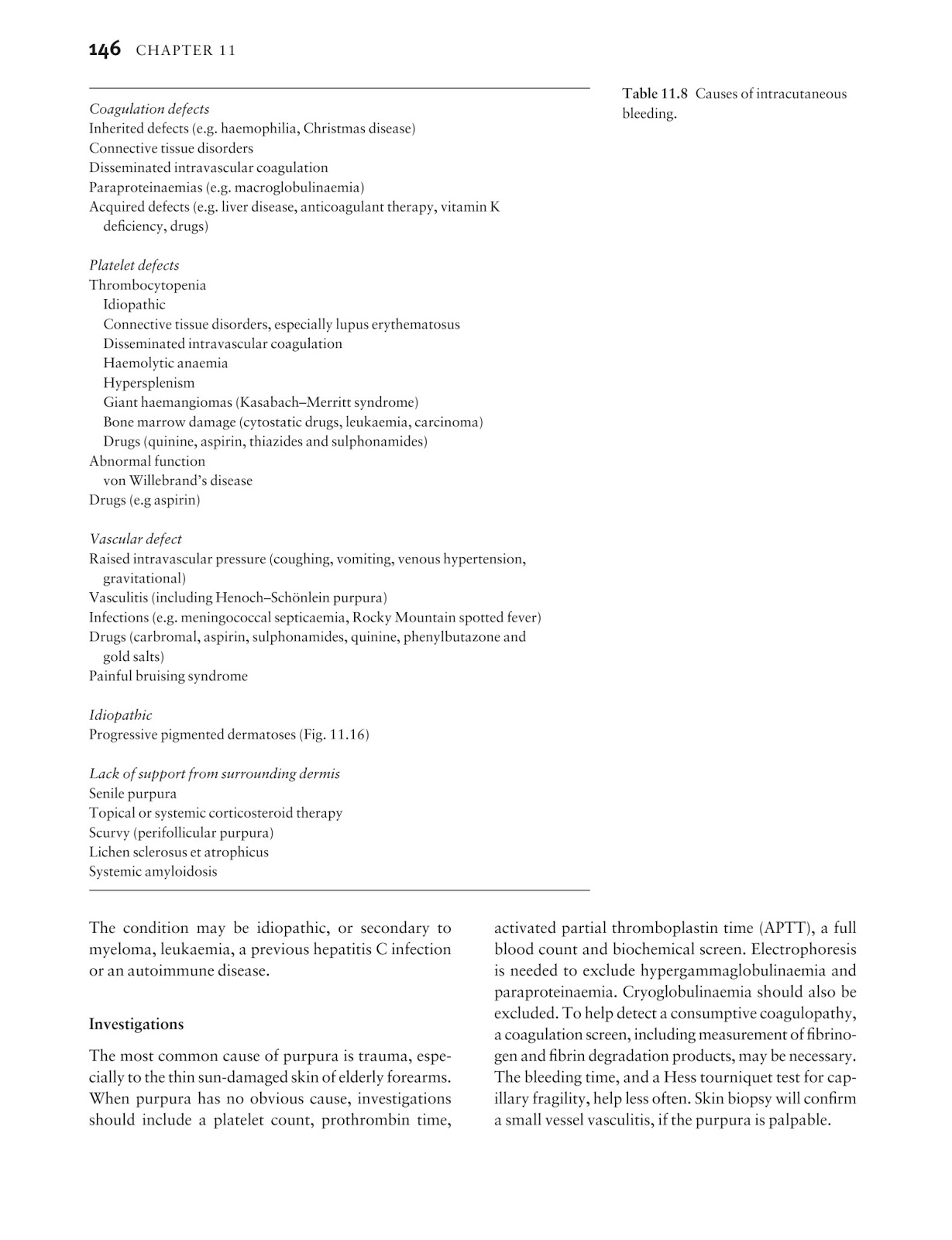
Staging
The TNM descriptive material and the International Federation of Gynecology and Obstetrics (FIGO) staging are displayed in Table 2. The purpose of staging, whether clinical or surgical, is to allow a common international vocabulary for comparison of data and to reasonably reflect clinical extent of disease.
Treatment
Therapy is obviously influenced by stage of disease, but other factors in addition to those that are included in the FIGO staging criteria (TNM) must be considered. These considerations include not only the size but also the location of the lesion.
Special Considerations
Vulvar Melanoma Vulvar melanoma is the second most frequent neoplasm of the vulva. It is found predominately in the Caucasian geriatric population, with the majority of lesions involving the clitoris or labia minor.
Treatment of Recurrence
The management of recurrent squamous cancer of the vulva is a dismal therapeutic challenge. Management decisions turn on: (1) location and extent of the recurrence, and (2) modalities available.
References
Berek JS, Heaps JM, Fu YS, et al: Concurrent cisplatin and 5-fluorouracil chemotherapy and radiation therapy for advanced-stage squamous carcinoma of the vulva. Gynecol Oncol 42:197-202, 1991.