
Procedures
The definitive treatment for cardiac tamponade is removal of the accumulated pericardial fluid. This is performed by employing one of these techniques: Medical and surgical procedures Tricuspid aortic valve repair or replacement Pericardial window Pericardiocentesis
Self-care
Aug 04, 2021 · The treatment of cardiac tamponade is pericardiocentesis. During this procedure, a needle is advanced through the chest wall into the pericardium. The procedure may be done blindly or with guidance from ultrasonography or fluoroscopy. Hemodynamically unstable patients warrant the use of pericardiocentesis without imaging.
Why is cardiac tamponade so dangerous?
Dec 21, 2021 · The treatment of cardiac tamponade is the removal of pericardial fluid to help relieve the pressure surrounding the heart. This can be done by performing a needle pericardiocentesis at the bedside, performed either using traditional landmark technique in a sub-xiphoid window or using a point-of-care echo to guide needle placement in real-time.
Is cardiac tamponade considered serious?
Conclusion: Acute cardiac tamponade can be efficiently treated by pericardiocentesis with subsequent continuous negative pressure drainage via a pigtail catheter. Our retrospective analysis shows a significantly lower mortality, a decreased rate of interventions and lower rates of cardiac re-tamponade without any relevant side effects when compared to classical …
What are the signs and symptoms of cardiac tamponade?
Apr 25, 2022 · Cardiac tamponade is an uncommon but severe medical condition that can result in shock or death. It is vital that anyone who suspects that they have cardiac tamponade seek emergency treatment. The...
What are the differential diagnoses for cardiac tamponade?
Treatment. Cardiac tamponade is an emergency condition that needs to be treated in the hospital. The fluid around the heart must be drained as quickly as possible. A procedure that uses a needle to remove fluid from the tissue that surrounds the heart will be done.
What is the definitive treatment for cardiac tamponade?
Removal of pericardial fluid, with or without echocardiographic guidance, is the definitive therapy for tamponade and can be done using the following 3 methods.Nov 28, 2018
What is cardiac tamponade what are known causes and treatments?
What is the nursing intervention for cardiac tamponade?
Is cardiac tamponade an emergency?
How do paramedics treat cardiac tamponade?
What are the three signs of cardiac tamponade?
- low blood pressure in the arteries.
- muffled heart sounds.
- swollen or bulging neck veins, called distended veins.
How do you empty pericardial drains?
Can a nurse perform a pericardiocentesis?
How is pericardial tamponade diagnosed?
- Physical exam: This will include taking your pulse, blood pressure and checking your breathing. ...
- Echocardiogram: This test uses ultrasound waves to see inside your chest and heart. ...
- Chest X-ray: An X-ray can show fluid buildup around your heart.
What does cardiac tamponade look like on ECG?
How long can you live with fluid around your heart?
Can fluid around the heart go away on its own?
What causes a tamponade in the heart?
Causes of Cardiac Tamponade 1 Malignancy “cancerous” spread 2 End-stage renal disease: a condition in which your kidneys have stopped working well and your body retains fluid. 3 Viral, bacterial, fungal or parasitic infections 4 Idiopathic “no known cause” pericarditis 5 Sharp or blunt chest trauma 6 Thyroid disease: a condition that is caused by the over or under function of the thyroid gland. The thyroid gland is an essential organ for producing thyroid hormones, which maintains the body’s metabolism. 7 Autoimmune disease: a condition in which your immune system mistakenly attacks your body (e.g. lupus, rheumatoid arthritis and scleroderma). 8 Invasive heart/lung surgical procedures 9 Rupture of an aortic aneurysm
How to tell if you have a tamponade?
Common symptoms of cardiac tamponade include: 1 Chest pain or pressure 2 Shortness of breath 3 Heart palpitations 4 Lightheadedness/Fainting 5 Confused or impaired thinking 6 Nausea and/or vomiting 7 Decreased urine output 8 Anxiety 9 Swelling of the legs or abdomen
What is the space between the heart and the pericardium?
The heart is surrounded by a double-layered sac called the pericardium. Between these two layers, there is a space known as the pericardial cavity. The pericardial cavi ty normally contains a small amount of pericardial fluid. This fluid prevents friction between the two layers and helps your heart move easier within the sac.
Why does the pericardium stretch?
A normal pericardium can stretch to accommodate increases in pericardial volume, with the stretch amount related to how quickly the effusion develops. Regardless, ongoing accumulation of pericardial fluid into a closed space will eventually lead to an increase of the intra-pericardial pressure. When the intra-pericardial pressure becomes too ...
What does it mean when you feel drowsy?
The acute onset of these symptoms could indicate the early stages of pericardial effusion, cardiac tamponade, or of another cardiac-related condition.
What are the symptoms of tamponade?
They may endorse vague symptoms of chest pain, palpitations, shortness of breath, or in more severe cases, dizziness, syncope, and altered mental status.
What is the result of tamponade?
Cardiac tamponade results from the rapid filling of fluid within the pericardium, leading to compression of the chambers of the heart, further resulting in decreased venous return, ventricular filling and decreased cardiac output.
What is pericarditis in the pericardium?
Pericarditis is a common disorder caused by inflammation of the pericardium. Acute pericarditis was reported in 5% of patients admitted to the emergency department[1] and 0.1% to 0.2% of hospitalized patients[2] for non-ischemic chest pain.
What is the pericardium?
Introduction. The pericardium is a membrane surrounding the heart. It comprises an outer fibrous pericardium and an inner double-layered serous pericardium. Serous pericardium includes visceral layer and parietal layers, separated by the pericardial cavity containing 15 to 50 ml of plasma ultra-filtrate in healthy people.
Can pericarditis be treated with NSAIDs?
Acute pericarditis often responds to treating the underlying cause. High-dose NSAIDs, with or without colchicine, tapered down over weeks is the first-line treatment. High dose aspirin (ASA) should be used in the post-myocardial infarction Dressler syndrome.
What is the role of a physician assistant in pericarditis?
Their role includes medication adjustment, follow up at the pericardial clinic.
Can aspirin be used for Dressler syndrome?
High dose aspirin (ASA) should be used in the post-myocardial infarction Dressler syndrome. The response is often assessed clinically based on symptom relief. Corticosteroids are not recommended as first-line therapy in most patients as it can increase the risk of recurrent pericarditis.
What is a cardiac tamponade?
Cardiac tamponade is a medical emergency that takes place when abnormal amounts of fluid accumulate in the pericardial sac compressing the heart and leading to a decrease in cardiac output and shock. This activity describes the evaluation and management of cardiac tamponade and reviews the role of the interprofessional team in improving care ...
What causes tamponade in the heart?
Cardiac tamponade is caused by the buildup of pericardial fluid (exudate, transudate, or blood) that can accumulate for several reasons. Hemorrhage, such as from a penetrating wound to the heart or ventricular wall rupture after an MI, can lead to a rapid increase in pericardial volume.
What is a tamponade?
Cardiac tamponade is a medical or traumatic emergency that happens when enough fluid accumulates in the pericardial sac compressing the heart and leading to a decrease in cardiac output and shock.
What are the symptoms of tamponade?
They may endorse vague symptoms of chest pain, palpitations, shortness of breath, or in more severe cases, dizziness, syncope, and altered mental status.
Can tamponade cause shortness of breath?
Patients with cardiac tamponade present similar to patients with other forms of cardiogenic or obstructive shock. They may endorse vague symptoms of chest pain, palpitations, shortness of breath, or in more severe cases, dizziness, syncope, and altered mental status.
Can you use positive pressure ventilation for tamponade?
If possible, positive pressure mechanical ventilation should be avoided as it may further decrease venous return and aggravate the symptoms. The treatment of cardiac tamponade is the removal of pericardial fluid to help relieve the pressure surrounding the heart.
How long does it take for a tamponade to die?
The key is the timing of intervention; the longer the delay, the worse the outcomes. Patients with tamponade caused by malignant disease have death rates exceeding 75% within 12 months.
What is cardiac tamponade?
Cardiac tamponade is an uncommon but severe medical condition that can result in shock or death. It is vital that anyone who suspects that they have cardiac tamponade seeks emergency treatment.
What causes tamponade in the heart?
A buildup of fluid around the heart muscles causes cardiac tamponade. Image credit: Blausen.com staff, 2014. Cardiac tamponade results from the buildup of fluid between the layers of the pericardium. In acute cardiac tamponade, this fluid accumulation occurs quickly, while it happens slowly in subacute cardiac tamponade.
Is tamponade a medical emergency?
If the level of fluid builds up quickly, it can be life-threatening. Doctors consider cardiac tamponade to be a medical emergency. In this article, we discuss the causes and symptoms of cardiac tamponade.
What are the symptoms of tamponade?
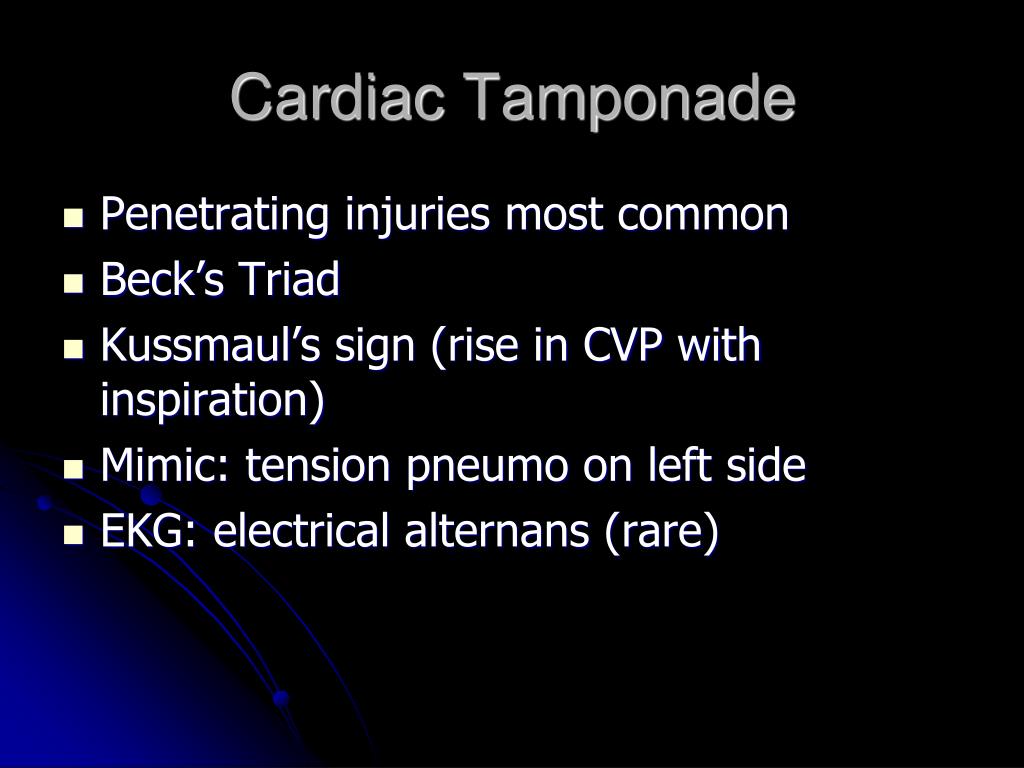
As a result, blood does not circulate properly, which can lead to chest pains and lightheadedness . The three classic signs of cardiac tamponade, which doctors refer to as Beck’s triad, are: low blood pressure in the arteries.
How to tell if you have a tamponade?
People with cardiac tamponade may also experience the following symptoms: a weak pulse. bluish skin that is cool to the touch. lightheadedness. a rapid heart rate. fainting. drowsiness. anxiety. sharp pain in the chest, back, abdomen, or shoulder.
How to diagnose tamponade?
To diagnose cardiac tamponade, a doctor will look for Beck’s triad of medical signs. They will do this by checking the individual’s blood pressure, listening to their heart, and examining the appearance of their veins. The doctor is likely to carry out additional tests to support their diagnosis. These may include:
Is tamponade fatal?
Prompt diagnosis and early treatment significantly improve the outlook for people with cardiac tamponade. Without treatment, the condition is fatal.
What is a tamponade in the heart?
Cardiac tamponade is pressure on the heart that occurs when blood or fluid builds up in the space between the heart muscle and the outer covering sac of the heart.
Can tamponade come back?
The outcome is often good if the condition is treated promptly. However, tamponade may come back.
Why does the heart not get enough blood?
This prevents the heart ventricles from expanding fully. The excess pressure from the fluid prevents the heart from working properly. As a result, the body does not get enough blood.
What are the symptoms of a swollen chest?
Symptoms. Symptoms may include: Anxiety, restlessness. Sharp chest pain that is felt in the neck, shoulder, back, or abdomen. Chest pain that gets worse with deep breathing or coughing. Problems breathing. Discomfort, sometimes relieved by sitting upright or leaning forward. Fainting, lightheadedness.
What is chest pain?
Sharp chest pain that is felt in the neck, shoulder, back, or abdomen. Chest pain that gets worse with deep breathing or coughing. Problems breathing. Discomfort, sometimes relieved by sitting upright or leaning forward.
What is the normal heart rate for a stethoscope?
Rapid breathing. Heart rate over 100 (normal is 60 to 100 beats per minute) Heart sounds are only faintly heard through a stethoscope. Neck veins that may be bulging (distended) but the blood pressure is low. Weak or absent peripheral pulses.
What is the procedure to remove fluid from the heart?
A procedure that uses a needle to remove fluid from the tissue that surrounds the heart will be done. A surgical procedure to cut and remove part of the covering of the heart (pericardium) may also be done.
