Medication
A few signs of stage 3 dementia include:
- Getting lost easily
- Noticeably poor performance at work
- Forgetting the names of family members and close friends
- Difficulty retaining information read in a book or passage
- Losing or misplacing important objects
- Difficulty concentrating
Therapy
- Lavender scented: The pleasant lavender fragrance helps promote relaxation.
- Fits into doll clothes: The baby doll easily fits into different doll outfits.
- Weighs 3 lbs.: The weight applies a calming therapeutic pressure for added comfort.
Self-care
a peaceful environment can help calm patients with dementia and is often best achieved in the comfort of their own home surrounded by familiar people. Providing care at home can be stressful for caregivers due to factors such as the need for constant
Nutrition
- Avoid letting the patient take long naps during the day.
- Do not give the patient large amounts of fluid close to bedtime. This can increase nighttime awakening.
- Be sure the room where the patient sleeps is dark, quiet, cool, and comfortable.
How do you feel when caring for patients with dementia?
What is the best therapy for dementia patients?
What is the best home care for dementia patients?
How to handle a combative senior with dementia?
:max_bytes(150000):strip_icc()/GettyImages-149276848-569ff4395f9b58eba4ae1e4e.jpg)
What can you do for a combative dementia patient?
10 tips for dealing with aggressive behavior in dementiaBe prepared with realistic expectations. ... Try to identify the immediate cause or trigger. ... Rule out pain as the cause of the behavior. ... Use a gentle tone and reassuring touch. ... Validate their feelings. ... Calm the environment. ... Play their favorite music.More items...
How do you calm an agitation for dementia?
Here are 10 tips for coping when an older adult with dementia exhibits difficult behaviors.Music. Music therapy helps seniors calm down and reflect on happier times. ... Aromatherapy. ... Touch. ... Pet Therapy. ... A Calm Approach. ... Move to a Secure Memory Care Community. ... Maintain Routines. ... Provide Reassurances.More items...•
What is the best way to combat dementia?
Physical activity. Doing regular physical activity is one of the best ways to reduce your risk of dementia. ... Eating healthily. ... Don't smoke. ... Drink less alcohol. ... Stay mentally and socially active. ... Take control of your health.
At what stage of dementia does aggression occur?
The middle stages of dementia are when anger and aggression are most likely to start occurring as symptoms, along with other worrying habits like wandering, hoarding, and compulsive behaviors that may seem unusual.
What is the best medication for agitation in dementia?
But common ones that can ease agitation include: Medicines that treat paranoia and confusion, called neuroleptics or antipsychotics. Examples of these are aripiprazole (Abilify), haloperidol (Haldol), olanzapine (Zyprexa), quetiapine (Seroquel), risperidone (Risperdal), and ziprasidone (Geodon).
Why do dementia patients get violent?
Some reasons why a person with dementia might be aggressive include: The person might be feeling unheard or misunderstood. The person might be feeling threatened or frightened. The person might be feeling embarrassed, frustrated or annoyed because they need help to do things they used to do independently.
What are the 3 most commonly prescribed drugs for dementia?
Three cholinesterase inhibitors are commonly prescribed:Donepezil (Aricept) is approved to treat all stages of the disease. It's taken once a day as a pill.Galantamine (Razadyne) is approved to treat mild to moderate Alzheimer's. ... Rivastigmine (Exelon) is approved for mild to moderate Alzheimer's disease.
What is Sundowning behavior?
Late afternoon and early evening can be difficult for some people with Alzheimer's disease. They may experience sundowning—restlessness, agitation, irritability, or confusion that can begin or worsen as daylight begins to fade—often just when tired caregivers need a break.
What foods should dementia patients avoid?
The MIND diet specifically limits red meat, butter and margarine, cheese, pastries and sweets, and fried or fast food. You should have fewer than 4 servings a week of red meat, less than a tablespoon of butter a day, and less than a serving a week of each of the following: whole-fat cheese, fried food, and fast food.
What happens to dementia patients who are violent?
Aggressive behaviour in dementia In the later stages of dementia, some people with dementia will develop what's known as behavioural and psychological symptoms of dementia (BPSD). The symptoms of BPSD can include: increased agitation. aggression (shouting or screaming, verbal abuse, and sometimes physical abuse)
At what point do dementia patients need 24 hour care?
During the middle stages of Alzheimer's, it becomes necessary to provide 24-hour supervision to keep the person with dementia safe. As the disease progresses into the late-stages, around-the-clock care requirements become more intensive.
How do you calm a dementia patient who wants to go home?
5 things to remember when someone with dementia is asking to go homeAvoid arguing about whether they are already 'home' ... Reassure them of their safety. ... Try diverting the conversation. ... Establish whether or not they are feeling unhappy or lonely. ... Keep a log of when they are asking to go home. ... 470 comments.
What to do when taking care of a dementia patient?
The most important thing for you to do is keep healthy, both physically and mentally. You will not be an effective caregiver if you get burned out or become sick yourself. If you need a break, find help!
How to calm a dementia patient?
Avoid activities that demand too much thought or concentration. Most dementia patients will become frustrated if they are asked to participate in activities that are too difficult for them to perform. Find activities that the person enjoys. Redirection is one of the best tools available to you.
Why is it important to be prepared for unusual behaviors from dementia patients?
It is essential to be prepared for unusual behaviors from dementia patients. Due to damage occurring in the brain , these patients often display unexpected behaviors.
What are the symptoms of dementia?
Guarding certain areas or withdrawing from touch. Writhing or constant movement. Increase in blood pressure or respiratory rate. Constipation-this can make anyone uncomfortable, including dementia patients. Be sure they follow a toileting schedule and pay attention to the frequency of bowel movements.
How to keep a patient comfortable?
Try to keep the patient comfortable. Maintain a reasonable room temperature and create a good place for the patient to relax.
What causes an aggressive patient to act out?
There are some basic things to rule out when patients begin to act out. Be sure basic needs are met. These include: Pain – uncontrolled pain can cause individuals to lash out. They often are not able to communicate.
What are caregivers trained to recognize?
Caregivers in these facilities are trained to recognize behaviors that require medication.
How to deal with someone with dementia?
Don't Argue: It's never helpful to argue with someone who has Alzheimer's or another dementia. Rather, use distraction or just listen. Remain Calm: Even though you might feel frustrated , your family member will respond better if you stay calm and relaxed.
Why do people with dementia have a catastrophic reaction?
Because of memory loss and confusion, people with dementia might not understand why you're trying to help them and begin to display challenging behaviors. At times, a catastrophic reaction might sometimes be the trigger for combative behavior. A catastrophic reaction is a sudden mood or behavior change that appears to be caused by an over-reaction ...
What is combative behavior?
Combative Behavior is a term often used to describe physical aggression in people with dementia. Combativeness can include hitting, pushing, kicking, spitting, and grabbing. Lucy Lambriex / Getty Images.
Can you argue with someone with Alzheimer's?
Don't Argue: It's never helpful to argue with someone who has Alzheimer's or another dementia. Rather, use distraction or just listen.
How to help dementia patients with confusion?
Simplifying tasks. Break tasks into easier steps and focus on success, not failure. Structure and routine also help reduce confusion in people with dementia.
How to slow the progression of Alzheimer's disease?
Some research also shows that physical activity might slow the progression of impaired thinking in people with Alzheimer's disease, and it can lessen symptoms of depression. Engage in activity. Plan activities the person with dementia enjoys and can do.
How to help a loved one remember upcoming events?
Keep a calendar . A calendar might help your loved one remember upcoming events, daily activities and medication schedules. Consider sharing a calendar with your loved one. Plan for the future. Develop a plan with your loved one while he or she is able to participate that identifies goals for future care.
What tests can be done to determine if a person has a degenerative disease?
Laboratory tests. Simple blood tests can detect physical problems that can affect brain function, such as vitamin B-12 deficiency or an underactive thyroid gland. Sometimes the spinal fluid is examined for infection, inflammation or markers of some degenerative diseases.
What scans show Alzheimer's disease?
CT or MRI. These scans can check for evidence of stroke or bleeding or tumor or hydrocephalus. PET scans. These can show patterns of brain activity and whether the amyloid or tau protein, hallmarks of Alzheimer's disease, have been deposited in the brain.
How to talk to your loved one?
Enhance communication. When talking with your loved one, maintain eye contact. Speak slowly in simple sentences, and don't rush the response . Present one idea or instruction at a time. Use gestures and cues, such as pointing to objects.
Can dementia be cured?
Most types of dementia can't be cured, but there are ways to manage your symptoms.
What journal is "Medication Management for People with Dementia"?
American Journal of Nursing: “Medication Management for People with Dementia.”
What is the chemical that helps prevent dementia?
What they do: Scientists think these help prevent a “messenger chemical” in our brains called acetylcholine from breaking down. Acetylcholine is important in learning, memory, and mood.
What Is Memantine?
If your loved one has moderate to severe Alzheimer’s, their doctor may prescribe them memantine (Namenda) for their symptoms.
What is the chemical that helps us remember?
Memantine helps balance glutamate, which is another “messenger chemical” involved in our memory and learning.
How to help a patient remember to take their medicine?
Make a routine to help them remember to take their medicine. Try to fit the medication schedule to their daily routine. Use a reminder like an alarm clock or a daily phone call to help them remember their medicine when you can't be there.
What happens when you care about dementia?
When someone you care about has dementia, their memory loss is affecting their daily life. You want to find a medication that can help them. There are medicines that can help.
How to keep a list of medications?
Be sure it has the name of everything your loved one takes. This includes prescriptions, vitamins, herbals, and supplements. It should also have the dose for each one and how and when to take it.
What is nonpharmacologic intervention in dementia?
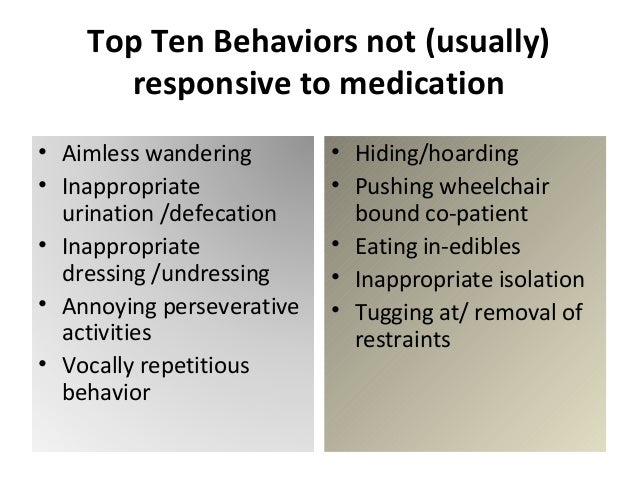
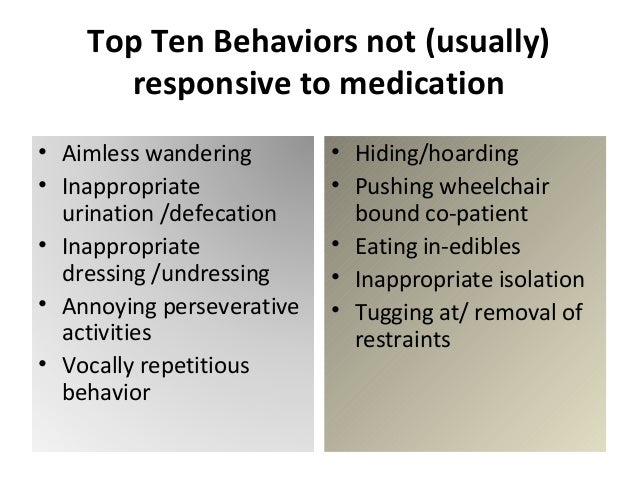
Nonpharmacologic interventions in patients with dementia are often focused on individualizing care and altering personal, behavioral or environmental factors that may contribute to inappropriate behaviors.
How to help dementia patients with agitation?
Sensory stimulation. It is challenging to provide proper stimulation for patients with dementia, and many support the theory that too little or too much stimulation is often an underlying source of agitation and disruptive behavior. Consequently, many studies have investigated the role of music, light and touch, with mixed results. A review of these interventions has found that, of the reported 25% to 54% improvement in agitated behavior, the results were statistically significant in only six of 20 trials. The study designs have been observational, so further studies are needed to confirm the benefits of these alternative interventions as a standard of care (Snowden et al., 2003).
What are the behavioral disturbances of dementia?
Both studies give caregivers and clinicians a framework of common behaviors to anticipate. More importantly, these studies suggest that behavioral disturbances are a central component of dementia and contribute significantly to morbidity. Various treatment modalities, including nonpharmacologic and pharmacologic approaches, have been used in an attempt to decrease the morbidity and mortality associated with behavioral disturbances in patients with dementia.
What is dementia aggression?
Dementia is characterized as a progressive and chronic decline in cognitive function, not limited to memory impairment, which significantly interferes with baseline daily functioning and frequently involves behavioral disturbances.
What is behavioral therapy?
Behavior-based therapy aims to detect situations in which behaviors occur and provide instruction in anticipating and coping with these situations. Both behavioral modification and behavioral therapy have been studied as treatment options for patients with dementia.
Can antipsychotics be used for dementia?
Antipsychotics-acute agitation. Historically, antipsychotics have been prescribed for treating psychosis as well as acutely violent and agitated behavior. The common complication of disruptive behavior in patients with dementia-not limited to aggression and agitation but also psychosis-has led to widespread use of these agents as a long-term treatment in patients with dementia, especially those in the institutional setting. For treating acute behavioral disturbances that pose a risk to patient and staff, it is evident that rapid-acting psychotropics are superior to placebo. A double-blind study of intramuscular olanzapine reported significant results with the use of 2.5 mg and 5 mg at two hours and 24 hours, when compared with placebo (Meehan et al., 2002).
Is antipsychotics a first line treatment for dementia?
Historically, antipsychotics have been first-line treatment for disruptive behavior in patients with dementia.
Why do people with dementia become aggressive?
While scientists do not understand why dementia patients often become aggressive, they do know that Alzheimer's and other forms of dementia profoundly alter the brain.
Can dementia cause hallucinations?
Sometimes patients even experience hallucinations. While some changes in personality may be irremediable, there are some steps you can take to cope with and minimize other behaviors. Common triggers of anger or aggression in dementia patients include:
What is agitation in dementia?
Agitation is a behavioral syndrome characterized by increased, often undirected, motor activity, restlessness, aggressiveness, and emotional distress. According to several observations, agitation prevalence ranges from 30 to 50% in Alzheimer's disease, 30% in dementia with Lewy bodies, 40% in frontotemporal dementia, and 40% in vascular dementia (VaD). With an overall prevalence of about 30%, agitation is the third most common neuropsychiatric symptoms (NPS) in dementia, after apathy and depression, and it is even more frequent (80%) in residents of nursing homes. The pathophysiological mechanism underlying agitation is represented by a frontal lobe dysfunction, mostly involving the anterior cingulate cortex (ACC) and the orbitofrontal cortex (OFC), respectively, meaningful in selecting the salient stimuli and subsequent decision-making and behavioral reactions. Furthermore, increased sensitivity to noradrenergic signaling has been observed, possibly due to a frontal lobe up-regulation of adrenergic receptors, as a reaction to the depletion of noradrenergic neurons within the locus coeruleus (LC). Indeed, LC neurons mainly project toward the OFC and ACC. These observations may explain the abnormal reactivity to weak stimuli and the global arousal found in many patients who have dementia. Furthermore, agitation can be precipitated by several factors, e.g., the sunset or low lighted environments as in the sundown syndrome, hospitalization, the admission to nursing residencies, or changes in pharmacological regimens. In recent days, the global pandemic has increased agitation incidence among dementia patients and generated higher distress levels in patients and caregivers. Hence, given the increasing presence of this condition and its related burden on society and the health system, the present point of view aims at providing an extensive guide to facilitate the identification, prevention, and management of acute and chronic agitation in dementia patients.
What triggers agitation in dementia patients?
Hospitalization is another well-known trigger of agitation either alone or as a manifestation of hyperkinetic delirium in people with dementia ( 41 ).
What is person centered care?
Person-centered care (PCC) is an operating system in healthcare, which considers the health practitioner and the patients as partners in achieving tailored care that meets patients' needs in a unique way ( 67, 68 ). In the PCC framework, the social and historical background, the personality, and the lifestyle of the patients are considered to promote a positive social environment, good compliance, and best outcomes for patients with dementia ( 67, 68 ). The PCC approach is considered a successful option to prevent agitation in home-living and care home patients with dementia ( 69, 70) and reduce antipsychotic use ( 71 ). Nonetheless, not every PCC-based strategy is effective. For instance, the Dementia Care Mapping (DCM) ( 69, 72, 73 ), which is based on patients' systematic observations, has generated conflicting results. In contrast, the Managing Agitation and Raising Quality of Life (MARQUE) intervention ( 74) has failed to improve agitation prevention in care home settings.
What is the NPS in dementia?
The presence of NPS in cognitively normal patients or in patients with mild cognitive impairment (M CI) is associated with an increased risk of progression to overt dementia. The need to identify, in the early stages of the disease, the population at risk of cognitive decline has led to the formulation of the concept of mild behavioral impairment (MBI) ( 34 ). Building on the prior definitions of a pre-dementia risk state ( 35, 36) and frontotemporal-MCI ( 37 ), the ISTAART NPS-PIA formally described MBI as the emergence of sustained and impactful NPS occurring after the age of 50, which are not encompassed in the psychiatric nosology, persist for at least 6 months, and manifest before or at the onset of MCI ( 34 ). Among the NPS associated with MBI, agitation is as frequent as 30%. It is important to understand the prevalence of agitation and impulsivity in pre-dementia syndromes as there is a potential opportunity for early intervention and higher impact in this early stage of disease, even though clinical trials need to be conducted to test and prove that behavioral and pharmacologic treatments in the pre-dementia stage can effectively improve agitation.
How to prevent delirium in hospitalized patients?
Combined strategies are far more adequate to prevent delirium onset, yet not always effective ( 95 ). Careful management of pharmacological therapy, space–time reorientation, early mobilization, minimization of restraint use, and adequate sleep hygiene is the most recommended option for preventing delirium in hospitalized patients ( 42, 96 ). Other options include access to a living room with other patients and the caregiver's presence ( 97 ). Multiple changes of rooms should be avoided ( 98 ).
Is VAD a neurologic condition?
VaD is a neurologic condition due to the occurrence of single or multiple ische mic lesions of the brain ( 166 ). However, risk factors for cerebrovascular injuries also contribute to neurodegenerative disease onset. Rather than a “stand-alone” entity, VaD should be regarded as part of a “Mixed dementia” phenotype, particularly in elderly subjects ( 167 ). In this perspective, we can easily understand why RCTs have a hard time in disentangling VaD from AD (the most common cause of neurodegenerative dementia). Considering this limitation, as well as the lack of recent studies addressing the issue of agitation in VaD, we report the most relevant approaches identified.
Is PCC effective for dementia?
Nonetheless, not every PCC-based strategy is effective.
Diagnosis
Clinical Trials
Lifestyle and Home Remedies
Alternative Medicine
Specialist to consult
Coping and Support
- Diagnosing dementia and its type can be challenging. To diagnose the cause of the dementia, the doctor must recognize the pattern of the loss of skills and function and determine what a person is still able to do. More recently, biomarkers have become available to make a more accurate diagnosis of Alzheimer's disease. Your doctor will review your medical history and symptoms an…
Preparing For Your Appointment
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.