
What is tomotherapy®?
Metastatic breast cancer patients live longer with improvement in systemic treatment and radiotherapy/ tomotherapy for metastatic sites. The survival rate at 5 years has increased from 10% in 1970 to about 40% in women treated after 1995 (Giordano et al., 2004). Clinicians have to address the issue whether or not to remove the primary cancer in the breast at some stage, …
How likely is cancer to respond to treatment?
Tomotherapy for Prostate Cancer Treatment. Radiation therapy is an important part of treatment for many men with prostate cancer. Conventional radiation treatment, which delivers a wide beam of radiation, is highly effective in destroying cancer cells. The wide beam, however, can also damage healthy tissue near a cancerous tumor.
What is tomotherapy for prostate cancer?
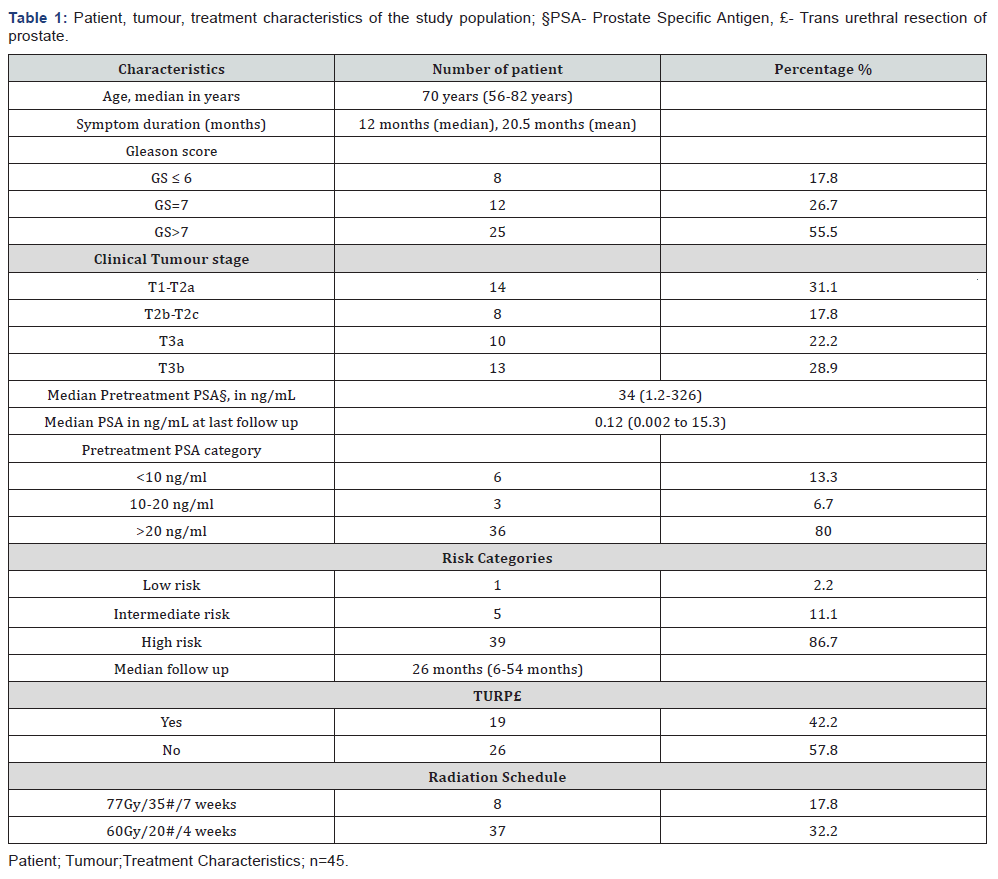
Aim of the study: Helical tomotherapy is one of the methods of radiotherapy. This method enables treatment implementation for a wide spectrum of clinical cases. The vast array of therapeutic uses of helical tomotherapy results directly from the method of dose delivery, which is significantly different from the classic method developed for conventional linear accelerators.
What is the TomoTherapy Hi-Art system ®?
The TomoTherapy® System is among the most revolutionary radiotherapy innovations in the history of cancer treatment, completely redefining the standard for individualized and precise treatment of tumors anywhere in the body — while creating a new paradigm for patient comfort and quality of life. The first truly complete IGRT/IMRT solution, TomoTherapy combines …
What is the success rate of Tomotherapy?
Overall survival in the conventional radiotherapy (RT) group and the helical tomotherapy group. The 1- and 2-year overall survival rates were 93.9% and 87.1% for the conventional RT group, 96.6% and 96.6% for the helical tomotherapy group, respectively (p = 0.095).
How long does it take for SBRT to work?
Most people getting SBRT don't have any skin changes during treatment. You may notice skin changes 4 to 6 weeks after you finish treatment.Dec 12, 2018
What is the difference between Tomotherapy and radiotherapy?
In general, radiation therapy (or radiotherapy) has developed with a strong reliance on homogeneity of dose throughout the tumor. Tomotherapy embodies the sequential delivery of radiation to different parts of the tumor which raises two important issues.
How long does it take for radiation therapy to work?
How long does radiation therapy take to work? Radiation therapy does not kill cancer cells right away. It takes days or weeks of treatment before cancer cells start to die. Then, cancer cells keep dying for weeks or months after radiation therapy ends.
What is the success rate of SBRT?
SBRT has shown dramatically better outcomes than conventional radiation therapy. Whereas two-year success rates for conventional treatment range from 30 to 40 percent, the success rates for SBRT range from 80 to 90 percent — comparable to those of resection surgery but with far fewer risks.
How is SBRT delivered?
SBRT is delivered through devices called linear accelerators, which form beams of fast-moving subatomic particles. Why Am I Hearing So Much About CyberKnife? CyberKnife is a brand name for one of several available stereotactic radiosurgery devices that deliver radiation with linear accelerators.
How is a TomoTherapy done?
TomoTherapy® is a new way to deliver radiation treatment in the fight against cancer. The process combines treatment planning, CT image-guided patient positioning and treatment delivery into one integrated system. The equipment used for TomoTherapy® looks much like a computed tomography (CT) system.
When do you use TomoTherapy?
What Is TomoTherapy Used For? TomoTherapy's accuracy, modulation and 360-degree delivery make it ideal for tumors that are hard to reach or next to vital organs. It's also used to treat multiple tumors at once and re-treat areas, with fewer side effects.
Is TomoTherapy a type of IMRT?
Tomotherapy is a type of intensity-modulated radiation therapy (IMRT). Also called helical tomotherapy.
How many sessions of radiotherapy is normal?
Most people have 5 treatments each week (1 treatment a day from Monday to Friday, with a break at the weekend). But sometimes treatment may be given more than once a day or over the weekend.
Do tumors grow back after radiation?
Normal cells close to the cancer can also become damaged by radiation, but most recover and go back to working normally. If radiotherapy doesn't kill all of the cancer cells, they will regrow at some point in the future.Jul 6, 2020
Is radiation worse than chemo?
Since radiation therapy is focused on one area of your body, you may experience fewer side effects than with chemotherapy. However, it may still affect healthy cells in your body. Side effects of radiation may include: digestive issues like nausea, vomiting, stomach cramps, diarrhea.Mar 27, 2020
What is tomotherapy used for?
Tomotherapy has been used for the treatment of benign brain tumors (meningiomas and neurinomas), resulting in good target coverage with high-dose homogeneity and respecting organs-at-risk constraints. 164 In addition, this technique allows treatment of larger brain lesions than GKS.
What is helical tomotherapy?
Helical tomotherapy unit is a new modality for radiation treatments, the first dedicated to intensity-modulated irradiation using a fully integrated image-guided radiotherapy machine with on-board megavoltage CT capability . The tomotherapy system (see Fig. 104-4) uses a 6-megavoltage accelerator, and a 64-leaf binary multileaf collimator and xenon image detector array mounted on a rotating gantry. Radiation is delivered in a helical way, obtained by concurrent gantry rotation and couch/patient movements. Altogether, these components allow continuous, intensity-modulated rotational irradiation with fan beam entry from 360 degrees. A megavoltage CT scan before the treatment (nominal energy of 3.5 megavoltages) can be fused with a planning CT scan to determine the correct patient setup every time that the radiotherapist needs to check it. Finally, ultimate dose calculation is refined by means of convolution/superimposition. Tomotherapy has been used for the treatment of benign brain tumors (meningiomas and neurinomas), resulting in good target coverage with high-dose homogeneity and respecting organs-at-risk constraints. 164 In addition, this technique allows treatment of larger brain lesions than GKS. Once again the most important difference seems to be that the latter still maintains a better conformity index, and non-negligible advantages in terms of the integral dose to the brain.
What is the purpose of the ionotherapy trial?
The purpose of the trial is to provide patients with a shorter course, dose intense and non-invasive radiotherapy treatment with equivalent or improved CNS control, survival, quality of life and toxicity. Other clinical trials using alternative radiotherapy platforms are also accruing patients ( www.clinicaltrials.gov ).
Why are some beams not compliant with standard protocols?
Some beams are not compliant with standard protocols because they do not have a flat dose profile (e.g., TomoTherapy or flattening filter free beams), which complicates reference dosimetry. 12. In addition, the size of the detector must be appropriate for the beam.
What is TomoTherapy Hi Art System?
Both of these concerns are greatly reduced with the TomoTherapy Hi-Art System ®, the latest evolution of radiation therapy for the treatment of prostate and other forms of cancer. Froedtert & the Medical College of Wisconsin were the first in southeast Wisconsin to install TomoTherapy, and are among fewer than 100 health care facilities in the country using this advanced technology.
What is IMRT radiation?
IMRT is an advanced form of radiation therapy. IMRT breaks a radiation beam into hundreds of tiny beams that enter the body from many angles to intersect the tumor. A computer calculates the precise radiation doses to deliver to a tumor or specific areas within the tumor.
Does TomoTherapy work?
This means faster, more effective treatment with fewer side effects than with conventional radiation therapy. TomoTherapy enables doctors to selectively destroy tumors in the prostate gland with higher doses of radiation while reducing exposure to surrounding structures, such as the rectum and bladder.
Can a wide beam of radiation damage a tumor?
The wide beam, however, can also damage healthy tissue near a cancerous tumor. In addition, on any given day, the prostate gland and the tumors inside can move, affecting the precision of the radiation treatment.
Can you get a tumor back after treatment?
If a tumor returns after treatment, some patients can be treated again with TomoTherapy because of the precise nature of technology. The system enables such finely tuned dose delivery that even previously irradiated areas can be treated again.
What is the TomoTherapy system?
The TomoTherapy® System is among the most revolutionary radiotherapy innovations in the history of cancer treatment, completely redefining the standard for individualized and precise treatment of tumors anywhere in the body — while creating a new paradigm for patient comfort and quality of life. The first truly complete IGRT/IMRT solution, TomoTherapy combines integrated CT imaging for exceptional treatment accuracy with a first-of-its-kind helical treatment delivery platform that uses patented beam-shaping technology to precisely target tumors while minimizing impact on surrounding healthy tissue. Ongoing investment in radiotherapy innovation enhances the trusted and proven platform, as Accuray continues to elevate imaging and beam-shaping capabilities to new levels.
What is a fully integrated CT?
Fully integrated CT imaging enables IGRT/IMRT and 3D CRT with a uniquely seamless workflow that allows clinicians to focus on patients first. The unique helical treatment delivery technology and beam-shaping multileaf collimator (MLC) empowers treatment teams to confidently deliver precise radiation therapy anywhere in the body.
