Medications include different types of blood thinners and clot dissolvers. Blood thinners (anticoagulants). These drugs prevent existing clots from enlarging and new clots from forming while your body works to break up the clots.
What are the treatment options for a brain embolism?
The treatment for a brain embolism may include medication, surgery, or both. The type of treatment a person receives depends on several factors, including: A doctor may prescribe one or more of the following medications to treat a brain embolism: thrombolytic medication to dissolves blood clots.
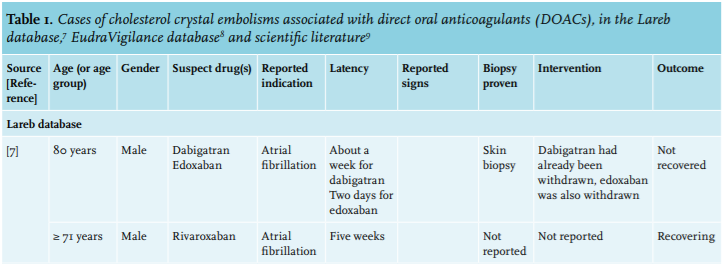
What is Crystal embolization (CCE)?
Cholesterol crystal embolization (CCE) is a dreaded complication of radiology, vascular surgery, and/or anticoagulation in patients with atherosclerosis and ulcerated aortic plaques. It also represents a cause of early graft failure and of poor results of renal artery surgery.
What is the treatment for thromboembolism?
The treatment for thromboembolism (blood clot embolism) involves anticoagulant or thrombolytic medications. Anticoagulants, such as heparin* or warfarin, are the main medications given for pulmonary embolism.
How is pulmonary embolism (PE) treated?
Treatment of pulmonary embolism is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death. Medications include different types of blood thinners and clot dissolvers. Blood thinners (anticoagulants).
How is cholesterol embolism treated?
Treatment of CES is largely supportive [10] and generally consists of fluid and blood pressure support, hemodialysis when indicated, nutritional and metabolic support. Surgical removal of the embolic source is warranted for those cases occurring spontaneously to prevent recurrent embolic showers.
What causes cholesterol crystal embolism?
Cholesterol crystal embolism, known as atheroembolic disease, is caused by showers of cholesterol crystals from an atherosclerotic plaque that occludes small arteries.
Which type of embolism is common in cholesterol cleft?
Cholesterol embolism occurs when cholesterol is released, usually from an atherosclerotic plaque, and travels as an embolus in the bloodstream to lodge (as an embolism) causing an obstruction in blood vessels further away....Cholesterol embolismSpecialtyCardiology3 more rows
What does Atheroembolism mean?
Cholesterol embolism or atheroembolism is a phenomenon where cholesterol crystals and atheroma debris such as cholesterol, platelets, and fibrins embolizes from proximal large arteries such as the aorta and its major branches to distal small arteries.
What is cholesterol embolization syndrome?
Cholesterol embolization syndrome refers to embolization of the contents of an atherosclerotic plaque (primarily cholesterol crystals) from a proximal large-caliber artery to distal small to medium arteries causing end-organ damage by mechanical plugging and an inflammatory response.
Is atherosclerosis a heart disease?
The plaque can cause your arteries to narrow, blocking blood flow. The plaque can also burst, leading to a blood clot. Although atherosclerosis is often considered a heart problem, it can affect arteries anywhere in your body. Atherosclerosis can be treated.
What does fat in the blood mean?
Hyperlipidemia, means that high levels of fats (or lipids) are in the blood. These fats include cholesterol and triglycerides. They are important for our bodies to function but when they are too high, they can put people at risk for heart disease and stroke.
How do you lower your cholesterol levels?
A few changes in your diet can reduce cholesterol and improve your heart health:Reduce saturated fats. Saturated fats, found primarily in red meat and full-fat dairy products, raise your total cholesterol. ... Eliminate trans fats. ... Eat foods rich in omega-3 fatty acids. ... Increase soluble fiber. ... Add whey protein.
What happens when cholesterol breaks down?
How is it broken down? Once in the blood stream, some cholesterol will be returned to the liver and broken down. It's used to make bile acids which are released into the intestines to help with digestion – bile acids break down the fats in food.
What is lower extremity atheroembolism?
Cholesterol embolization syndrome (CES), also known as atheroembolism, or “blue toe syndrome” from its most peripheral manifestation, refers to the release of cholesterol crystals from ruptured atherosclerotic plaque in a large artery resulting in embolization to more distal small and medium sized arteries.
Is atherosclerosis an embolism?
Two types of emboli originate from atherosclerotic plaques: thromboemboli and atheroemboli (cholesterol crystal emboli). Although the underlying risk factors may be similar, the two can often be differentiated based upon associated conditions and clinical manifestations.
What causes renal artery stenosis?
The two main causes of renal artery stenosis include: Buildup on kidney (renal) arteries. Fats, cholesterol and other substances (plaque) can build up in and on your kidney artery walls (atherosclerosis).
What is the treatment for pulmonary embolism?
Treatment of pulmonary embolism is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death.
Where to get pulmonary embolism evaluated?
Preparing for your appointment. Pulmonary embolism is often initially evaluated in hospitals, emergency rooms or urgent care centers. If you think you might have a pulmonary embolism, seek immediate medical attention.
How accurate is a pulmonary embolism test?
This test provides a clear picture of the blood flow in the arteries of your lungs. It's the most accurate way to diagnose pulmonary embolism, but because it requires a high degree of skill to administer and has potentially serious risks, it's usually performed when other tests fail to provide a definitive diagnosis.
Why is it important to keep on blood thinners?
Because you may be at risk of another deep vein thrombosis or pulmonary embolism, it's important to continue treatment, such as remaining on blood thinners, and be monitored as often as suggested by your doctor. Also, keep regular doctor visits to prevent or treat complications.
How to prepare for a syringe?
You may want to prepare a list that includes: 1 Detailed descriptions of your symptoms 2 Information about your past medical problems, especially any recent surgeries or illnesses that kept you bedridden for several days 3 Details on any recent journeys that involved long car or plane rides 4 All medications you're taking, including vitamins, herbal products and any other supplements, and the dosages 5 Information about the medical problems of parents or siblings 6 Questions you want to ask the doctor
Can a chest X-ray show pulmonary embolism?
Although X-rays can't diagnose pulmonary embolism and may even appear normal when pulmonary embolism exists , they can rule out conditions that mimic the disease.
Where is the catheter used for pulmonary angiogram?
In a pulmonary angiogram, a flexible tube (catheter) is inserted into a large vein — usually in your groin — and threaded through your heart and into the pulmonary arteries . A special dye is then injected into the catheter, and X-rays are taken as the dye travels along the arteries in your lungs.
What tests are done to check for pulmonary embolism?
There are several tests that may be done to diagnose a pulmonary embolism. In addition to a chest X-ray, a ventilation perfusion ( V/Q) scan may be performed to see if anything is blocking blood flow through the lungs. Other tests include CT scan or pulmonary angiography .
What is a pulmonary embolism?
pulmonary embolism: An embolus, usually formed in the leg (sometimes known as a deep vein thrombosis or DVT ), lodges in one of the arteries of the lungs. Many emboli are broken down by the body and go away by themselves; however, serious pulmonary embolism may cause death.
What is an embolus?
The Facts. An embolus is a particle that moves about in our blood vessels, either in the veins or arteries. Most emboli are composed of clotted blood cells. A blood clot is called a thrombus and a moving blood clot is called a thromboembolus. As an embolus moves through the body's blood vessels, it's likely to come to a passage it can't fit through.
What are the risk factors for pulmonary embolism?
Other risk factors for other types of emboli include high blood pressure, atherosclerosis (buildup of fatty plaque in the blood vessels), high cholesterol, and obesity. The primary cause of most pulmonary embolisms is deep vein thrombosis (DVT).
What happens if a blood clot travels to the brain?
brain embolism: If a blood clot travels to the brain, this causes an ischemic stroke or TIA (transient ischemic attack). retinal embolism: Small clots that wouldn't block a major artery can block the smaller blood vessels feeding the retina at the back of the eye.
What happens when an embolus moves through the blood vessels?
As an embolus moves through the body's blood vessels, it's likely to come to a passage it can't fit through. It lodges there, backing up blood behind it. The cells that normally get their blood supply via this passage are starved of oxygen ( ischemia) and die. This condition is called an embolism.
How to prevent DVT?
Non-medication methods to help prevent DVT include using compression devices and compression stockings (to ensure blood doesn't pool in the legs), and frequently stretching, massaging, and moving your lower leg muscles if you are inactive for a long time.
How to treat pulmonary embolism?
How Pulmonary Embolism Is Treated. Treatment is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death. Blood thinners or anticoagulants are the most common treatment for a blood clot in the lung. While hospitalized an injection is used, but ...
How long after pulmonary embolism can you breathe?
If you continue to have breathing difficulty 6 months after a pulmonary embolism you should talk to your doctor and get tested for CTEPH. Your physician may complete a "hypercoagulability" evaluation on you at some point after your diagnosis. This could include blood tests looking for a genetic cause of your DVT.
How long do you have to take blood thinners for lung clots?
Thanks to medical advancements, many patients are good candidates for taking blood thinner tablets which do not require routine monitoring. Patients will normally have to take medications regularly for an indefinite amount of time, usually at least 3 months. However, it is important to work with your doctor to find the best possible treatment for your condition.
What is a clot dissolver?
Clot dissolvers called thrombolytics are a medication reserved for life-threatening situations because they can cause sudden and severe bleeding. For a very large, life-threatening clot, doctors may suggest removing it via a thin, flexible tube (catheter) threaded through your blood vessels.
Can blood thinners dissolve blood clots?
It is important to note that blood thinners won’t dissolve the blood clot. In most cases, the hope is your body will eventually dissolve the clot on its own. If it doesn’t, more drastic measures may need to be taken.
Can pulmonary embolism be life threatening?
Managing Pulmonary Embolism. While a pulmonary embolism can be life-threatening, most patients survive and need to learn how to live with the risk of recurrence.
What is the best treatment for a blood clot in the lung?
Also called “ anticoagulants ,” these are the most common treatment for a blood clot in the lung. They serve two key roles: First, they keep the clot from getting any bigger. Second, they keep new clots from forming. They don’t dissolve blood clots. Your body normally does that on its own over time.
What is the name of the medication that breaks up blood clots?
In life-threatening situations, doctors might use what are called thrombolytic drugs . These quickly break up clots that cause severe symptoms. But they can lead to sudden bleeding and are only used after careful consideration.
What is a PE in a pulmonary artery?
What Is a Pulmonary Embolism? A pulmonary embolism (PE) is a blood clot in the lung that has dislodged from a vein and travels through the bloodsream. It’s serious and can be life-threatening.
What is the best blood thinner?
The most commonly prescribed blood thinners are warfarin ( Coumadin, Jantoven) and heparin. Warfarin is a pill and can treat and prevent clots. You get it through a shot or an IV. There are many other blood thinners in pill form, and your doctor will help decide which agent would work best in your situation.
Where do they insert a tube to remove a clot?
They’ll insert a thin, flexible tube into a vein in your thigh or arm. They’ll continue on to your lung, where they’ll remove the clot or use medicine to dissolve it. Inferior vena cava filter. The inferior vena cava is a large vein that carries blood from the lower body to the heart.
Can blood thinners cause internal bleeding?
Internal bleeding is the main side effect of blood thinners. It can happen if the medicine thins your blood too much. Your doctor may give you blood tests to keep an eye on that. However, even when at therapeutic doses, internal bleeding remains a risk.
What is the treatment for deep venous thrombosis?
Endovascular treatment options include: Catheter-directed thrombolysis (CDT), pharmacomechanical catheter-directed thrombolysis (PCDT), percutaneous aspiration thrombectomy (PAT), vena cava filter protection, venous balloon dilatation and venous stent implantation. Current practice shows strong clinical tendency for the use of PCDT with or without other endovascular methods and an individualized approach for each DVT patient. PMT has not received general acceptance because of the associated risk of PE and damage to venous valves caused by thrombectomy devices. PAT is most commonly used as an adjunctive endovascular technique like balloon maceration to fragment thrombus, balloon angioplasty, stent implantation and vena cava filter placement. Interventional endovascular therapies for DVT have the potential to provide PE protection and prevention of PTS. Patient centered individualized approach for endovascular DVT treatment is recommended to optimize the ideal clinical result.Acute stroke is the leading cause of death for people above the age of 60 and the fifth leading cause in people aged 15-59. Mortality during the first 30 days of ischemic stroke is 20 % and 30 % of survivors will remain permanently disabled. Acute stroke patients within the therapeutic window must receive IVrtPA unless there is a contraindication. In case of contraindication to IVrtPA or for patients out of the therapeutic window for thrombolytics, standart of care is the intraarterial treatment. Patients have to be transferred to a comprehensive stroke center with capacity of dedicated neurovascular imaging and interventional neuroradiology. Noncontrast head CT that is used to rule out hemorrhage is followed by imaging studies dedicated to show if there is reasonable penumbra to save. Intraarterial thrombolysis has the main advantage of extended therapy window, earlier and more efficient recanalization and less risk of hemorrhage due to lower doses of thrombolytics. Mechanical thrombectomy has several advantages over IV/IA fibrinolysis including faster recanalization and less risk of hemorrhage especially in large artery occlusions. ASA guidelines recommend choosing stent retrievers over other devices for mechanical thrombectomy. Better recanalization rates and less infarct volume after mechanical thrombectomy result in higher numbers of functionally independent patients compared with other treatments. Two landmark studies that were published recently, SWIFT PRIME and MR CLEAN, showed that IA treatment especially with the new stent retrievers lead to a significant increase in functional recovery and independence in daily life after an acute stroke.Cerebral venous and sinus thrombosis (CVST) comprises nearly 0.5-1 % of all stroke cases. CVST causes different neurological deficits depending on the sinus/cortical vein involved. CVST may cause death and dependency in 13.4 % of patients. CT/CT venography and MR/MR venography can be effectively used to diagnose and to follow up CVT cases. Anticoagulation with heparin is the most widely accepted therapy to prevent the expansion of the thrombus. Patients deteriorating despite heparinization and patients presenting with very severe neurological deficits must receive endovascular treatment. Endovascular methods include intrasinus infusion of thrombolytics or heparin, balloon angioplasty, mechanical thrombectomy or a combination of different techniques. There is a higher rate or recanalization with endovascular methods compared to other medical therapies.
What is the most widely accepted therapy to prevent the expansion of the thrombus?
Anticoagulation with heparin is the most widely accepted therapy to prevent the expansion of the thrombus. Patients deteriorating despite heparinization and patients presenting with very severe neurological deficits must receive endovascular treatment.
Why is PMT not accepted?
PMT has not received general acceptance because of the associated risk of PE and damage to venous valves caused by thrombectomy devices. PAT is most commonly used as an adjunctive endovascular technique like balloon maceration to fragment thrombus, balloon angioplasty, stent implantation and vena cava filter placement.
Can CVST cause death?
CVST causes different neurological deficits depending on the sinus/cortical vein involved. CVST may cause death and dependency in 13.4 % of patients. CT/CT venography and MR/MR venography can be effectively used to diagnose and to follow up CVT cases.
What is an example of an air embolism?
A pressure gradient is required to drive air into the vascular system; a central line or its tract (post-removal) is an example of such a connection. Often these lines terminate in the superior vena cava where low central venous pressure (CVP) below atmospheric pressure further increases the likelihood of an air embolism.
What is an intravascular air embolism?
An intravascular air embolism (VAE) is a rare, preventable, but serious complication of endovascular procedures resulting in significant morbidity and mortality. It occurs as a result of a pressure gradient that allows air to enter the blood stream, which can subsequently occlude blood flow. This complication can arise in a range of clinical situations including interventional radiology (IR) procedures, trauma, barotrauma, central line placement and removal, and certain types of surgical interventions such as cardiac and neurosurgery. The main causes of systemic and cerebral air embolism are shifting from the traditional culprits of open surgery and trauma to endoscopy, angiography, tissue biopsy, and peripheral venous access [1,2]. While the true incidence of air embolism is unknown, as many instances go unreported, one study included a series of over 11,000 central venous catheter placements and found an incidence of 1 in 772 [3]. As a result of its high chance of mortality and morbidity, physicians should be well equipped to prevent, identify, and manage air embolism. In this article, we explore the clinical presentation of air embolism, review practical tips for prevention and treatment, and present cases of iatrogenic air embolism.
How to conduct invasive arteriography?
When conducting invasive procedures including arteriography, it is important to identify high-risk cases in advance. Use of a continuous flush through a closed system is encouraged. Any wire should be withdrawn from the catheter gradually, while using a syringe to maintain a water seal and incorporating the use of a double flush. In addition, physicians should prepare syringes in batches. This avoids having to draw and then inject and thus allows micro-bubbles to settle. All tubing should be primed with saline and no air should be present in syringes used for hand injections. The syringe should be held upright in order to ensure that any air will travel towards the syringe plunger, away from the catheter (Figure 7). To further ensure that no air is introduced into the catheter, it is recommended that the syringe be connected from wet to wet end. Additionally, it is recommended that the complete volume of the syringe never be completely injected. It should be ensured that balloons for angioplasty are correctly primed and free of air. Air-in-line detection devices incorporated into modern infusion pumps are particularly useful to detect air bubbles in plastic tubing [16]. In surgical procedures where there is a high risk of air embolism, precordial Doppler may be used during anesthesia to allow for early detection of air embolism.
Can an arterial air embolism cause ischemia?
Though the higher intravascular pressure in the arterial system is somewhat protective, arterial air embolism has the potential to produce ischemia or infarction in any organ with limited collateral blood supply, even when the volume of air is small.
Can an air embolism cause seizures?
Clinical symptoms include dyspnea, continuous coughing and chest pain. Neurological symptoms include seizures, loss of consciousness, altered mental status, and hemiparesis/hemiplegia. In many cases, patients may exhibit sudden onset of a combination of signs and symptoms (Figure 4). Although much of the literature discusses arterial infarcts as a result of air embolism, it is worth noting that intravascular air can also cause venous infarcts [9].
Can an air embolism cause hemodynamic disturbance?
Larger air bubbles are also more likely to cause hemodynamic disturbance than smaller air bubbles [7]. With the potential for air embolism to occur almost instantaneously, it is prudent for physicians to take appropriate measures for prevention. It should also be noted that low volume air entering the venous system can often times dissipate and that air emboli can therefore spontaneously resolve on their own with minimal sequelae, (see Figure 1and Figure 2). However, an arterial embolism may be immediately lethal. A case of air embolism is often difficult to diagnose (Figure 3) and oftentimes, the cause of an air embolism cannot be unequivocally determined. This is not unusual since cerebral air embolism is thought to be uncommon. Due to a combination of low overall incidence and some cases where the diagnosis goes undiagnosed [2], an anesthesiologist or intensive care specialist may see only a few or none during their career. A common error is for the air embolism to be misdiagnosed as a thrombotic or thrombo-embolic stroke [8].
When placing catheters, should the CVP be raised?
When placing catheters, the CVP should be raised (to decrease the pressure gradient) by placing the patient in the Trendelenburg position. It should also be ensured that patients are adequately hydrated to prevent hypovolemia and to increase CVP. Avoiding placement of venous catheters during inspiration when negative intra-thoracic pressure is at its maximum is also recommended.
What causes embolisms in the blood?
Embolisms can occur as a result of air bubbles or other gases entering the bloodstream. According to one 2013 journal article, this can be a complication of:
What is the cause of a brain embolism?
Blockages can be caused by a blood clot, fat globule, or air pocket within an artery.
How to prevent stroke?
The best way to prevent a stroke is to receive regular medical checkups and adopt a healthy lifestyle. This includes eating a healthy balanced diet and exercising regularly to maintain a healthy weight.
How long does it take for a stroke to be treated with mechanical thrombectomy?
For the procedure to be successful, a person must receive the treatment within 6 hours of symptom onset.
Can a fat embolism happen after a bone fracture?
Fat from the bone marrow can leak out and enter the bloodstream. This can also happen following bone surgery or after sustaining severe burns.
How to recover from crystal meth addiction?
They have toxic effects on the body that are sometimes fatal. Section Menu. Comprehensive treatment is the best way to recover from crystal meth addiction. The disease can be treated on an inpatient or outpatient basis, depending on the patient’s needs.
What is CBT used for?
CBT was originally designed to treat alcohol addiction, but it is commonly used to treat meth addiction and other substance use disorders. A 2014 study in the journal of Drug and Alcohol Dependence noted good clinical outcomes in people addicted to meth who were treated with CBT.
What are the elements of CBT?
Important elements of CBT include exploring the consequences of meth addiction, recognizing and avoiding high-risk situations and monitoring cravings.
Is it better to go to an inpatient or outpatient program for meth?
Breaking the cycle of addiction and confronting cravings can be difficult when you aren’t in the controlled, drug-free environment of an inpatient program. Outpatient treatment, however, is less disruptive to a person’s life. It is often preferable for people with meth addiction depending on insurance coverage, job constraints and other limitations.
Is there a treatment for meth addiction?
Treatment Options. Currently, the Food and Drug Administration has not approved any medications to treat meth addiction. However, researchers are investigating new medications in clinical trials that may prove useful during detox and recovery.