What are the treatment options for central venous thrombosis (CVST)?
Patients with CVST without contraindications for anticoagulation (AC) should be treated either with body weight-adjusted subcutaneous low molecular weight heparin or dose-adjusted intravenous heparin. Concomitant intracranial hemorrhage related to CVST is not a contraindication for heparin therapy.
What does CVST stand for in medical terms?
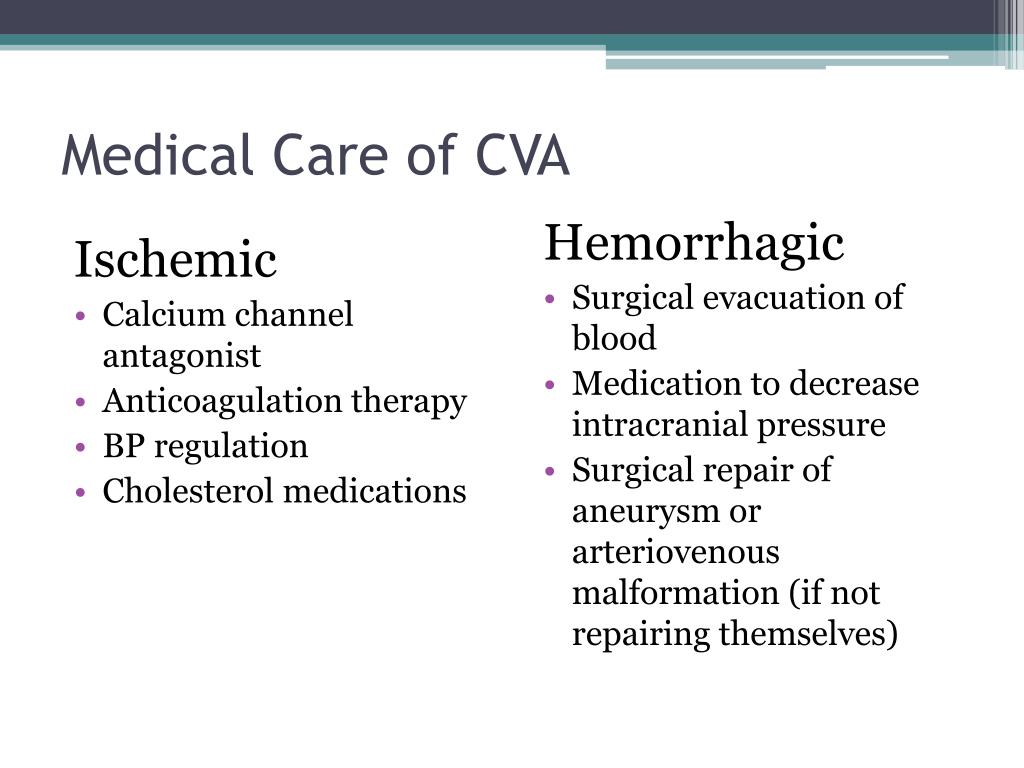
A treatment plan could include: Fluids Antibiotics, if an infection is present Antiseizure medicine to control seizures if they have occurred Monitoring and controlling the pressure inside the head Medicine called anticoagulants to stop the blood from clotting Surgery Continued monitoring of …
What is the prognosis for CVST?
The preferred initial treatment is with a low molecular weight heparin. After the acute stage of CVST, treatment with a vitamin K antagonist (oral anticoagulant therapy) is recommended. Current evidence suggests that in the future, factor Xa …
What tests are used to diagnose CVST?
How treatable is CVST?
About 80% affected by a CVST recover fully. But depending on the severity of your stroke, it may take weeks or even months to get back to normal.Apr 13, 2021
Can cerebral venous sinus thrombosis be cured?
While uncommon, cerebral venous thrombosis can become a life-threatening condition if left untreated. When caught early, CVT can be treated noninvasively using medication.Oct 27, 2017
How long does CVST last?
If the cause was a temporary trigger such as an infection, pregnancy or use of medications containing estrogen, then treatment would last 3-6 months. If the cause was not identified or if the patient has is a strong clotting disorder, then treatment may last 6-12 months.
Can you live with CVST?
CVST is a rare but potentially serious condition. Around 80% of people make a strong recovery, though some will continue to experience headache, vision problems, impaired motor control, speech problems, or other mild symptoms for weeks or months. For some, these symptoms may be permanent.Dec 16, 2021
What causes CVST?
Cerebral venous sinus thrombosis (CVST) occurs when a blood clot forms in the brain's venous sinuses. The clot keeps blood from draining out of the brain. As a result, pressure builds up in the blood vessels. This can lead to swelling and bleeding (hemorrhage) in the brain.
Is CVST a disability?
CVST is an extremely rare but serious type of stroke caused by a blood clot in a part of the brain known as the venous sinus, involving veins that carry blood away from the brain. Spontaneous CVST is estimated to affect 5 of every 1 million people in the world annually. It can cause serious disability or even death.Apr 15, 2021
What is a CVST headache like?
Headache is the most common complaint in CVST; it presents in almost 90% of patients. It is usually described as diffuse and progressive, but in a few patients may present as a thunderclap headache, suggesting subarachnoid hemorrhage [2].Oct 22, 2018
What are the signs of CVST?
Cavernous sinus thrombosis is a blood clot in the cavernous sinuses. It can be life-threatening.a sharp and severe headache, particularly around the eye.swelling and bulging of the eye(s) and the surrounding tissues.eye pain that's often severe.double vision.a high temperature.
What is the most common treatment for CVT?
Anticoagulant therapy is the most common treatment for CVT. In the 1990s, three small randomized trials demonstrated the effectiveness of heparin treatment (Einhaupl et al., 1991; Nagaraja et al., 1995; de Bruijn and Stam, 1999 ). Both low molecular weight heparin (LMWH) and unfractionated heparin (UFH) can be used to treat CVT, but some scholars have proposed that LMWH is more appropriate, except when the patient may need a surgical intervention, in which case, anticoagulation should be immediately reversed (Coutinho et al., 2010; Einhäupl et al., 2010; Misra et al., 2012 ). Misra et al. ( 2012) conducted a randomized controlled trial (RCT) in which they compared the efficacy and safety of LMWH and UFH in CVT. Thirty-two patients were administered UFH at a dose of 80 U/kg in an intravenous bolus followed by intravenous infusion at a rate of 18 U/kg/h, and 34 patients were administered LMWH at a dose of 100 units/kg subcutaneously twice daily. Six patient died, all of whom belonged to the UFH group ( P = 0.01). The authors found that hospital mortality was significantly lower in patients treated with LMWH than in patients treated with UFH. A large multicenter, multi-country study found that patients treated with LMWH had a better functional prognosis after 6 months. Patients treated with LMWH were less likely to develop new intracranial hemorrhage (adjusted odds ratio, 0.29; CI, 0.07–1.3), and this was especially true in those with intracranial lesions at baseline (0.19; CI, 0.04–0.99; Coutinho et al., 2010 ). In CVT, LMWH and UFH are usually used during the acute phase, and then oral anticoagulants are used later. The best time for anticoagulation therapy remains unclear but is usually administered from 3 to 12 months (Coutinho et al., 2011 ).
What is CVT in medical terms?
CVT is a special type of cerebrovascular disease that present with focal cerebral edema, venous cerebral infarction, seizures, and intrac ranial hypertension as its most prominent clinical features (Stam, 2005; Scheffer et al., 2017 ). The disease often affects young adults, women of childbearing age and children.
What is a CVT?
Cerebral venous thrombosis (CVT), also called cerebral venous sinus thrombosis (CVST), is a cerebrovascular disease with diverse clinical manifestations that often affects young adults, women of childbearing age, and children. It's most common clinical manifestations are headache, seizures, altered consciousness, and neurological focal signs on physical examination. CVT can manifest as a single symptom, or it can present as a syndrome consisting of multiple symptoms. This non-specific clinical picture makes diagnosing CVT difficult. Although the mortality rate of CVT has been significantly reduced by improvements in treatment and diagnostic techniques, the mortality rate of severe CVT remains as high as 34.2%. Survivors of this type of CVT have varying degrees of residual symptoms and are not able to return to their previous work. Hence, we performed a comprehensive literature search in the PubMed, EMBASE, and Medline databases to review the diagnosis and treatment of CVT.
When was CVT first diagnosed?
In 1825, Ribes ( 1825) described the first case of CVT, which was later confirmed by autopsy, in a 45-year-old male with severe headache, seizures, delirium, and thrombosis involving the superior sagittal and lateral sinuses. In 1828, Abercrombie ( 1828) reported the first postpartum CVT in a 24-year-old woman who developed headache and seizures 2 weeks after an unremarkable delivery. A subsequent autopsy revealed thrombosis of the superior sagittal sinus and cortical veins. Since these cases were published, many additional sporadic cases have been reported, and all of these were confirmed by autopsy. In rare cases, a diagnosis was achieved by angiography. Because it is difficult to diagnose, CVT is considered a serious and rare disease (Goldman et al., 1964; Rousseaux et al., 1977 ). In 1968, (Krayenbuhl, 1968) conducted a retrospective study of 92 patients with CVT diagnosed by angiography, surgery, or autopsy. Thirty-seven of these cases (40%) were associated with infection, and 17 of the remaining 55 non-infectious CVT cases were associated with pregnancy, abortion, or the perinatal period. In these patients, headache (60/92), varying degrees of paresis (56/92), and seizures (34/92) were the most common manifestations. Headache was often unilateral, and seizures were usually furious. Among these 92 patients, 35 (38%) died. In 1985, Bousser et al. ( 1985) found that the incidence of infectious CVT was significantly reduced by the use of antibiotics, whereas the incidence of CVT associated with other factors, including trauma, Behcet's disease, the perinatal period, the use of oral contraceptives, neoplasms, nephrotic syndrome, coagulation factor, and other abnormalities, was higher. With the advent of new diagnostic techniques, such as CTV and MRA, it has become easier to achieve an early diagnosis of CVT (Poon et al., 2007 ). Currently, the largest studies to explore CVT are an Italian multicenter study of 706 CVT patients and a multicenter, multi-country study of 624 patients (the International study on Cerebral Vein and Dural Sinus Thrombosis, ISCVT; Ferro et al., 2004; Dentali et al., 2012 ).
Is CVT a rare disease?
Because it is difficult to diagnose, CVT is considered a serious and rare disease (Goldman et al., 1964; Rousseaux et al., 1977 ). In 1968, (Krayenbuhl, 1968) conducted a retrospective study of 92 patients with CVT diagnosed by angiography, surgery, or autopsy.
Can thunderclap headaches be a sign of subarachnoid hemorrhage?
A thunderclap headache is noteworthy. These headaches are a serious headache that occurs suddenly and reaches a peak within 1 min. It can be seen in various diseases, the most well-known of which is subarachnoid hemorrhage. In CVT, a thunderclap headache can be combined with or without subarachnoid hemorrhage. Studies have shown that 5–13% of CVT patients may have a thunderclap headache (Wasay et al., 2010; Sparaco et al., 2015 ). de Bruijn et al. ( 1996) reported that 10 out of 71 patients with CVT had a thunderclap headache as a prominent manifestation. These included five cases who had a normal CT scan at admission, three cases with subarachnoid hemorrhage, and two with multiple cerebral hemorrhage. The authors suggest that it is difficult to distinguish a thunderclap headache in CVT from a headache caused by subarachnoid hemorrhage because the properties, clinical symptoms, and signs of the headaches are similar. Coutinho et al. (Coutinho and Stam, 2011) reported a 44-year-old female who suddenly had 2 days prior had a serious headache that lasted for a few seconds while she was wake. The headache was diffuse, radiated to the neck, and was accompanied by nausea, vomiting, and photophobia. A physical examination was unremarkable except that she exhibited mild neck resistance. A CT scan showed a hyperdense aspect of the straight sinus and no signs of subarachnoid hemorrhage. Further examination revealed complete thrombosis of the straight sinus and partial thrombosis of the bilateral transverse sinus. After the patient underwent 1 month of anticoagulation therapy, she fully recovered. Hassan et al. ( 2015) reported a 35-year-old male in whom the condition manifested mainly as a severe headache and partial seizure. A physical examination showed mild bilateral papilledema and neck resistance. A cerebral CT showed bilateral subarachnoid hemorrhage and complete thrombosis of the superior sagittal sinus. An MRV also indicated that the superior sagittal sinus was completely occluded. The patient's symptoms were relieved after he underwent anticoagulation therapy for 1 week.
Can CVT cause papilledema?
Papilledema is a common manifestation of CVT that is observed in 28–67.5% of CVT patients. Papillede ma is rare in CVT patients without headache (Ferro et al., 2004; Wasay et al., 2008; O'Rourke et al., 2014; Coutinho et al., 2015; Thammishetti et al., 2016 ). In patients with chronic onset or a late visit, papilledema is more frequent than in patients with acute onset (Ferro et al., 2005 ). Coutinho et al. ( 2014) found that papilledema was more common in patients with cortical hemorrhage (44 vs. 9%) than in those without. Eliseeva et al. ( 2015) conducted a retrospective case study of 49 patients diagnosed with CVT, including 15 who were acute (30.6%), 11 who were subacute (22.4%) and 23 who were chronic (47.0%). Papilledema was observed in 84.6% of the CVT patients with acute and subacute onset, and all patients with chronic onset had papilledema. Of the patients with acute and subacute onset, only 4% had visual impairment, and 65.2% of patients with chronic onset had visual impairment caused by papilledema or optic atrophy after papilledema.
How rare is CVST?
CVST is a rare form of stroke . It affects about 5 people in 1 million each year. The risk for this kind of stroke in newborns is greatest during the first month. Overall, about 3 out of 300,000 children and teens up to age 18 will have a stroke .
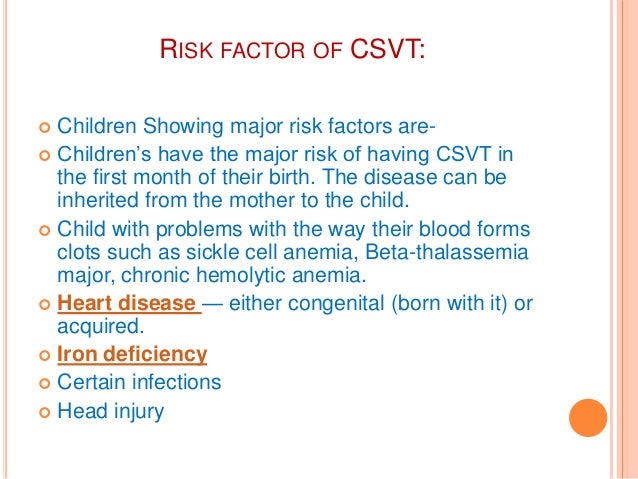
What are the risk factors for CVST?
Children and adults have different risk factors for CVST. Risk factors for children and infants include: Heart disease — either congenital (you're born with it) or acquired (you develop it) For newborns, a mother who had certain infections or a history of infertility. Risk factors for adults include:
What is the term for a blood clot in the brain?
Cerebral venous sinus thrombosis (CVST) occurs when a blood clot forms in the brain’s venous sinuses. This prevents blood from draining out of the brain. As a result, blood cells may break and leak blood into the brain tissues, forming a hemorrhage. This chain of events is part of a stroke that can occur in adults and children.
What diseases are associated with collagen?
Collagen vascular diseases like lupus, Wegener’s granulomatosis, and Behcet syndrome. Obesity. Low blood pressure in the brain (intracranial hypotension) Inflammatory bowel disease like Crohn’s disease or ulcerative colitis.
What to do if you suspect a stroke?
If you suspect a stroke based on the symptoms, have someone take you immediately to the emergency room, or call 911 to get help. Doctors typically take a medical history and do a physical exam. Family and friends can describe the symptoms they saw, especially if the person who had the stroke is unconscious.
What is the name of the condition where blood clots form in the brain?
Cerebral venous sinus thrombosis ( CVST) occurs when a blood clot forms in the brain’s venous sinuses. If you have cerebral venous sinus thrombosis: Respond quickly to symptoms like headaches, blurry vision, fainting, losing control of a part of your body, and seizures.
What are some ways to reduce blood pressure?
Lead a healthy lifestyle which includes eating a low-fat diet made up mostly of fruits and vegetables, low-fat meats and proteins, low-fat dairy products, and whole-fiber grains, breads, cereals, and pasta. Exercise daily and avoid smoking. Manage your other chronic health issues, such as diabetes or high blood pressure.
