
What is high grade dysplasia?
High grade dysplasia (HGD) refers to precancerous changes in the cells of the esophagus. Gastroesophageal reflux disease (GERD) can be complicated by Barrett’s esophagus (BE), a change in the normal esophageal cells to intestinal-like cells. BE cells can become abnormal or dysplastic.
Is high grade dysplasia cancer?
The high grade dysplasia is only in the top layer of cells lining the inside of the oesophagus (the epithelium). It has not started to grow into the deeper layers. High grade dysplasia can change to invasive cancer if you don't have treatment. People with Barrett’s oesophagus are at a small risk of developing these abnormal cells.
How often do colon polyps become cancer?
While the majority of colon cancers start as polyps, only 5-10% of all polyps will become cancerous. The size of a polyp typically does make a difference. The larger the polyp becomes, the bigger the risk of it developing into colon cancer.
What are the chances of a sessile polyp being cancerous?
What are the chances of a sessile polyp being cancerous? There’s a 10% chance a colon polyp that size contains cancerous cells. Which types of colon polyps are most likely to turn into cancer? Villous adenomas, also called tubulovillous adenomas, and large serrated sessile polyps are either precancerous or carry a high risk of becoming cancerous.
What is the treatment for high grade dysplasia in the colon?
The most common treatment for an adenoma is to remove it during a colonoscopy or sigmoidoscopy. Depending on the number and type of adenomas and how severe the dysplasia is, a bowel resection may be done. Your doctor may suggest you have regular follow-up with a colonoscopy or sigmoidoscopy to check for more adenomas.
Is high grade dysplasia in a colon polyp cancer?
Polyps that are only mildly abnormal (don't look much like cancer) are said to have low-grade (mild or moderate) dysplasia. Polyps that are more abnormal and look more like cancer are said to have high-grade (severe) dysplasia.
How is colon dysplasia treated?
If the lesion is flat with low-grade dysplasia, one can either suggest colectomy (especially if multifocal) or repeat the colonoscopy in three to six months to look for other evidence of dysplasia (which, if present, colectomy would be recommended).
Is high grade dysplasia malignant?
In high-grade dysplasia, the cellular changes are often reminiscent of the changes seen in cells with invasive cancer. However, these cells have not penetrated the muscularis mucosa and, therefore, do not represent a malignancy.
Is high grade dysplasia serious?
It has not started to grow into the deeper layers. High grade dysplasia can change to invasive cancer if you don't have treatment. People with Barrett's oesophagus are at a small risk of developing these abnormal cells.
How serious is dysplasia in the colon?
Abstract. Colorectal cancer is the most serious complication of chronic inflammatory bowel disease. It is generally accepted that dysplasia in most cases precedes the development of colorectal cancer. Thus, detection of dysplasia through surveillance may allow therapeutic interventions to lower the risk of cancer.
Can colon dysplasia be reversed?
Patients could be counseled that LGD is reversible and does not always lead to cancer or need for surgery.
What causes dysplasia in colon?
The risk for dysplasia and colorectal carcinoma (CRC) is largely influenced by chronicity of the disease, age of diagnosis, past familial record, and evidence of ongoing active colonic inflammation including the area of colonic involvement and concurrent existence of primary sclerosing cholangitis (PSC) [1].
Can dysplasia be reversed?
In most cases, mild dysplasia resolves on its own and doesn't become cancerous. Your doctor may recommend follow-up in a year to check for additional changes. If you have severe dysplasia (CIN II or III), your doctor may recommend treatment, such as surgery or other procedures to remove the abnormal cells.
What does it mean to have high grade dysplasia?
High grade dysplasia (HGD) refers to precancerous changes in the cells of the esophagus. Gastroesophageal reflux disease (GERD) can be complicated by Barrett's esophagus (BE), a change in the normal esophageal cells to intestinal-like cells. BE cells can become abnormal or dysplastic.
What causes high grade dysplasia?
They are usually caused by chronic infection with certain types of human papillomavirus (HPV) and are found when a Pap test or biopsy is done. If not treated, these abnormal cells may become cancer and spread into nearby tissue.
What is the next step if a colon polyp is cancerous?
In most cases, only a polypectomy and/or a local excision is needed to treat this stage of cancer. A polypectomy or local excision involves removing the polyp in its entirety during a colonoscopy. Additional treatment may be needed if a polyp or tumor is too big to be removed through local excision.
Is dysplasia a cancer?
A term used to describe the presence of abnormal cells within a tissue or organ. Dysplasia is not cancer, but it may sometimes become cancer. Dysplasia can be mild, moderate, or severe, depending on how abnormal the cells look under a microscope and how much of the tissue or organ is affected.
What is adenoma with high grade dysplasia?
"Dysplasia" is a term that describes how much your polyp looks like cancer under the microscope. Polyps that are only mildly abnormal are said to have low-grade (mild or moderate) dysplasia, while polyps that are more abnormal and look more like cancer are said to have high-grade (severe) dysplasia.
What causes dysplasia in the colon?
The risk for dysplasia and colorectal carcinoma (CRC) is largely influenced by chronicity of the disease, age of diagnosis, past familial record, and evidence of ongoing active colonic inflammation including the area of colonic involvement and concurrent existence of primary sclerosing cholangitis (PSC) [1].
What is high grade colon cancer?
What is the significance of the grade of colon cancer? Grade is one of the many factors used to help predict how likely a cancer is to grow and spread. Poorly differentiated (high-grade) colon cancers tend to grow and spread more quickly than well and moderately differentiated colon cancers.
What to do if you have a polyp in your stool?
If a polyp is found, you'll need a colonoscopy to have it removed. Stool-based tests. This type of test works by checking for the presence of blood in the stool or assessing your stool DNA. If your stool test is positive you will need a colonoscopy.
How to remove polyps from bowel?
Polyps that are too large or that can't be removed safely during screening are usually removed laparoscopically, which is performed by inserting an instrument called a laparoscope into the bowel. Colon and rectum removal.
What is the most sensitive test for colorectal polyps?
Colonoscopy, the most sensitive test for colorectal polyps and cancer. If polyps are found, your doctor may remove them immediately or take tissue samples (biopsies) for analysis. Virtual colonoscopy (CT colonography), a minimally invasive test that uses a CT scan to view your colon. Virtual colonoscopy requires the same bowel preparation as ...
What happens if you have adenomatous polyp?
If you have had an adenomatous polyp or a serrated polyp, you are at increased risk of colon cancer. The level of risk depends on the size, number and characteristics of the adenomatous polyps that were removed.
What tests can be used to detect polyps?
Screening tests play a key role in detecting polyps before they become cancerous. These tests can also help find colorectal cancer in its early stages, when you have a good chance of recovery.
How long does it take to get a colonoscopy for polyps?
You'll need follow-up screenings for polyps. Your doctor is likely to recommend a colonoscopy: In five to 10 years if you had only one or two small adenomas. In three years if you had more than two adenomas, adenomas measuring 0.4 inches (about 1 centimeter) or larger, or certain adenomas.
How big is a polyp?
Removal with forceps or a wire loop (polypectomy). If a polyp is larger than 0.4 inches (about 1 centimeter), a liquid may be injected under it to lift and isolate the polyp from surrounding tissue so that it can be removed. Minimally invasive surgery.
What is the procedure to remove a small polyp?
Polypectomy. When colon dysplasia is discovered, the physician will perform a procedure called a polyepectomy. This is a simple procedure that can be done at the same time as a colonoscopy. Biopsy forceps are used to cut off a small polyp which is removed to test if it has cancerous cells.
What is colon dysplasia?
Colon Dysplasia: Diagnosis and Management in Patients. Dysplasia is a term that refers to the abnormal growth or development of organs or cells. In relation to colorectal cancer, dysplasia is the abnormal growth and development of cells in the colon. Generally, colon cancer develops from polyps in the colon. Because polyps start to develop as ...
What is the term for the abnormal growth and development of cells in the colon?
In relation to colorectal cancer, dysplasia is the abnormal growth and development of cells in the colon. Generally, colon cancer develops from polyps in the colon. Because polyps start to develop as a person gets older, colon cancer screening guidelines suggest that everyone 50 years old and above should be screened regularly.
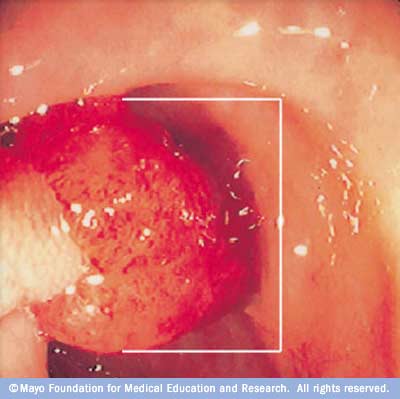
What is the test to see the inner lining of the large intestine?
Diagnosis. Diagnosis can be easily made with a colonoscopy. This is a test conducted to view the inner lining of the large intestine that includes the colon and rectum. The doctor uses a thin, flexible tube called a colonoscope to see the colon. Colonoscopy can also be used to find colon tumors, colon polyps, ulcers and areas ...
What is colon health magazine?
Colon Health Magazine is a free resource for families, providing everything from in-depth product reviews to expert advice. Our articles and guides are written by industry experts and backed by in-depth research and analysis. View all posts by Colon Health Magazine Staff.
Can a polypectomy be followed up?
Polypectomy Follow Up. There is an increased risk of colon dysplasia when a single colonic polyp is found. Although a polypectomy gets rid of a single lesion, other dormant polyps may still exist. In most cases, physicians recommend increasing rate of colonoscopies in order to make sure that all dysplasia are identified and treated accordingly.
Can radiation kill colon cancer?
In early stages of colon cancer, radiation therapy is not commonly used. references.
Why is it important to have a polyp removed?
The most important thing is that your polyp has been completely removed and does not show cancer. The growth pattern is only important because it helps determine when you will need your next colonoscopy to make sure you don’t develop colon cancer in the future.
What is a polyp made of tissue that looks much like the normal lining of your colon?
An adenoma is a polyp made up of tissue that looks much like the normal lining of your colon, although it is different in several important ways when it is looked at under the microscope. In some cases, a cancer can start in the adenoma.
What does it mean when a polyp looks like cancer?
Dysplasia is a term that describes how much your polyp looks like cancer under the microscope: Polyps that are only mildly abnormal (don’t look much like cancer) are said to have low-grade (mild or moderate) dysplasia. Polyps that are more abnormal and look more like cancer are said to have high-grade (severe) dysplasia.
What are the two major growth patterns of adenomas?
There are 2 major growth patterns: tubular and villous. Many adenomas have a mixture of both growth patterns, and are called tubulovillous adenomas. Most adenomas that are small (less than ½ inch) have a tubular growth pattern. Larger adenomas may have a villous growth pattern.
What is the beginning of the colon?
The cecum is the beginning of the colon, where the small intestine empties into the large intestine. The ascending colon, transverse colon, descending colon, and sigmoid colon are other parts of the colon after the cecum. The colon ends at the rectum, where waste is stored until it exits through the anus.
What is a polyp that grows flattened called?
Polyps that tend to grow as slightly flattened, broad-based polyps are referred to as sessile.
What is the name of the doctor who examines colons?
When your colon was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. This report helps manage your care.
Is a bowel lesion pre-cancerous?
Pre-cancerous: Villous lesions in the colon are considered pre-cancerous and your doctor is correct in advising resection of the lesion.
Can colonoscopy prevent cancer?
No.: If you have close follow up and colonoscopies you can avoid cancer. You should start by having genetic testing to see if you have hnpcc syndrome. If y ... Read More
Is colon dysplasia pre malignant?
Colon dysplasia ?'s: Sigmoid stricture with rectovaginal fistula can be surgically treated, but colon dysplasia can clearly be a pre-malignant condition. Get a referral t... Read More
What is the recurrence of colon polyps?
Colon polyp recurrence is common among patients who exhibit high grade dysplasia at index colonoscopy. Number of polyps ≥ 3 and gender (male) are traits that carry a higher risk for future occurrence for both typical and advanced adenoma.
How long does it take for colonic adenoma to progress?
Two longitudinal follow-up studies on small polyps (6–9 mm) using computed tomography found a tumor progress rates of 22% [ 42] and 35% [ 43] during follow-up periods of 8 and 3 years , respectively. Advanced disease was seen in 47% of progressive polyps [ 43 ], which is similar to the rate of 40% in our patient group with baseline adenoma number ≥ 3. The high incidence rate of recurrent and advanced adenoma in patients with multiple lesions is hard to explain solely based on incomplete resection. Multiple small polyps not detected at baseline colonoscopy might progress slowly to become detectable at surveillance colonoscopy. Multiplicity or polyclonicity in patients with adenoma number ≥ 3 is a reasonable explanation, but a longer observation period with other non-invasive study modalities such as computed tomography or capsule endoscopy to detect missed adenomas may be required to elucidate the natural history of recurrent adenomas. The surveillance period recommended by the United States Preventive Services Task Force (USPSTF) is 3 years after removal of advanced adenoma, traditional serrated adenoma, or advanced sessile serrate adenoma [ 44 ]. The European guidelines [ 45] recommend a more aggressive surveillance at 1 year for high-risk polyps (≥ 20 mm). For treatment with piecemeal resection, Walsh et al. found a rate of 14% polyp recurrence after at least one negative examination, and the rate of CRC development was 17% among 65 patients with large, flat polyps [ 46 ]. A second look examination for patients who undergo piecemeal resection or suspected incomplete resection may be warranted.
How much risk of advanced adenoma with HGD?
In a meta-analysis study by Saini [ 32 ], patients with HGD in polyps experience a 1.84-fold risk of developing advanced adenoma (95% CI 1.06–3.19) compared to those without HGD. Some other studies, including a randomized controlled trial, revealed no association of HGD with subsequent advanced adenomas during surveillance colonoscopy [ 33, 34, 35, 36 ].
How long after index colonoscopy is a follow up colonoscopy performed?
Follow-up colonoscopy was performed 6 to 12 months after index colonoscopy if adenomas were removed via the piecemeal method or if incomplete resection was suspected. Patients who underwent surveillance colonoscopy within three years of initial polypectomy were eligible for inclusion. Clinical traits including gender, age, indication of colonoscopy, family history of colon cancer, tumor number, size, site, and histology were considered.
What is the rate of metachronous adenoma after polypectomy?
The rates of recurrent metachronous adenoma and advanced adenoma after polypectomy for colon polyps with HGD were 58% and 20% , respectively. Age, gender, stool occult blood, size of polyp, morphology, pathology, and site of polyp did not differ between patients with recurrent adenoma and those without.
Can colon adenomas recur at time of colonoscopy?
Recurrence of colonic adenoma at time of follow-up colonoscopy is common in patients who undergo polypectomy for HGD colon adenomas during baseline colonoscopy. Risk of further developing advanced adenomas is associated with gender and the number of colon adenomas present.
Is a polyp smaller in the right or left colon?
Gupta S, Balasubramanian BA, Fu T, et al. Polyps with advanced neoplasia are smaller in the right than in the left colon: implications for colorectal cancer screening. Clin Gastroenterol Hepatol. 2012;10:1395–401.
What is the management of polyps?
The management of malignant polyps can be challenging and often requires a multidisciplinary approach. Emphasis should be placed on the proper initial endoscopic assessment of these polyps and appropriate, complete resection using conventional snare polypectomy or more advanced techniques, such as endoscopic mucosal resection. After successful polypectomy, regardless of technique, appropriate decision analysis must be applied to those polyps deemed “malignant”. Patients with polyps that are concerning for malignancy during endoscopy or resected polyps with high-risk features (positive or indeterminate resection margins, margin < 1 mm, lymphovascular invasion, poor differentiation, Sm3 invasion, or tumor budding) should be referred for consultation for segmental colectomy, if medically fit, as the incidence of lymph node metastasis is high. Similarly, appropriate surveillance after polypectomy is critical to mitigate the risk of recurrent or metachronous disease. By understanding the risk factors associated with lymph node metastases based on the anatomic and histologic features of polyps, we as clinicians, can help risk stratify our patients and make rational, safe and informed choices for surgery.
What is the best way to remove sessile polyps?
Larger, sessile polyps should be referred to advanced endoscopists for consideration for EMR or ESD with the ultimate goal of complete, intact resection for histological evaluation. Endoscopic mucosal resection was developed for removal of sessile polyps confined to the mucosa and submucosa and is typically used for complete excision of lesions up to 2 cm. There are several techniques for EMR that have been described including cap-, and ligation-assisted EMR; however, injection-assisted EMR is most commonly employed. This typically involves an initial submucosal injection of saline, or other suitable injectates, which elevates the identified lesion and facilitates its removal from the deeper layers with an electrocautery snare[23,24]. The inability to lift a polyp with submucosal injection heralds the potential for deeper invasion by malignancy, and indicates suitability for endoscopic management. Endoscopic submucosal dissection is generally employed for larger GI lesions but has not been widely adopted for advanced colorectal polyps. Similar to EMR, ESD initially involves the saline lift of the polyp; however, this is followed by a mucosal incision and submucosal dissection with specialized endoscopic electrosurgical knives[23,25]. These techniques are more technically challenging and are associated with slightly higher risk of serious complications (bleeding and perforation). Again it is paramount that the polypectomy site be marked endoscopically so that the area can be reassessed for surveillance or can be identified if surgery is needed.
What is the margin of a polypectomy?
However, when the resection margin is involved, or < 1 mm, the percentage of relapse ranges between 21% and 33%. Subsequently, many authors believe that a resection margin of ≥ 2 mm is ideal[2]. In 2012, Butte et al[18] reported a series of colectomies performed following polypectomy in 143 patients with clear or suspicious submucosal invasion. They found residual invasive disease in 11% of colectomy specimens. Analysis of margin status at polypectomy revealed that 16% of patients had residual invasive disease in the colon wall if the polypectomy margin was < 1 mm and 21% had residual invasive disease if the margin was indeterminate. None of the patients with a polypectomy margin ≥ 1 mm had residual invasive disease. The overall rate of lymph node metastasis in this study was 7%[18].
How are polyps classified?
Histologically, polyps are classified by several factors but perhaps the most important feature is the depth of invasion. In 1985, Haggitt et al[11] put forward a classification system for pedunculated and sessile polyps based on the depth of invasion of adenocarcinoma. According to this classification system, pedunculated polyps can be classified as levels 0-4. Level 0 indicates cancer cells that are limited to the mucosa but do not penetrate through the muscularis mucosa (carcinoma in situor intramucosal carcinoma). Levels 1 through 3 pertain to pedunculated polyps only. Level 1 indicates cancer cells invading through the muscularis mucosa into the submucosa but limited to the head of the polyp. When the cancer cells invade into the level of the neck (the junction of the head and the stalk) of the polyp, this denotes level 2. Level 3 indicates cancer cells invading any part of the stalk and level 4 signifies cancer cells invading into the submucosa of the bowel wall below the stalk of the polyp but above the muscularis propria. All sessile polyps with any degree of invasion were defined as level 4 (Figure (Figure1).1). In this landmark study, they found that level 4 invasion was associated with statistically significant adverse prognostic factors[4,6,11]. These findings were confirmed in subsequent studies. Nivatvongs et al[12] reported a series of 151 patients undergoing colectomy for polyps with invasive carcinoma to determine the incidence of lymph node metastasis based on depth of invasion. They found that 10% of patients with sessile malignant polyps had evidence of lymph node metastasis. Overall, the incidence of lymph node metastasis in patients with pedunculated polyps was 6%; however, when the level of invasion reached level 4 the incidence increased to 27%[12].
How are polyps characterized?
Polyps are initially characterized endoscopically by their size and morphology, which are two important features that may predict underlying malignancy and should ultimately guide how advanced polyps are managed. Morphologically, polyps can be broadly classified as either pedunculated or sessile. Pedunculated polyps are those attached to the colonic mucosa by a stalk of variable length, while sessile polyps grow in a more flattened pattern over the mucosa with less separation of the adenomatous epithelium from the underlying layers of the bowel wall[4]. The latter are often, understandably, more difficult to completely remove with conventional snare polypectomy, depending on their location within the colon and their size. Studies have shown that those polyps ≤ 5 mm have negligible risk of malignancy and are therefore more amenable to standard techniques for endoscopic removal. Using a prospective registry of colorectal polyps, Nusko et al[5] performed a multivariate analysis of 11188 adenomas detected at colonoscopy. Of the 5027 adenoma < 5 mm analyzed, none contained invasive carcinoma. Larger polyps between 1.5 and 3.5 cm have higher malignant potential ranging from 19%-43% and should be approached with more caution[5,6].
Is there a standard for colonoscopy after polypectomy?
However, currently there is no established standard for surveillance after endoscopic removal of malignant polyps in patients that do not undergo surgery. Most authors suggest initial follow up endoscopy in 3-6 mo but the duration of subsequent surveillance varies[8,10]. There does not appear to be a role for routine CT imaging due to its poor sensitivity.
Is colorectal cancer declining?
Fortunately, the incidence of colorectal cancer is declining, in large part due to more prevalent educational and screening programs designed to detect early cancers and their precursor polyps[1]. It is widely accepted that more than 95% of colorectal cancers arise from adenomatous polyps, which are generally defined as benign lesions with dysplastic epithelium that have variable potential for malignancy. This adenoma-carcinoma sequence is well described and is often an indolent process that can take many years to fully manifest after a stepwise accumulation of genetic alterations[2,3].
