Nutrition
Horner syndrome
- Diagnosis. In addition to a general medical examination, your doctor will conduct tests to judge the nature of your symptoms and identify a possible cause.
- Treatment. There's no specific treatment for Horner syndrome. ...
- Preparing for your appointment. ...
See more
Some of the many conditions that may produce Horner’s syndrome include:
- Trauma to the neck or head
- Infections
- Tumor at the top of the lung
- Lung cancer
- Thyroid tumor
- Migraines or cluster headaches
- Cerebrovascular — interruption of the blood flow to the brain caused by a stroke, aneurysm, or blood clot (embolism)
What can be done to treat Horner's syndrome?
There's no specific treatment for Horner syndrome. Often, Horner syndrome disappears when an underlying medical condition is effectively treated. In most nonemergency situations, you will start by seeing a family doctor or an eye specialist (ophthalmologist).
What are the treatment options for Horner syndrome?
Other than this, Horner Syndrome itself is not serious. To summarize, Horner Syndrome is a collection of symptoms that are caused due to disruption of nerve pathway of the sympathetic nervous system. This results in droopiness of the eyelid, anisicoria, and hypohidrosis or decreased sweat in the affected area of the face.
Are there any natural treatment for Horner's syndrome?
How serious is Horner syndrome?
See more

Is Horners syndrome serious?
It can affect people of all races and ethnic groups. The symptoms associated with Horner's syndrome, in and of themselves, generally do not cause significant problems with a person's health or vision. However, they can indicate the presence of an underlying health problem that may be very serious.
What are the 3 classic signs of Horner's syndrome?
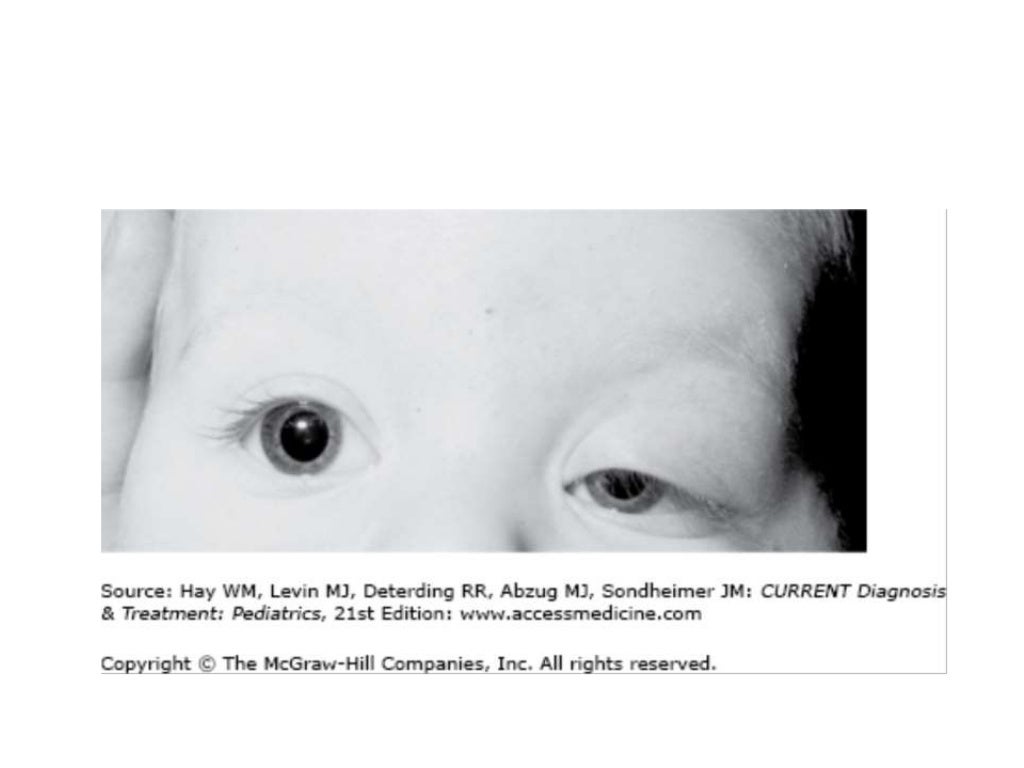
Typically, signs and symptoms of Horner syndrome include decreased pupil size, a drooping eyelid and decreased sweating on the affected side of the face.
How long does it take for Horner's syndrome to go away?
What is the recovery rate? If the lesion is not due to any pathological cause, a slow recovery lasting up to several weeks to 4 months can be expected.
Does Horner's syndrome go away on its own?
In many cases, the symptoms of Horner syndrome will go away once the underlying condition is addressed. In other cases, no treatment is available.
What is the most common cause of Horner's syndrome?
The congenital, and more rare, form of Horner syndrome is present at birth but the cause is not known. Most often, Horner syndrome is acquired as a result of some kind of interference with the sympathetic nerves serving the eyes.
Can Horner's syndrome cause blindness?
The abnormalities in the eye area related to Horner syndrome do not generally affect vision or health. However, the nerve damage that causes Horner syndrome may result from other health problems, some of which can be life-threatening.
What cranial nerve causes Horner's syndrome?
Horner syndrome (Horner's syndrome or oculosympathetic paresis) results from an interruption of the sympathetic nerve supply to the eye and is characterized by the classic triad of miosis (ie, constricted pupil), partial ptosis, and loss of hemifacial sweating (ie, anhidrosis), as well as enophthalmos (sinking of the ...
How do you test for Horner's syndrome?
Horner's syndrome is diagnosed clinically by observing ptosis (of upper and lower lids), miosis of the ptotic eye and demonstration of dilation lag in the affected eye, and anhidrosis on the same side as the ptosis and/or mitosis.
Is Horner syndrome painful?
studied the prognosis of 90 cases of isolated Horner syndrome due to internal carotid artery dissection [3]. They found that 91% of cases of Horner syndrome due to internal carotid artery dissection were painful.
Can ear infection cause Horner's syndrome?
Horner's syndrome can result from deep ear infections because the nerves in question pass right through the middle ear (where the eardrum is) and this is where we suspected Nero's infection was coming from.
Adie syndrome
This is a rare neurological disorder that also affects the eye. Usually, the pupil is larger in the affected eye. However, in some cases, it may appear smaller and look like Horner’s syndrome. Further testing will allow your doctor to confirm this as your diagnosis.
Wallenberg syndrome
This is also a rare disorder. It’s caused by a blood clot. Some of the symptoms will mimic Horner’s syndrome. However, further testing will find other symptoms and causes leading your doctor to this diagnosis.
What Causes Horner's Syndrome?
Sympathetic nerves connect the brain to different parts of the body. The sympathetic nervous system (SNS) triggers involuntary actions in response to dangerous or stressful situations.
The 3 Types of Horner's Syndrome
The cervical ganglia has three nerve pathways. Depending on which pathway is affected, it can lead to one of three types of Bernard-Horner’s syndrome: 6
Is Horner's Syndrome Life-Threatening?
Horner syndrome does not cause any significant effects on a person’s vision and overall health. However, it may be a sign of oculosympathetic nerve damage.
When to See a Doctor
You should see a doctor as soon as you notice signs. Horner’s syndrome may occur due to serious conditions, so you must get a prompt and accurate diagnosis.
How is Horner's Syndrome Diagnosed?
A doctor may initially assess for signs of Horner’s syndrome and check for possible causes.
Treatment Options for Horner's Syndrome
According to the Genetic and Rare Diseases (GARD) Information Center, the treatment for Horner syndrome depends on the underlying cause.
What Is Horner Syndrome?
H orner syndrome is a rare condition that causes problems on one side of your face when the nerves there are damaged. It's also called Horner-Bernard syndrome or oculosympathetic palsy.
Horner Syndrome Causes
In about 35% to 40% of cases, doctors aren’t sure what exactly causes Horner syndrome. Some researchers think it can be tied to your genes.
Horner Syndrome Diagnosis
Your doctor or an eye doctor ( ophthalmologist) can do tests to check for Horner syndrome.
Horner Syndrome Treatment
There aren’t any treatments specifically for Horner syndrome. The best way to ease your symptoms is to treat the health problem that caused them.
Children
Additional signs and symptoms in children with Horner syndrome may include:
When to see a doctor
A number of factors, some more serious than others, can cause Horner syndrome. It is important to get a prompt and accurate diagnosis.
First-order neurons
This neuron pathway leads from the hypothalamus at the base of the brain, passes through the brainstem and extends into the upper portion of the spinal cord. Problems in this region that can disrupt nerve function related to Horner syndrome include:
Second-order neurons
This neuron path extends from the spinal column, across the upper part of the chest and into the side of the neck. Causes related to nerve damage in this region may include:
Third-order neurons
This neuron path extends along the side of the neck and leads to the facial skin and muscles of the iris and eyelids. Nerve damage in this region may be associated with the following:
Unknown causes
In some cases the cause of Horner syndrome cannot be identified. This is known as idiopathic Horner syndrome.
Overview
Horner’s syndrome, also known as oculosympathetic palsy or Bernard-Horner syndrome, is a relatively rare condition that affects the eyes and part of the face. It occurs due to a disruption of the pathway of the sympathetic nerves that connect the brain stem to the eyes and face.
Diagnosis and Tests
The diagnosis of Horner’s syndrome may be complex, since other disorders may cause similar symptoms. Once a definite diagnosis is made, further tests may be required to determine the underlying cause of the symptoms.
Management and Treatment
The treatment will depend on which kind of underlying disorder is causing Horner’s syndrome. Since there are many possible causes, the kinds of treatment can vary widely. Sometimes no treatment is necessary unless the patient is experiencing pain or other discomforts. If a tumor or other abnormality is found, options may include surgery.
Tests to Confirm Diagnosis
When an infant shows symptoms of Horner’s syndrome, a pupil dilation test is usually administered to see how the pupil responds to stimulation. A physical exam may follow, accompanied by an MRI to determine any birth injuries that may have led to the disorder. In some cases, a urine catecholamine test may be ordered.
Treatment
There is no specific treatment for this condition, but physicians typically identify and treat the underlying reason that the disorder developed. For instance, if it was caused by a brachial plexus injury, the nerves in the brachial plexus must heal in order to treat Horner’s syndrome.
Prognosis
While Horner’s syndrome may clear on its own or heal with medication and surgery in some infants, others may experience lifelong problems with the affected side of the face. The prognosis will greatly depend upon the severity of the disorder as well as how quickly it’s detected and treated.