What is the best drug for Mycobacterium kansasii infection?
18 rows · Sep 24, 2018 · Mycobacterium kansasii infection is challenging to treat since the course of therapy requires ...
Which medications are used in the treatment of Mycoplasma kansasii pulmonary disease?
Short-course and effective therapies must be developed. New candidate drugs, such as tedizoid and clofazimine, exhibit excellent antimycobacterial activity against M. kansasii in vitro, but in vivo studies of their clinical applications are lacking. This paper reviews the treatment, outcomes and future directions in patients with M. kansasii-LD.
How is Mycobacterium kansasii infection diagnosed?
Dec 12, 2021 · Rifampin is the cornerstone of M kansasii therapy. The first line therapy recommended by IDSA-ATS guidelines for M. kansasii is rifampin, ethambutol, and isoniazid plus pyridoxine. [27] [28] [29] The recommended duration of therapy is at least 12 months or more with the goal to have culture negative results for 12 months on therapy.
What is the treatment for Mycoplasma kansasii resistant to rifampin?
Jun 11, 2020 · Patients in whom M kansasii infection is diagnosed should be treated with at least 3 drugs. The initial drug regimen should include rifampin, which has been shown to yield low failure rates (1.1%)...

Why is M. kansasii-LD treated?
Treatment of M. kansasii-LD is recommended because of the disease's poor prognosis and fatal outcome. The decision on the optimal time point for treatment initiation should be based on both the benefits and risks posed by multiple antimicrobial agents.
Is Mycobacterium kansasii a virulent disease?
Treatment of pulmonary disease caused by Mycobacterium kansasii. As a cause of lung disease (LD ), Mycobacterium kansasii is regarded as a highly virulent species among nontuberculous mycobacteria (NTM). Both the frequency of M. kansasii isolates and global prevalence of M. kansasii-LD have increased gradually over recent decades.
Is M. kansasii a LD?
As a cause of lung disease (LD), Mycobacterium kansasii is regarded as a highly virulent species among nontuberculous mycobacteria (NTM). Both the frequency of M. kansasii isolates and global prevalence of M. kansasii-LD have increased gradually over recent decades. Treatment of M. kansasii-LD is recommended because of the disease's poor prognosis ...
What is a mycobacterial infection?
Mycobacterial infections are grouped into Mycobacterium tuberculosis (MTB) related and those caused by atypical mycobacterial organisms (e.g., Mycobacterium kansasii, Mycobacterium leprae ). Before the advent of antibiotics, laryngeal tuberculosis (laryngeal phthisis; phthisis: to dry up) was one of the most common causes of laryngeal pathologic features.5 An autopsy study in the preantibiotic era revealed that almost 40% of patients dying of tuberculosis had laryngeal infection. 6 The majority of these patients also had gastrointestinal tuberculosis, presumably a result of swallowed infectious sputum.6 Laryngeal tuberculosis was usually accompanied by the stigmas of cavitary pulmonary disease, highly infectious sputum, progression to end-stage miliary infection, and a poor prognosis. At present, laryngotracheal tuberculosis is quite uncommon and the subject of isolated case reports.7–9
Where is M. kansasii most common?
In the United States, M. kansasii is most common in midwestern and southwestern states, especially in Texas. 178 Moreover, the majority of cases of tuberculosis occur among racial and ethnic minorities, while the majority of cases of M. kansasii pulmonary disease occur among whites.
What is the second most common cause of NTM?
Mycobacterium kansasii is usually the second most common cause of NTM disease. Isolation of the bacteria in human specimens is almost always associated with disease. The major reservoir of the bacteria is likely to be tap water. The primary manifestation of M. kansasii infection resembles that of pulmonary tuberculosis with cavitary infiltrates in ...
Which two organisms account for the most episodes of non-tuberculous systemic disease?
M. avium complex and Mycobacterium kansasii account for most episodes of non-tuberculous systemic disease, particularly since the arrival of the AIDS epidemic; the lungs and lymph nodes are the most common sites of infection.
What bacteria grows well at 37°C?
Mycobacterium kansasii, which grows well at 37°C and is isolated principally from patients with pulmonary disease. On microscopy, it often appears elongated and distinctly beaded ( Fig. 19.1 ). •. M. simiae, which, like M. kansasii, grows at 37°C and is occasionally involved in pulmonary disease. •.
What are the predisposing conditions to pulmonary disease?
Other predisposing lung conditions include bronchogenic carcinoma, bronchiectasis, silicosis, and prior tuberculosis. In contrast, most of the children and adolescents reported with M. kansasii pulmonary disease have not had underlying chronic conditions.
Which bacteria have PGLs?
The PGLs are present in significant amounts in M. leprae, M. kansasii, a few strains of M. tuberculosis, M. bovis and a few other slow-growing mycobacteria ( M. ulcerans, Mycobacterium marinum, Mycobacterium gastri, Mycobacterium microti and Mycobacterium haemophillum ).
What are the comorbidities of M. kansasii?
kansasii pulmonary disease have underlying pulmonary comorbidities, such as smoking, chronic obstructive pulmonary disease, bronchiectasis, and prior or concurrent M. tuberculosis infection.
What are the sites of extrapulmonary disease?
Common sites of extrapulmonary disease include the lymph nodes, skin, and musculoskeletal and genitourinary systems. The specificity of gamma interferon release assays (IGRAs) for M. tuberculosis may be reduced by M. kansasii infection, as M. kansasii encodes CFP-10 and ESAT-6, two antigens targeted by IGRAs.
Is M. kansasii transmitted by humans?
Human-to-human transmission is thought not to occur. Clinical syndromes and radiological findings of M. kansasii infection are mostly indistinguishable from that of Mycobacterium tuberculosis, thus requiring microbiological confirmation.
Is Mycobacterium kansasii a nontuberculous mycobacteri
The incidence of Mycobacterium kansasii varies widely over time and by region, but this organism remains one of the most clinically relevant isolated species of nontuberculous mycobacteria.
What is the best treatment for M. kansasii?
Rifampin is the cornerstone of M kansasii therapy. The first line therapy recommended by IDSA-ATS guidelines for M. kansasii is rifampin , ethambutol, and isoniazid plus pyridoxine. [27] [28] [29] The recommended duration of therapy is at least 12 months or more with the goal to have culture negative results for 12 months on therapy. M. kansasii are predictably resistant to pyrazinamide. Isoniazid (INH) resistance should be interpreted with caution as a higher concentration is needed for M. kansasii when compared to M. tuberculosis. M. kansasii organisms show resistance to isoniazid at one mcg/mL but are susceptible at five mcg/mL. In a treatment naïve patient, INH is effective regardless of concentration achieved in the serum. Rifampin -containing regimens have low failure rates (1.1%) and low long-term relapse rates (< 1%). Based on M. kansasii susceptibilities in vitro, patients with rifampin-re sistant M kansasii disease should be treated with a 3-drug regimen, which should include clarithromycin or azithromycin. The other two drugs should be chosen from moxifloxacin, ethambutol, sulfamethoxazole, or streptomycin. [3] The Clinical and Laboratory Standards Institute (CLSI) recommends that all initial isolates of M. kansasii be tested only for clarithromycin and rifampin susceptibility. INH and streptomycin susceptibility should be tested as secondary agents.
What are the clinical patterns of M. kansasii?
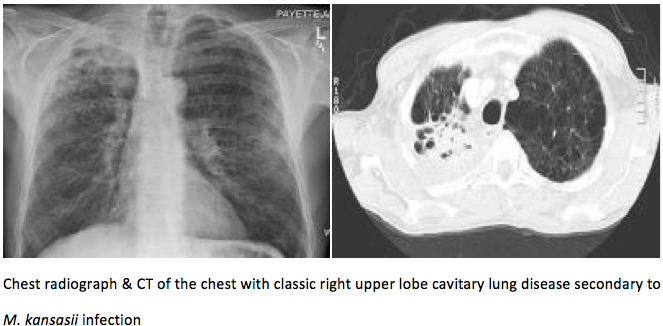
kansasii infections, can be categorized into six clinical patterns: pulmonary disease, skin, and soft tissues, musculoskeletal infections (monoarticular septic arthritis and tenosynovitis), disseminated disease, catheter-associated disease, and lymphadenitis. [20] Chronic pulmonary cavitary disease in the upper lobe is the most common presentation of M. kansasii infections. Not surprisingly these patients may be initially diagnosed with pulmonary tuberculosis. In one study, the mean age of patients with M. kansasii infection was 58 years, and 64% were men. However, M. kansasii can infect adults of any age, sex, or race. Infection results in symptoms in 85% of cases.
What temperature does mycobacterium grow?
Mycobacterium Kansasii is a slow-growing acid-fast bacillus. It grows best at 32 degrees Celcius, but can be cultured at 37 degrees. Its in-vitro and chemical characteristics are similar to those of M. marinum and M. szulgai . It produces mature colonies in greater then 7 days. Like other mycobacteria in the family, M. kansasii is strictly a gram-positive, non-motile and non-spore-forming organism. Colony morphology ranges from flat to raised and smooth to rough. When grown in the dark M. kansasii colonies are at first non-pigmented but turn yellow after exposure to light due to deposition of beta-carotene crystals. [5] Microscopic examinations show that when compared to M. tuberculosis, M. kansasii appears longer and broader and are often beaded or cross-barred in appearance when stained with Ziehl Neelsen or Kinyoun stain. [6] In Runyon classification, M. kansasii belongs to the group photochromogens. Biochemical characteristics include Catalase positive, nitrate reduction, tween hydrolysis, and urea hydrolysis. Identification using traditional methods could take as long as two months.
Why do M. kansasii colonies turn yellow?
When grown in the dark M. kansasii colonies are at first non-pigmented but turn yellow after exposure to light due to deposition of beta-carotene crystals. [5] .
What are the complications of disseminated disease?
Complications can include disseminated disease. Bone involvement, such as vertebral osteomyelitis and sacroiliitis are common with disseminated diseases. [31] Pneumothorax, Psoas abscess, bone marrow granuloma, liver granuloma, and possible spleen abscesses have also been described in the literature. [32] CNS complications like meningoencephalitis are very rare and are usually fatal.
Is M. kansasii a good disease?
Patients should know that the prognosis of M. kansasii is usually good when recognized and treated early. Treatment duration is long and the patients should adhere to the duration of the treatment as relapse rates are high if treatment is stopped early.
Is M. kansasii a treatable infection?
Treatment is prolonged and requires meticulous monitoring, but M. kansasii is a treatable infection. With rifampin-based regimens, the relapse rate is very low, and the prognosis is good. A study of 302 patients followed over more than a 50-year period (1952-1995), showed a mortality rate of 11%, but this included both immunocompromised and non-immunocompromised patients.
What is the recommended medication for M kansasii?
The 2007 ATS/IDSA guideline for the treatment of M kansasii pulmonary disease recommends a regimen containing rifampin (600 mg), ethambutol (15 mg/kg) and isoniazid (300 mg) with pyridoxine (50 mg) daily for a total duration that includes at least 12 months of negative sputum culture results. [ 24]
What are the agents that kill M kansasii?
Other agents with useful activity against M kansasii include fluoroquinolones (moxifloxacin, sparfloxacin), aminoglycosides (streptomycin, amikacin), sulfamethoxazole, bedaquiline, and oxazolidinones (tedizolid or linezolid). [ 24, 29, 30] However, clinical experience for their use in the treatment of M kansasii infection are very limited.
How much pyridoxine should I take daily?
Prophylactic doses of 6-50 mg of pyridoxine daily are recommended. Ansamycin antibiotic derived from rifamycin S. Inhibits DNA-dependent RNA polymerase, preventing chain initiation, in susceptible strains of Escherichia coli and Bacillus subtilis but not in mammalian cells.
Can rifampin be used with HIV?
Rifampin should not be used concurrently with HIV protease inhibitors or nonnucleoside reverse transcriptase inhibitors (NNRTIs) because rifampin significantly enhances their metabolism. Rifabutin at a lower dose (150 mg/d) should be substituted for rifampin in patients receiving protease inhibitors.
Does peptidyl tRNA inhibit bacterial growth?
Inhibits bacterial growth, possibly by blocking dissociation of peptidyl tRNA from ribosomes, causing RNA-dependent protein synthesis to arrest. Macrolide that inhibits bacterial growth, possibly by blocking dissociation of peptidyl tRNA from ribosomes, causing RNA-dependent protein synthesis to arrest.
Is pyrazinamide resistant to M kansasii?
Most M kansasii isolates are pyrazinamide-resistant in vitro. Pyrazinamide is unacceptable as an alternative drug for M kansasii infection. Empiric antimicrobial therapy must be comprehensive and should cover all likely pathogens in the context of the clinical setting.
How to treat NTM lung disease?
Once you treat your NTM lung disease, you can take steps to prevent another infection. These bacteria are often found in water or moist places, so take these easy steps: Avoid hot tubs or spas. If you have a hot tub, make sure it’s outside your house.
How to get rid of mucus in lungs?
Talk to your doctor first if you’d like to try any of these therapies: Nebulized hypertonic saline: A machine called a nebulizer sprays sterile, salty water into your airways to help clear mucus from your lungs. High-frequency chest wall oscillation: This device loosens mucus in your lungs. Physical therapy.
What antibiotics are used for MAC?
For MAC Infection. Doctors treat mycobacterium avium complex (MAC) disease, the most common NTM lung infection, with a combination of three antibiotics: If you have more severe MAC disease that results from cavities in your lungs, your doctor may try rifabutin ( Mycobutin) instead of rifampin ( Rifadin, Rimactane ).
What to ask your doctor about NTM?
What to Ask Your Doctor. If you’re diagnosed with nontuberculous mycobacterial lung disease, your doctor will discuss the right treatment for you. Some people with NTM lung disease don’t need treatment. Others require ongoing treatments to keep their disease under control.
What to do if you have a numbness in your hands?
If you notice sudden problems with your hearing or eyesight, or pain or numbness in your hands or feet, call them right away. Surgery. Antibiotics alone may not clear up your infection or ease your symptoms. Some people also need surgery to take out damaged lung tissue.
What is the best medicine for MAC?
Rifampin ( Rifadin, Rimactane) If you have more severe MAC disease that results from cavities in your lungs, your doctor may try rifabutin ( Mycobutin) instead of rifampin ( Rifadin, Rimactane ). They might add amikacin or streptomycin three times a week early in your treatment. Continued.
How to help someone with lung disease?
Counseling or support groups of other people with lung disease can help you manage depression or anxiety. Check out groups in your area or online. Let your doctor know if your lung disease makes you feel depressed or hopeless, so you can get treatment right away. Pagination.
