The most common complications for patients: About 20% had dumping, which includes vomiting, reflux, and diarrhea. 12% had complications from the surgical joining of the stomach and intestine -- usually leaking or stricture. 7% had abdominal hernias.
- Acid reflux.
- Anesthesia-related risks.
- Chronic nausea and vomiting.
- Dilation of esophagus.
- Inability to eat certain foods.
- Infection.
- Obstruction of stomach.
- Weight gain or failure to lose weight.
What is surgical treatment of obesity?
Complications also may include leakage through staples or sutures, bowel obstruction, ulcers in the stomach or small intestine, blood clots in the lungs or legs, stretching of the pouch or esophagus, recurring vomiting and abdominal pain, inflammation of the gallbladder, and failure to …
Are there any complications with bariatric surgery?
Incisional hernia - This is more common in open bariatric surgery. Blood clot in the leg - This may migrate to the lung. In addition to surgical complications, long-term consequences of the malabsorption arise if patients with gastric bypass do not take supplemental vitamins, iron, and calcium. These nutritional deficiencies include the following:
What are the most common complications of gastric sleeve surgery?
· Nausea and vomiting are the most common complaints after bariatric surgery, and they are typically associated with inappropriate diet and noncompliance with a gastroplasty diet (ie, eat undisturbed, chew meticulously, never drink with meals, and wait 2 hours before drinking after solid food is consumed).
What are the health risks of obesity?
· The most common major complication includes an anastomotic leak, anastomotic stenosis with an associated small bowel obstruction, and GI hemorrhage. Weight complications, as defined as greater than 30 days postoperatively, tend to involve a small bowel obstruction, incisional hernias, and malnutrition.

What is the most common complication of bariatric surgery?
An anastomotic leak is the most dreaded complication of any bariatric procedure because it increases overall morbidity to 61% and mortality to 15%.
What are common complications after weight loss surgery?
Rare complications of gastric bypass surgery include leakage through staples or sutures, ulcers in the stomach or small intestine, blood clots in the lungs or legs, stretching of the pouch or esophagus, persistent vomiting and abdominal pain, inflammation of the gallbladder, and failure to lose weight (very rare).
What are complications after gastric sleeve?
Gastric sleeve complications can include excessive bleeding, infection, negative reaction to anesthesia, blood clots, breathing problems, and leaks from the edge of the stomach where it was cut. There are long term risks of gastric sleeve surgery as well.
What are the long term effects of weight loss surgery?
Long-term risks associated with bariatric surgery Dumping syndrome, a condition where food from the stomach is dumped into the large intestine without proper digestion. Low blood sugar. Malnutrition. Vomiting.
What are complications of dumping syndrome?
Dumping syndrome is a complication of stomach bypass or stomach reduction surgery. Other complications related to this surgery include: poor nutrient absorption. weakened bones, called osteoporosis, from poor calcium absorption. anemia, or a low red blood cell count, from poor absorption of vitamins or iron.
What are 3 common long-term complications of gastric bypass?
Longer term risks and complications of gastric bypass can include:Bowel obstruction.Dumping syndrome, causing diarrhea, nausea or vomiting.Gallstones.Hernias.Low blood sugar (hypoglycemia)Malnutrition.Stomach perforation.Ulcers.More items...•
What are the pros and cons of gastric sleeve surgery?
3. Gastric sleeve pros and cons 4Quick, dramatic weight loss.Shorter procedure time.Safer for high-risk patients than other options.Less likely to create a long-term nutrient deficiency compared to other types of bariatric surgeries.
What is Candy Cane syndrome?
Candy cane syndrome is a rare complication reported in bariatric patients following Roux-en-Y gastric bypass. It occurs when there is an excessive length of roux limb proximal to gastrojejunostomy, creating the possibility for food particles to lodge and remain in the blind redundant limb.
Do you regret bariatric surgery?
Although many women reported negative thoughts and health issues after weight loss surgery, none of them said they regret undergoing the procedure. “They say they would have done the same today and that they had no choice considering their life before surgery.
What are signs of dumping syndrome?
SymptomsFeeling bloated or too full after eating.Nausea.Vomiting.Abdominal cramps.Diarrhea.Flushing.Dizziness, lightheadedness.Rapid heart rate.
What are the complications of a weight loss surgery?
Ten percent to 20 percent of patients who have weight loss operations require follow-up operations to correct complications. Abdominal hernias are the most common complications requiring follow-up surgery.
What are the nutritional deficiencies of weight loss surgery?
Nearly 30 percent of patients who have weight loss surgery develop nutritional deficiencies such as anemia, osteoporosis and metabolic bone disease. These deficiencies can be avoided if vitamin and mineral intakes are maintained.
What is the Cleveland Clinic's obesity surgery?
Two obesity surgery procedures performed at Cleveland Clinic include gastric bypass surger y and adjustable gastric banding. For individuals who need to lose weight, bariatric surgery (also called gastric bypass, banding or weight loss surgery) has an excellent long-term track record. Long-term lifestyle changes are necessary for obesity, a chronic condition. Anyone contemplating surgical weight loss must expect to continue with the lifestyle changes and understand the surgery risks and benefits.
Why is Roux en gastric bypass called adjustable gastric banding?
It has this name because it limits and hinders the amount of calories the body can absorb. We offer two methods of surgery: Roux-en gastric bypass and a process known as adjustable gastric banding. The Roux-en- gastric procedure merges both the restrictive and the malabsorptive procedures.
What is the BMI of a morbidly obese person?
A morbidly obese person has a BMI of 40 or greater. Candidates for obesity weight loss surgery include those with a BMI of 40 or more or individuals with a BMI or 35 or more with serious health conditions. Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission.
How much weight is considered obese?
When is someone obese? He or she must weigh at least 100 pounds more than the ideal body weight or if the body mass index ( BMI) is more than 35 The BMI, a mathematical formula, considers an individual’s height and weight to determine whether they are obese. A morbidly obese person has a BMI of 40 or greater. Candidates for obesity weight loss surgery include those with a BMI of 40 or more or individuals with a BMI or 35 or more with serious health conditions.
How long does it take to lose weight after malabsorptive surgery?
Patients who have malabsorptive surgery generally lose one-half to two-thirds of their excess weight within two years. The weight loss generally continues for a year and a half before stabilizing.
What are the disadvantages of gastric bypass surgery?
Disadvantages of gastric bypass - A patient who has gastric bypass may develop the following complications: " Dumping syndrome " - Patients experience nausea, abdominal cramping, and diarrhea after eating sugar.
What is the most effective treatment for obesity?
Surgical treatment of obesity is also known as bariatric surgery or weight loss surgery. Surgery is currently the most effective treatment for morbid obesity resulting in durable and sustainable weight loss and accompanying health improvements.
What is the procedure to lose weight?
The 2 most commonly performed operations for weight loss in the United States are the Roux-en-Y gastric bypass (RYGB) and the adjustable gastric band (AGB). Both procedures could be done laparoscopically with smaller incisions than those required for traditional open approach (laparotomy). Small incisions result in less pain, early ambulation, and rapid postoperative recovery and less chance for wound complications (wound infection, fluid collection, and hernia ).
What is laparoscopic gastric binding?
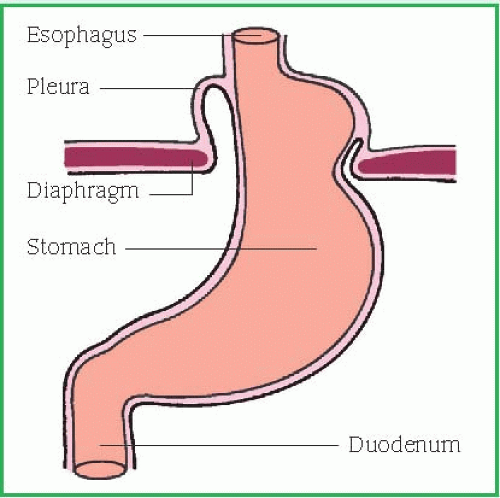
Laparoscopic adjustable gastric binding This is a purely restrictive procedure. It involves placing an inflatable silastic band around the uppermost part of the stomach. This results in a smaller upper stomach pouch and a narrow opening between the upper and lower parts of the stomach. This induces and early feeling of fullness and thereby decreases food intake. It is adjustable by changing the volume of saline in a surgically placed subcutaneous reservoir, thereby tightening or loosening the band.
What is the BMI?
A measure called the body mass index (BMI) is used to assess your weight relative to your height.
Is surgery cheaper than other treatments?
Surgery seems to be much more expensive than other treatments for obesity, but is cheaper than the treatment of all the complications of obesity. However, rates vary depending on choice of surgeon and hospital and region in which you live. Check with your carrier to see whether such operations are covered. Surgery may be covered by Medicare or Medicaid; check with your regional office.
Is gastric bypass good for sweets?
With gastric bypass, no band is introduced into the body. Also, it is a good operation for a sweet eater because eating sugar makes the patient feel ill (referred to as "dumping").
How does obesity affect health?
Patients with obesity are at major risk for developing a range of comorbid conditions, including cardiovascular disease (CVD), gastrointestinal disorders, type 2 diabetes (T2D), joint and muscular disorders, respiratory problems, and psychological issues, which may significantly affect their daily lives as well as increasing mortality risks. Obesity‐associated conditions are manifold; however, even modest weight reduction may enable patients to reduce their risk for CVD, diabetes, obstructive sleep apnea (OSA), and hypertension among many other comorbidities (Cefalu et al., 2015). A relatively small and simple reduction in weight, for example, of around 5%, can improve patient outcomes and may act as a catalyst for further change, with sustainable weight loss achieved through a series of incremental weight loss steps. In facilitating the process of losing weight for patients, nurse practitioners play an essential role. Through assessing the patient's risk, establishing realistic weight‐loss targets, providing motivation and support, and supplying patients with the necessary knowledge and treatment tools to help achieve weight loss, followed by tools for structured lifestyle support to maintain weight lost, the nurse practitioner is ideally positioned to help patient's achieve their weight‐loss—and overall health—targets.
What is the recommended weight loss target for overweight people?
Guidelines endorse weight‐loss targets of 5%–10% in individuals with obesity or overweight with associated comorbidities, as this has been shown to significantly improve health‐related outcomes for many obesity‐related comorbidities (Cefalu et al., 2015; Figure Figure3),3), including T2D prevention, and improvements in dyslipidemia, hyperglycemia, osteoarthritis, stress incontinence, GERD, hypertension, and PCOS. Further benefits may be evident with greater weight loss, particularly for dyslipidemia, hyperglycemia, and hypertension. For NAFLD and OSA, at least 10% weight loss is required to observe clinical improvements (Cefalu et al., 2015).
What is the progression from lean state to obesity?
The progression from lean state to obesity brings with it a phenotypic change in adipose tissue and the development of chronic low‐grade inflammation (Wensveen, Valentic, Sestan, Turk Wensveen, & Polic, 2015). This is characterized by increased levels of circulating free‐fatty acids, soluble pro‐inflammatory factors (such as interleukin [IL] 1β, IL‐6, tumor necrosis factor [TNF] α, and monocyte chemoattractant protein [MCP] 1) and the activation and infiltration of immune cells into sites of inflammation (Hursting & Dunlap, 2012). Obesity is also usually allied to a specific dyslipidemia profile (atherogenic dyslipidemia) that includes small, dense low‐density lipoprotein (LDL) particles, decreased levels of high‐density lipoprotein (HDL) particles, and raised triglyceride levels (Musunuru, 2010). This chronic, low‐grade inflammation and dyslipidemia profile leads to vascular dysfunction, including atherosclerosis formation, and impaired fibrinolysis. These, in turn, increase the risk for CVD, including stroke and venous thromboembolism (Blokhin & Lentz, 2013).
What percentage of Americans are obese?
In the United States in 2015, all states had an obesity prevalence more than 20% , 25 states and Guam had obesity rates >30% and four of those 25 states (Alabama, Louisiana, Mississippi, and West Virginia) had rates >35% (Centres for Disease Control and Prevention, 2016; Figure Figure1).1). Approximately 35% and 37% of adult men and women, respectively, in the United States have obesity (Yang & Colditz, 2015). Adult obesity is most common in non‐Hispanic black Americans, followed by Mexican Americans, and non‐Hispanic white Americans (Yang & Colditz, 2015). Individuals are also getting heavier at a younger age; birth cohorts from 1966 to 1975 and 1976 to 1985 reached an obesity prevalence of ≥20% by 20–29 years of age, while the 1956–1965 cohort only reached this prevalence by age 30–39 years (Lee et al., 2010). Additionally, the prevalence of childhood obesity in 2‐ to 17‐year‐olds in the United States has increased from 14.6% in 1999–2000 to 17.4% in 2013–2014 (Skinner & Skelton, 2014). Childhood obesity is an increasing health issue because of the early onset of comorbidities that have major adverse health impacts, and the increased likelihood of children with obesity going on to become adults with obesity (50% risk vs. 10% for children without obesity; Whitaker, Wright, Pepe, Seidel, & Dietz, 1997).
How much weight loss is good for comorbidities?
A recent meta‐analysis of 15 studies demonstrated that relatively small amounts of weight loss, on average 5.5 kg in the treatment arm versus 0.2 kg with placebo from an average baseline BMI of 35 kg/m2, resulted in a substantial 15% reduction in all‐cause mortality (Kritchevsky et al., 2015).
Is obesity a chronic disease?
Obesity is a chronic disease that is associated with a wide range of complications affecting many different aspects of physiology (Dobbins, Decorby, & Choi, 2013; Guh et al., 2009; Martin‐Rodriguez, Guillen‐Grima, Marti, & Brugos‐Larumbe, 2015; summarized in Table Table1).1). To examine these obesity‐related morbidities in detail is beyond the scope of this review and therefore only a brief overview of some of the key pathophysiological processes is included next.
Is weight loss curative for OSA?
Data indicate that weight loss is beneficial, although not curative, in patients with obesity who experience OSA. Meta‐analyses of patients who underwent treatment with either intensive lifestyle intervention (Araghi et al., 2013) or bariatric surgery (Greenburg, Lettieri, & Eliasson, 2009) demonstrated improvements in apnea‐hypopnea index (AHI) following treatment. In the first of these meta‐analyses, in randomized controlled trials, lifestyle intervention lead to a mean reduction in BMI of 2.3 kg/m2, which was associated with a decrease in mean AHI of 6.0 events/h. As expected, weight loss was much higher in the second meta‐analysis that investigated the effect of bariatric surgery on measures of OSA, and this was associated with greater reductions in AHI; the mean BMI reduction of 17.9 kg/m2resulted in AHI events being reduced by a mean of 38.2 events/h. Once these improvements in AHI have occurred, they seem to persist for some time, irrespective of a certain degree of weight regain. In one study, an initial mean weight loss of 10.7 kg resulted in a persistent improvement in AHI over a 4‐year period despite weight regain of approximately 50% by Year 4 (Kuna et al., 2013).