
Medication
For some people, Barrett's esophagus can heal, per Cedars Sinai, though it's typically a permanent condition. Tip If you have severe or frequent GERD symptoms or take heartburn medicine more than twice a week, visit your doctor to get treatment and check for Barrett's esophagus, per the Mayo Clinic.
Procedures
Those who asked “can Barrett’s esophagus be cured?” and find that the answer is “no” can at least take relief in the fact that management and treatment of Barrett’s are possible, and can greatly improve your quality of life.
Therapy
In GERD, stomach contents wash back into the esophagus, damaging esophagus tissue. As the esophagus tries to heal itself, the cells can change to the type of cells found in Barrett's esophagus. However, some people diagnosed with Barrett's esophagus have never experienced heartburn or acid reflux.
Self-care
Barrett’s esophagus does not proceed to cancer in all patients; however, it is estimated that around 10–15% of cases of BE may progress to esophageal cancer. There are two kinds of cell transformations that are associated with either squamous cell or adenocarcinoma of the esophagus.
Nutrition
Does Barretts esophagus ever heal?
Does Barretts esophagus get better?
Can Barrett's esophagus heal itself?
How often does Barrett's turn to cancer?

What is the best treatment for Barrett's esophagus?
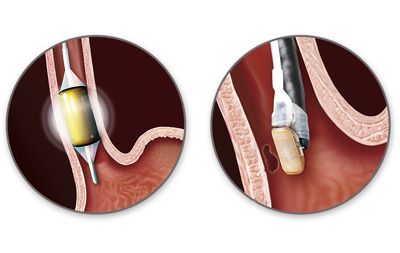
Preferred treatments include: Endoscopic resection, which uses an endoscope to remove damaged cells to aid in the detection of dysplasia and cancer. Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue. Radiofrequency ablation may be recommended after endoscopic resection.
Can Barrett's esophagus be cured?
There is no cure for Barrett's esophagus. Your care plan will try to stop any more damage by keeping acid reflux out of your esophagus.
Is Barrett's esophagus serious?
Barrett's esophagus is a potentially serious complication of GERD, which stands for gastroesophageal reflux disease. In Barrett's esophagus, normal tissue lining the esophagus -- the tube that carries food from the mouth to the stomach -- changes to tissue that resembles the lining of the intestine.
How do you stop the progression of Barrett's esophagus?
Medical and surgical therapy of Barrett's oesophagus is effective in controlling reflux, although not proven to prevent neoplastic progression of the at risk mucosa. Endoscopic techniques of mucosal injury have been applied as alternatives to oesophagectomy in efforts to prevent progression to cancer.
Can omeprazole cure Barrett's esophagus?
Gore and colleagues found that significant but modest regression in the length of the Barrett's segment occurred in 23 patients treated with omeprazole 40 mg daily for up to 2 years. However, no patient had anything approaching complete abolition of the Barrett's segment.
What foods should be avoided with Barrett's esophagus?
Here are some common foods to limit or avoid if you have acid reflux or Barrett's esophagus:alcohol.coffee.tea.milk and dairy.chocolate.peppermint.tomatoes, tomato sauce, and ketchup.french fries.More items...
What are the signs that Barrett's esophagus is getting worse?
The development of Barrett's esophagus is most often attributed to long-standing GERD , which may include these signs and symptoms:Frequent heartburn and regurgitation of stomach contents.Difficulty swallowing food.Less commonly, chest pain.
How often do you need endoscopy for Barrett's esophagus?
Usually, you don't need treatment at this stage. But your healthcare provider will want to monitor the condition. You'll need to have an upper endoscopy every two to three years.
How long can you live with Barrett's Oesophagus?
RESULTS: The mean age at diagnosis of Barrett's esophagus was 61.6 years in males and 67.3 years in females. The mean life expectancy at diagnosis was 23.1 years in males, 20.7 years in females and 22.2 years overall.
What vitamins are good for Barrett's esophagus?
Subjects with Barrett's esophagus will take vitamin D supplementation for 2-12 weeks depending on the severity of their condition, and receive an upper endoscopy procedure before and after vitamin D supplementation trial.
How fast does Barrett's progress?
Barrett esophagus (BE) is a precancerous condition that progresses to high-grade dysplasia (HGD) at an estimated rate of 0.5% to 0.9% per year.
Is Barrett esophagus reversible?
Dr Sarmed Sami advises that Barrett's oesophagus is not reversible by itself, though the majority of patients only need monitoring. The minority of patients with pre-cancerous cells can benefit from removal, such as endoscopic resection (ER) and HALO radiofrequency ablation (RFA).
What is the screening for Barrett's esophagus?
Screening for Barrett's esophagus. Barrett's esophagus has a distinct appearance when viewed during an endoscopy exam. During endoscopy, the doctor passes a flexible tube with a video camera at the tip (endoscope) down your throat and into the swallowing tube (your esophagus).
What is the best way to remove abnormal esophagus tissue?
Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue. Radiofrequency ablation may be recommended after endoscopic resection. Cryotherapy, which uses an endoscope to apply a cold liquid or gas to abnormal cells in the esophagus. The cells are allowed to warm up and then are frozen again.
What is the best treatment for esophageal cancer?
But, given the risk of esophageal cancer, treatment may be recommended if the diagnosis is confirmed. Preferred treatments include: Endoscopic resection , which uses an endoscope to remove damaged cells to aid in the detection of dysplasia and cancer. Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue.
How to treat GERD?
Treatment for GERD. Medication and lifestyle changes can ease your signs and symptoms. Surgery or endoscopy procedures to correct a hiatal hernia or to tighten the lower esophageal sphincter that controls the flow of stomach acid may be an option.
What is the tube that is passed down your throat?
A lighted tube with a camera at the end (endoscope) is passed down your throat to check for signs of changing esophagus tissue. Normal esophagus tissue appears pale and glossy. In Barrett's esophagus, the tissue appears red and velvety. Your doctor will remove tissue (biopsy) from your esophagus. The biopsied tissue can be examined to determine ...
Is Barrett's esophagus a low grade or high grade?
No dysplasia, if Barrett's esophagus is present but no precancerous changes are found in the cells. Low-grade dysplasia, if cells show small signs of precancerous changes. High-grade dysplasia, if cells show many changes. High-grade dysplasia is thought to be the final step before cells change into esophageal cancer.
Can acid back up in the esophagus?
This reinforces the lower esophageal sphincter, making it less likely that acid will back up in the esophagus. High-grade dysplasia is generally thought to be a precursor to esophageal cancer. For this reason, your doctor may recommend endoscopic resection, radiofrequency ablation or cryotherapy.
What is the treatment for Barrett's esophagus?
Gastroenterologists at Johns Hopkins developed the use of cryoablation therapy, an effective treatment for Barrett's esophagus. Ablation therapy may cause Barrett's esophagus to regress. Medications will be given to suppress your stomach acid. Then, during an endoscopy, thermal injury is administered to the abnormal mucous lining.
What is the name of the doctor who treats Barrett's esophagus?
Doctors at Johns Hopkins are at the forefront of diagnosing and treating Barrett's esophagus. In fact, gastroenterologists at Hopkins pioneered the use of cryoablation, a revolutionary new therapy, to treat Barrett's esophagus.
How often do you need an endoscopy for Barrett's?
Patients with low-grade dysplasia may need an endoscopy every three to six months. Patients with high-grade dysplasia may need to undergo an esophagectomy (removal of the esophagus) because of the increased risk of cancer.
What is the goal of surgery for reflux disease?
Some patients prefer a surgical approach as an alternative to a lifetime of taking medications. The goal of surgery for reflux disease is to strengthen the anti-reflux barrier.
What is endoscopic surveillance?
This means that you undergo periodic endoscopic examinations to evaluate whether the condition has evolved into cancer. Your doctor looks for increasing degrees of dysplasia, the abnormal growth of cells, and may perform a biopsy on the area to check for cancerous tissue.
What is Barrett's esophagus?
Barrett’s esophagus is a change in the tissue lining your esophagus, the tube in your throat that carries food to your stomach. For reasons no one understands completely, cells in the esophageal lining sometimes become more like intestinal cells. Researchers suspect that having acid reflux or gastroesophageal reflux disease (GERD) ...
How to diagnose Barrett's esophagus?
How is Barrett's esophagus diagnosed? The only way to confirm the diagnosis of Barrett's esophagus is with a test called an upper endoscopy. This involves inserting a small lighted tube (endoscope) through the throat and into the esophagus to look for a change in the lining of the esophagus.
How to keep esophagus healthy?
The best way to keep the lining of your esophagus healthy is to address heartburn or GERD symptoms. People with ongoing, untreated heartburn are much more likely to develop Barrett’s esophagus. Untreated heartburn raises the risk of esophageal adenocarcinoma by 64 times.
What is the procedure to remove a spot on the esophagus?
Surgery: If you have severe dysplasia or esophageal cancer, your provider may recommend an esophagectomy, a surgery to remove all or part of the esophagus.
What is the most common procedure for esophageal sloughing?
Radiofrequency ablation: This is the most common procedure. It burns off abnormal tissue using radio waves, which generate heat. Cryotherapy: Healthcare providers use liquid nitrogen to freeze diseased parts of the esophagus lining so it will slough off (shed).
Is Barrett's esophagus a precancerous condition?
Barrett’s esophagus is a precancerous condition that may lead to esophageal adenocarcinoma. This type of cancer is rare. Most people with Barrett’s esophagus don’t have to worry — over 90% won’t develop esophageal adenocarcinoma. However, it’s important to monitor the condition.
Does Barrett's esophagus produce symptoms?
How common is Barrett’s esophagus? On its own, Barrett’s esophagus doesn’t produce symptoms. You may discover you have it only after seeing your healthcare provider for gastroesophageal reflux disease (GERD) symptoms or after developing esophageal cancer. Because of the lack of symptoms, no one is sure how common it is.
What is Barrett's oesophagus?
Barrett’s oesophagus means that some cells in the lining of your food pipe have started to change. In a small number of people these cells may develop into oesophageal cancer over a long period of time. The cells lining the food pipe are normally flat. They’re called squamous cells. In Barrett's oesophagus they change into a type more like ...
What is the term for an operation to remove abnormal cells from the lining of the food pipe?
They use a thin wire called a snare put down through the endoscope to remove the inner lining of the oesophagus. This operation is called endoscopic mucosal resection or an EMR.
What is the procedure to strengthen the food pipe valve?
Strengthening the food pipe valve. A surgeon can sometimes strengthen the valve at the lower end of your oesophagus. This operation is called fundoplication. It stops acid from the stomach going back up into the oesophagus and reduces indigestion and heartburn.
How to destroy abnormal cells?
destroying the affected area using radiofrequency ablation (RFA) surgery to remove the area containing the affected cells. other treatments to destroy abnormal cells, such as light therapy (photodynamic therapy) or freezing treatment (cryotherapy)
Can Barrett's oesophagus be diagnosed early?
You’ll need to see your specialist doctor regularly if you have Barrett's oesophagus. You’ll also have regular tests called endoscopies to look inside your food pipe. This checks whether the abnormal cells are developing. It can also pick up oesophageal cancer early when treatment is usually successful.
What is the best treatment for Barrett's esophagus?
Medications used for the treatment of Barrett's esophagus are often available as OTC formulations.
How does Barrett's esophagus affect your lifestyle?
Certain foods and lifestyle factors can affect the disease itself. It is important that you pay attention to the modifications that you can make on your own. Helpful daily habits include: Quitting smoking.
What is the best medicine for acid reflux?
H2 blockers suppress acid production in the stomach. H2 blockers , also called H2-receptor antagonists, are acid-reducing medicines commonly used to treat gastroesophageal reflux disease and esophagitis and to reduce the symptoms of peptic ulcer disease . Commonly used H2 blockers include: Tagamet.
What is the tube used for endoscopy?
Endoscopy is the use of a tube that is placed into your mouth and directed down to your esophagus. The tube is attached to a camera, which allows your medical team to see the appearance of your esophagus from the inside.
How to reduce acid reflux?
Photodynamic therapy: Using light to destroy damaged tissue. In some cases, surgery can be used to narrow the sphincter (opening between the stomach and the esophagus) to reduce acid reflux.
Can Barrett's esophagus be treated?
OTC Therapies & Prescriptions. Surgery and Procedures. Barrett's esophagus can be treated with lifestyle modifications, medications, and surgery. While prevention is undoubtedly important, there are valuable ways to avoid harmful health effects of Barrett's esophagus even if you have already been diagnosed with the condition.
Can you cure Barrett's esophagus?
Over-the-Counter Therapies and Prescriptions. Currently, there are no medications that will cure or reverse Barrett's esophagus. A number of medications can help alleviate your symptoms and may prevent your condition from worsening. Antacids, proton pump inhibitors, and H2 blockers can reduce the reflux (upflow) of stomach acid into the esophagus.
What is the procedure to remove Barrett's esophagus?
The last and final step for treating Barrett's esophagus is the surgical removal of the damaged sections of the esophagus, a procedure called esophagectomy.
What is the best treatment for GERD?
Rabeprazole (AcipHex) Esomeprazole (Nexium) Dexlansoprazole (Dexilant) If GERD symptoms don't respond to medication or if the patient has high-grade dysplasia, the doctor may recommend an endoscopic procedure to remove or destroy the abnormal cells or dysplasia. The approach depends on the patient and how far the Barrett's esophagus has progressed.
What are the symptoms of Barrett's esophagus?
The development of Barrett's esophagus is most often attributed to long-standing GERD, which may include these signs and symptoms: Frequent heartburn and regurgitation of stomach contents. Difficulty swallowing food. Less commonly, chest pain.
What are the factors that increase the risk of Barrett's esophagus?
Factors that increase your risk of Barrett's esophagus include: Family history. Your odds of having Barrett's esophagus increase if you have a family history of Barrett's esophagus or esophageal cancer. Being male. Men are far more likely to develop Barrett's esophagus. Being white.
What is the valve between the esophagus and the stomach called?
Between the esophagus and the stomach is a critically important valve, the lower esophageal sphincter (LES). Over time, the LES may begin to fail, leading to acid and chemical damage of the esophagus, a condition called gastroesophageal reflux disease (GERD). GERD is often accompanied by symptoms such as heartburn or regurgitation.
What causes the lining of the esophagus to thicken?
Barrett's esophagus is a condition in which the flat pink lining of the swallowing tube that connects the mouth to the stomach (esophagus) becomes damaged by acid reflux, which causes the lining to thicken and become red. Between the esophagus and the stomach is a critically important valve, the lower esophageal sphincter (LES).
What to do if you have heartburn and reflux?
If you've had trouble with heartburn, regurgitation and acid reflux for more than five years, then you should ask your doctor about your risk of Barrett's esophagus. Seek immediate help if you: Have chest pain, which may be a symptom of a heart attack. Have difficulty swallowing.
Can Barrett's esophagus cause cancer?
Fortunately, most people with Barrett's esophagus will never develop esophageal cancer. By Mayo Clinic Staff. Barrett's esophagus care at Mayo Clinic.
Can proton pump inhibitors cause Barrett's esophagus?
Chronic heartburn and acid reflux. Having GERD that doesn't get better when taking medications known as proton pump inhibitors or having GERD that requires regular medication can increase the risk of Barrett's esophagus. Current or past smoking. Being overweight.
Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Specialist to consult
Preparing For Your Appointment