Is Stage 0 melanoma curable?
Prognosis: Stage 0 melanoma, or melanoma in situ, is highly curable. There is very little risk for recurrence or metastasis. The 5-year survival rate as of 2018 for local melanoma, including Stage 0, is 98.4%.
How serious is melanoma in situ?
In situ melanomas don't spread to other parts of the body or cause death, but if the tumor has an opportunity to grow even one millimeter deep into the skin, it can lead to more involved treatment and greater danger. If left untreated, it can metastasize and even become life-threatening.
Is melanoma in situ considered cancer?
Melanoma in situ is also called stage 0 melanoma. It means there are cancer cells in the top layer of skin (the epidermis). The melanoma cells are all contained in the area in which they started to develop and have not grown into deeper layers of the skin. Some doctors call in situ cancers pre cancer.
How long does melanoma in situ take to spread?
The lesion can grow slowly for 5 to 15 years in the in situ form before becoming invasive.
What is the 5 year survival rate for stage 0 melanoma?
Stage 0: The 5-year relative survival rate is 97%. Stage I: The 5-year survival rate is 90-95%. If a sentinel node biopsy yields findings of melanoma in the lymph nodes, the 5-year survival is approximately 75%.
How quickly should melanoma in situ be removed?
Hypothesis-based, informal guidelines recommend treatment within 4–6 weeks. In this study, median surgical intervals varied significantly between clinics and departments, but nearly all were within a 6-week frame. Key words: melanoma, surgical interval, treatment time, melanoma survival, time factors.
How thick is melanoma in situ?
This stage is also known as melanoma in situ. The tumor is more than 1 mm thick (T2b or T3) and may be thicker than 4 mm (T4). It might or might not be ulcerated. The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0).
Is melanoma in situ hereditary?
Familial melanoma is a genetic or inherited condition. This means that the risk of melanoma can be passed from generation to generation in a family. To date, 2 genes have been primarily linked to familial melanoma; they are called CDKN2A and CDK4.
What causes melanoma in situ?
What causes melanoma in situ? Genetic mutations in the DNA of melanocytes are observed in melanoma in situ. These are predominantly due to exposure to ultraviolet radiation.
What is the best treatment for melanoma in situ?
Stage 0 melanoma (melanoma in situ) has not grown deeper than the top layer of the skin (the epidermis). It is usually treated by surgery (wide excision) to remove the melanoma and a small margin of normal skin around it.
Is melanoma a death sentence?
Metastatic melanoma was once almost a death sentence, with a median survival of less than a year. Now, some patients are living for years, with a few out at more than 10 years.
What is the most effective treatment for melanoma?
The main treatment for melanoma is surgical removal, or excision, of the primary melanoma on the skin. The extent of the surgery depends on the thickness of the melanoma. Most melanomas are found when they are less than 1.0 mm thick, and outpatient surgery is often the only treatment needed.
What is stage 0 melanoma?
In Stage 0 melanoma, the malignant tumor is still confined to the upper layer of the skin—the epidermis—which means the cancer cells are only in the outer layer of the skin and have not grown into the second layer of skin, called the dermis. Stage 0 melanoma is not considered invasive melanoma; the other stages (I, II, III, and IV) are invasive. In Stage 0 melanoma, there is no evidence the cancer has spread to the lymph nodes or to distant sites (metastasis). Stage 0 is local melanoma, meaning it has not spread beyond the primary tumor. Another term for Stage 0 melanoma is in situ, which means “in place” in Latin.
Is stage 0 melanoma a risk?
Risk: Patients with Stage 0 melanoma are considered at very low risk for local recurrence or for regional and distant metastases.
What is stage 0 melanoma?
Stage 0 Melanoma. When melanoma is Stage 0, sometimes referred to as ‘melanoma in situ,’ cancer cells have breached only the epidermis (the very outer layer of the skin). Stage 0 melanoma is contained completely in this layer and has not yet moved into the deeper layers of skin.
What is the staging system for melanomas?
The system assigns a stage based on tumor-node-metastasis (TNM) scores as well as additional prognostic factors. The goal is that melanomas of the same stage will have similar characteristics, treatment options, and outcomes.
Is melanoma in situ curable?
Prognosis: Stage 0 melanoma, or melanoma in situ, is highly curable. There is very little risk for recurrence or metastasis. The 5-year survival rate as of 2018 for local melanoma, including Stage 0, is 98.4%. Click here to learn more about melanoma survival rates.
What is stage 0 melanoma?
Melanoma in situ is also called stage 0 melanoma. It means there are cancer cells in the top layer of skin (the epidermis). The melanoma cells are all contained in the area in which they started to develop and have not grown into deeper layers of the skin. Some doctors call in situ cancers pre cancer. In a way, they are.
How to treat melanoma?
Surgery is the main treatment. To diagnose melanoma doctors remove the abnormal area of skin and a small area of surrounding skin. You may then need a second operation to remove a larger area of healthy tissue around where the melanoma was. This is called a wide local excision.
Is in situ cancer a cancer?
Some doctors call in situ cancers pre cancer. In a way, they are. Although the cells are cancerous, they cannot spread to other parts of the body, so in situ cancers are not a cancer in the true sense. But if they are not treated, in situ cancers can develop into invasive cancer.
How to treat stage 0 melanoma?
They are usually treated with surgical removal ("excision") of the melanoma and a minimal amount (about 0.5 cm) of normal skin (called the "margin"). Surgery at this stage usually cures the disease. For melanomas on the face, some doctors may instead prescribe a cream containing the drug Aldara (imiquimod). This is mainly used when surgery would create a cosmetic problem. The cream is applied anywhere from once a day to two times a week for around three months. 1
What does it mean when a biopsy came back positive for melanoma?
If your skin biopsy came back positive for melanoma, the most aggressive form of skin cancer, you might hear your melanoma described in stages. Early stage melanoma (0, I, or II) generally means your prognosis is good. ...
What is sentinel node biopsy?
Sentinel node lymph biopsy is recommended for stage II melanoma, as well. 3 In this procedure, a dye and a radioactive tracer are injected into the melanoma before surgery is performed. Melanomas spread by way of either the lymphatic system or the bloodstream. When they spread through the lymphatic system, they usually first spread to the lymph nodes that are closest to cancer, and once they spread to a first lymph node, spread down the line to others. Doing a sentinel node biopsy allows the surgeon to determine if a melanoma has begun to spread.
How does melanoma spread?
Melanomas spread by way of either the lymphatic system or the bloodstream. When they spread through the lymphatic system, they usually first spread to the lymph nodes that are closest to cancer, and once they spread to a first lymph node, spread down the line to others.
Is melanoma being studied?
Newer treatments are becoming available for melanoma all the time and even more are being studied in clinical trials. Talk to your healthcare provider about whether you may be a candidate for any of these studies. It's important to be your own advocate in your cancer care .
Can you take adjuvant therapy for stage 1 melanoma?
In stage I or II melanoma, your doctor may advise adjuvant therapy drugs or perhaps vaccines as part of a clinical trial to try to reduce the chance that the melanoma will come back. Current evidence for the effectiveness of adjuvant drug or radiation treatment for stage II patients, however, is limited. 3 .
Is lymph node cancer metastatic?
It's important to note that if there is evidence that cancer has spread to the sentinel node or other lymph nodes, this does not mean that it is metastatic (the cancer has spread to distant organs or other parts of the body). On your biopsy report it will likely say "metastatic to lymph nodes" but again, this does not mean that your cancer is metastatic, but only that it has the potential to become metastatic.
What are the treatment options for melanoma?
Options include: Surgical removal of the melanoma. Immunotherapy. Targeted therapy. Chemotherapy. Radiation.
How to treat melanoma early?
Tumors discovered at an early stage are confined to the upper layers of the skin and have no evidence of spread. These melanomas are treated by excisional surgery. Usually, this is the only treatment required.
How does immunotherapy help with cancer?
Immunotherapies boost the body’s ability to fight melanoma and other cancers by using synthetic versions of natural immune system proteins, or by enabling the release of cells that attack tumors. These therapies are effective when used alone or in combinations.
What is advanced melanomas?
Advanced melanomas are those that have spread beyond the original tumor, most often reaching the lymph nodes and/or distant organs and becoming more difficult to treat. In recent years, new immunotherapies and targeted therapies have achieved positive results in many patients with stage III and stage IV melanoma.
What to do if you have melanoma in your lymph node?
If melanoma is found in the sentinel node, your physician may examine the rest of the nodes in this lymphatic basin and remove any that contain cancer cells. After surgery, additional treatment may be recommended, including immunotherapy or radiation to decrease the chance that the melanoma will come back.
How long does it take for a melanoma to be removed?
Surgeons may, under certain circumstances, recommend removal of melanoma by Mohs surgery. The procedure is done in stages over a few days to remove all of the cancer cells in layers while sparing healthy tissue and leaving the smallest possible scar. One layer at a time is removed and examined until the margins are cancer-free. New advances in this technique make it easier for the surgeon to spot melanoma cells in the margins.
What is the use of immunotherapy to destroy cancer cells?
Pioneering breakthroughs in immunotherapy — the use of medicines to stimulate a patient’s immune system to destroy cancer cells — have led to significant progress in treating patients with advanced melanoma.
What is the staging system for melanoma?
The staging system most often used for melanoma is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
What is the term for a breakdown of the skin over a melanoma?
Ulceration: Ulceration is a breakdown of the skin over the melanoma. Melanomas that are ulcerated tend to have a worse outlook.
How thick is a melanoma?
Tumor thickness: The thickness of the melanoma is called the Breslow measurement. In general, melanomas less than 1 millimeter (mm) thick (about 1/25 of an inch) have a very small chance of spreading. As the melanoma becomes thicker, it has a greater chance of spreading.
How thick is a T2B tumor?
The tumor is more than 1 mm thick (T2b or T3) and may be thicker than 4 mm (T4). It might or might not be ulcerated. The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0).
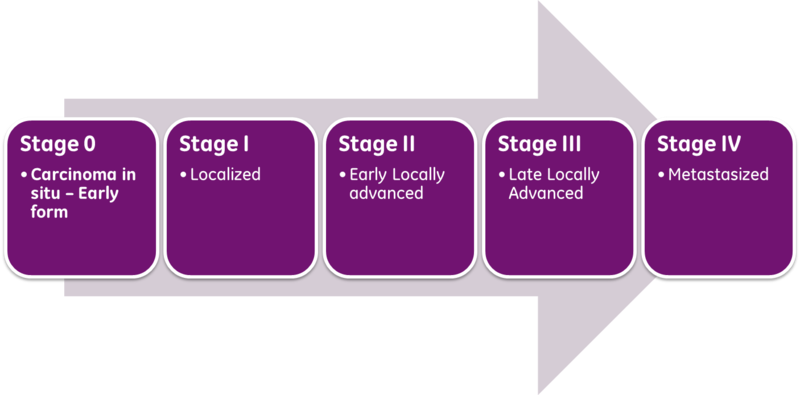
What is the stage of cancer?
The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer's stage when talking about survival statistics. The earliest stage melanomas are stage 0 (melanoma in situ), and then range from stages I (1) through IV (4).
Does melanoma spread to lymph nodes?
It has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). This stage is also known as melanoma in situ. I. The tumor is no more than 2mm (2/25 of an inch) thick and might or might not be ulcerated (T1 or T2a). The cancer has not spread to nearby lymph nodes ( N0) or to distant parts of the body (M0) II.
Does M0 have a spread?
It has not spread to distant parts of the body (M0).
What is the standard margin for melanoma in situ?
Most international clinical guidelines recommend 5–10 mm clinical margins for excision of melanoma in situ (MIS). While the evidence supporting this is weak, these guidelines are generally consistent. However, as a result of the high incidence of subclinical extension of MIS, especially of the lentigo maligna (LM) subtype, wider margins will often be needed to achieve complete histologic clearance. In this review, we assessed all available contemporary evidence on clearance margins for MIS. No randomized trials were identified and the 31 non-randomized studies were largely retrospective reviews of single-surgeon or single-institution experiences using Mohs micrographic surgery (MMS) for LM or staged excision (SE) for treatment of MIS on the head/neck and/or LM specifically. The available data challenge the adequacy of current international guidelines as they consistently demonstrate the need for clinical margins > 5 mm and often > 10 mm. For LM, any MIS on the head/neck, and/or ≥ 3 cm in diameter, all may require wider clinical margins because of the higher likelihood of subclinical spread. Histologic clearance should be confirmed prior to undertaking complex reconstruction. However, it is not clear whether wider margins are necessary for all MIS subtypes. Indeed, it seems that this is unlikely to be the case. Until optimal surgical margins can be better defined in a randomized trial setting, ideally controlling for MIS subtype and including correlation with histologic excision margins, techniques such as preliminary border mapping of large, ill-defined lesions and, most importantly, sound clinical judgement will be needed when planning surgical clearance margins for the treatment of MIS.
What is the best margin for melanoma?
One hundred years ago a 5 cm radial margin was recommended for all patients with melanoma in the hope of reducing the risk of local recurrence and improving survival. However, in the late twentieth century surgeons began selectively using narrower margins. In the past few years, the surgical management of primary melanoma has shifted from a Halstedian “more is better” philosophy to a “less is equal” approach, based on new evidence. In 2018, for example, the Swedish and Danish melanoma groups published updated results from their landmark randomized multicenter international trial of 2 cm versus 4 cm surgical excision margins for patients with invasive primary melanomas > 2 mm in thickness [1]. In their report of 936 patients with melanoma after a median follow-up of 19.6 years, the authors found no difference in overall and melanoma-specific survival between the two groups. These results definitively eliminate the need for radical surgical excision margins (> 2 cm) for melanomas ≥ 2 mm in Breslow thickness, and international guidelines will doubtless be changed to reflect this paradigm shift.
What is the clinical margin for lentigo maligna?
There is a high risk of subclinical spread in certain subsets of MIS (lentigo maligna, head and neck location, diameter ≥ 3 cm), requiring a wider clinical margin (10–15 mm) than for other forms of MIS to achieve histologic clearance
What is a clinical photograph of LM on the arm?
Clinical photograph of a LM on the arm showing measurement of a surgical margin at the time of wide excision, with the goal of obtaining histologic clearance. The total extent of the lesion is outlined (dotted line) and then a surgical margin is measured around the lesion (solid line)
Can lentigo maligna be removed?
Lentigo maligna, (a variant of melanoma in situ), should also be surgically removed, given the risk of invasion. Currently 5 mm surgical margins are recommended
What is stage 0 cancer?
Stage 0: This is also called melanoma in situ.
What is the earliest stage of melanoma?
This is the earliest stage—it’s best to catch and treat melanocytes here before they have the chance to turn cancerous. Stage 1: In general, a stage 1 melanoma has grown deeper into the skin but hasn’t spread to the lymph nodes or other parts of the body.
What is the T category of a tumor?
The rate at which the tumor cells are dividing (also known as the mitotic rate) and the presence or absence of ulceration (an open, bleeding sore) are also considered in determining the T category. N (node): Indicates whether or not the melanoma has spread to nearby lymph nodes, or the channels connecting the lymph nodes.
What is the difference between stage 3 and stage 3 melanoma?
Stage 3: A stage 3 melanoma diagnosis means that the cancer cells have spread to nearby lymph nodes , but not to distant organs or any other part of the body . Stage 3 is divided into 3A, 3B, 3C and 3D.
What is the TNM staging system?
The American Joint Committee on Cancer has developed a uniform staging system that allows doctors to determine how advanced a melanoma is, and to share that information with each other in a meaningful way. This melanoma staging system, known as TNM staging, measures three characteristics of the cancer.
How many stages of melanoma are there?
The stages range from 1 through 4, with higher numbers indicating more advanced melanoma.
Where does melanoma spread?
Metastasis (M): Melanoma may spread almost anywhere, but it tends to travel to the lungs, liver, brain, bones and the skin or lymph nodes in other parts of the body. The letter M indicates the potential spread of the melanoma throughout the body. MX: Spread can’t be measured.