Medication
Can bacterial vaginosis go away on its own? BV will often go away on its own within a few days, but it also tends to come back. If you take antibiotics to treat BV, the symptoms may disappear within a day or two, but it’s important to take the full course of pills, which is usually seven days.
Self-care
While initial cure rates for bacterial vaginosis (BV) approach 80%, 2 out of 3 women experience a recurrence within 6 months of treatment. Since BV is not currently considered a sexually transmitted infection, treatment guidelines do not include treating partners of women with BV.
Nutrition
Clindamycin isn’t practical because you’re not treating the cause of bacterial vaginosis; you’re only treating the frustrating symptoms you’re experiencing. Another problem you’ll find with using clindamycin to treat bacterial vaginosis is that some women are allergic to this antibiotic.
Can BV go away on its own?
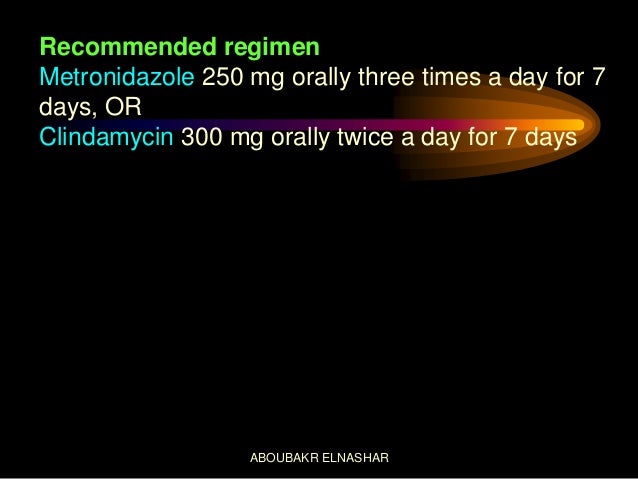
Treatment. To treat bacterial vaginosis, your doctor may prescribe one of the following medications: Metronidazole (Flagyl, Metrogel-Vaginal, others). This medicine may be taken as a pill by mouth (orally). Metronidazole is also available as a topical gel that you insert into your vagina.
Should partners of women with bacterial vaginosis be treated?
Does clindamycin really treat bacterial vaginosis?
What is the best medicine for vaginal bacteria?
Does bacterial vaginosis need to be treated in pregnancy?
In summary, women with bacterial vaginosis during pregnancy should be aggressively evaluated and effectively treated. This is particularly true for women considered at high risk for pregnancy-related complications. Asymptomatic pregnant women with bacterial vaginosis may also benefit from therapy.
Can I take metronidazole for BV while pregnant?
Metronidazole, a nitroimidazole derivative, is a recommended treatment during pregnancy for bacterial vaginosis (BV) and infections with Trichomonas vaginalis (8, 9). Preterm birth has been associated with both BV and T.
Can I take metronidazole 500mg while pregnant?
You can use metronidazole while you're pregnant.
Is Flagyl contraindicated in pregnancy?
Metronidazole is used to treat genitourinary infections and is one of the most commonly used drugs in pregnancy, but it is widely thought to be relatively contraindicated in the first trimester because of a possible increased risk for birth defects.
Is metronidazole safe in pregnancy 2nd trimester?
Use of metronidazole, a common treatment for bacterial vaginosis and Trichomonas vaginalis, should be avoided during the second trimester of pregnancy in this population.
What category is metronidazole in pregnancy?
US FDA pregnancy category: Not assigned. Risk summary: No controlled data available on use of this drug in pregnant women to inform a drug-related risk.
Can BV harm baby during delivery?
Bacterial vaginosis (BV) during pregnancy is a well-established risk factor for preterm birth and other preterm pregnancy complications. Little is known about adverse neonatal outcomes associated with BV exposure in full-term births, nor its influence on adverse outcomes independent of its effect on gestational age.
How to diagnose BV?
BV can be diagnosed by using clinical criteria (i.e., Amsel’s diagnostic criteria) ( 999) or by determining the Nugent score from a vaginal Gram stain ( 1000 ). Vaginal Gram stain, considered the reference standard laboratory method for diagnosing BV, is used to determine the relative concentration of lactobacilli (i.e., long gram-positive rods), small gram-negative and gram-variable rods (i.e., G. vaginalis or Bacteroides ), and curved gram-negative rods (i.e., Mobiluncus) characteristic of BV. A Nugent score of 0–3 is consistent with a Lactobacillus -predominant vaginal microbiota, 4–6 with intermediate microbiota (emergence of G. vaginalis ), and 7–10 with BV. Clinical diagnosis of BV by Amsel criteria requires at least three of the following four symptoms or signs:
What is the best test for BV?
In addition to the Amsel criteria, multiple POC tests are available for BV diagnosis. The Osom BV Blue test (Sekisui Diagnostics) detects vaginal sialidase activity ( 1003, 1004 ). The Affirm VP III (Becton Dickinson) is an oligonucleotide probe test that detects high concentrations of G. vaginalis nucleic acids (>5 x 10 5 CFU of G. vaginalis/ mL of vaginal fluid) for diagnosing BV, Candida species, and T. vaginalis. This test has been reported to be most useful for symptomatic women in conjunction with vaginal pH measurement and presence of amine odor (sensitivity of 97%); specificity is 81% compared with Nugent. Finally, the FemExam Test Card (Cooper Surgical) measures vaginal pH, presence of trimethylamine (a metabolic by-product of G. vaginalis ), and proline aminopeptidase ( 1005 ). Sensitivity is 91% and specificity is 61%, compared with Nugent. This test has primarily been studied in resource-poor settings ( 1005 ), and although it has been reported to be beneficial compared with syndromic management, it is not a preferred diagnostic method for BV diagnosis.
What is the Max Vaginal Panel?
The Max Vaginal Panel provides results by an algorithmic analysis of molecular DNA detection of Lactobacillus species ( L. crispatus and L. jensenii) in addition to G. vaginalis, A. vaginae, BVAB2, and Megasphaera type 1. This test has 90.5% sensitivity and 85.8% specificity for BV diagnosis, compared with Amsel criteria and Nugent score. It also provides results for Candida species and T. vaginalis. The Aptima BV detects G. vaginalis, A. vaginae, and certain Lactobacillus species including L. crispatus, L. jensenii, and L. gasseri, with sensitivity and specificity ranging from 95.0% to 97.3% and 85.8% to 89.6%, respectively (using either clinician- or patient-collected vaginal swabs). The three laboratory-developed tests (NuSwab VG, OneSwab BV Panel PCR with Lactobacillus Profiling by qPCR, and SureSwab BV) have to be internally validated before use for patient care yet have good sensitivity and specificity, similar to FDA-cleared assays. BV NAATs should be used among symptomatic women only (e.g., women with vaginal discharge, odor, or itch) because their accuracy is not well defined for asymptomatic women. Despite the availability of BV NAATs, traditional methods of BV diagnosis, including the Amsel criteria, Nugent score, and the Affirm VP III assay, remain useful for diagnosing symptomatic BV because of their lower cost and ability to provide a rapid diagnosis. Culture of G. vaginalis is not recommended as a diagnostic tool because it is not specific. Cervical Pap tests have no clinical utility for diagnosing BV because of their low sensitivity and specificity.
Can BV be used during pregnancy?
BV treatment is recommended for all symptomatic pregnant women because symptomatic BV has been associated with adverse pregnancy outcomes , including premature rupture of membranes, preterm birth, intra-amniotic infection, and postpartum endometritis ( 989, 991, 1036 ). Studies have been undertaken to determine the efficacy of BV treatment among this population, including two trials demonstrating that oral metronidazole was efficacious during pregnancy by using the 250 mg 3 times/day regimen ( 1037, 1038 ); however, oral metronidazole administered as a 500 mg 2 times/day regimen can also be used. One trial involving a limited number of participants revealed treatment with oral metronidazole 500 mg 2 times/day for 7 days to be equally effective as metronidazole gel 0.75% for 5 days, with cure rates of 70% by using Amsel criteria to define cure ( 1039 ). Another trial demonstrated a cure rate of 85% by using Gram-stain criteria after treatment with oral clindamycin 300 mg 2 times/day for 7 days ( 1040 – 1043 ).
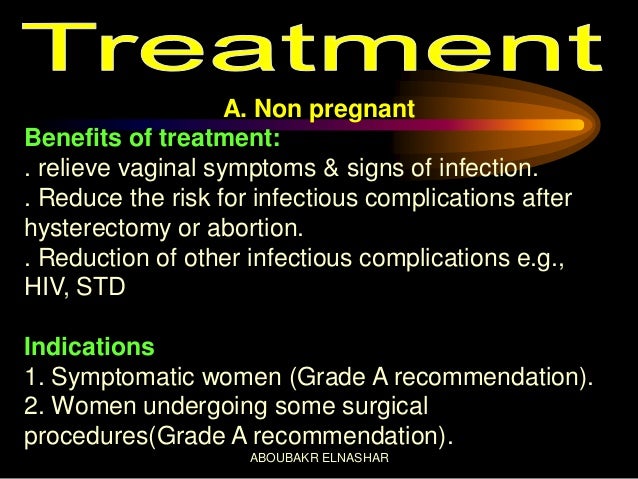
Is BV treatment recommended for women?
Treatment for BV is recommended for women with symptoms. Established benefits of therapy among nonpregnant women are to relieve vaginal symptoms and signs of infection. Other potential benefits of treatment include reduction in the risk for acquiring C. trachomatis, N. gonorrhoeae, T. vaginalis, M. genitalium, HIV, HPV, and HSV-2 ( 971, 986 – 988, 990, 1010 ). No data are available that directly compare the efficacy of oral and topical medications for treating BV.
Can you douch for BV?
Douching might increase the risk for relapse , and no data support use of douching for treatment or symptom relief.
Should women with BV be tested for HIV?
All women with BV should be tested for HIV and other STIs.
How to cure BV during pregnancy?
Bacterial vaginosis treatment during pregnancy is mostly based on the restoration of pH of the vagina. Vaginal pH correction treatment: This brings us to the next cure for BV during pregnancy. Vaginal washes and pH neutral soaps help correct the altered pH of the vagina.
What causes bacterial vaginosis during pregnancy?
Bacterial Vaginosis (BV) during pregnancy occurs due to the imbalance of good and bad bacteria in the vagina.
What is bacterial vaginosis?
Bacterial vaginosis during pregnancy is the condition of having an outbreak of harmful bacteria in the vagina area.
Why does BV cause spotting?
Bacterial vaginosis spotting: Bacterial vaginosis spotting is due to the tearing of vaginal walls. BV during pregnancy can spread to the uterus and causes tearing of membranes. It can result in vaginal bleeding and passing of vaginal tissue. Spotting is the most important symptom of BV during pregnancy.
Why is a condom used during pregnancy?
Using a condom is the only way to prevent bacterial vaginosis during pregnancy due to unprotected sex.
What does it mean when your vagina is grayish white?
Gray whitish discharge: Unlike yeast infection, you will not exude the thick cheesy discharge. If you have bacterial vaginosis, your vaginal discharge will be grayish white. The discharge has a fishy smell. The smell of discharge during pregnancy bacterial vaginosis heightens when you have sex.
Why does my vagina feel wet?
One reason for BV during pregnancy is the excessive amount of moisture present near the vagina. During early pregnancy vaginal discharge increases and makes you feel wet.
Can bacterial vaginosis be cured?
BV will sometimes go away without treatment. But if you have symptoms of BV you should be checked and treated. It is important that you take all of the medicine prescribed to you, even if your symptoms go away. A health care provider can treat BV with antibiotics, but BV may recur even after treatment.
Resources for Clinicians
Vaginitis Self-Study Module external icon – An online learning experience that helps users learn how to manage vaginitis. Free CME/CNE available. (November 1, 2017)
What is the best medicine for bacterial vaginosis?
To treat bacterial vaginosis, your doctor may prescribe one of the following medications: Metronidazole (Flagyl, Metrogel-Vaginal, others). This medicine may be taken as a pill by mouth (orally). Metronidazole is also available as a topical gel that you insert into your vagina.
How to diagnose bacterial vaginosis?
Open pop-up dialog box. Close. Pelvic examination. Pelvic examination. In a pelvic exam, your physician inserts two gloved fingers inside your vagina. While simultaneously pressing down on your abdomen, he or she can examine your uterus, ovaries and other organs. To diagnose bacterial vaginosis, your doctor may: ...
How long does it take for bacterial vaginosis to recur?
It's common for bacterial vaginosis to recur within three to 12 months, despite treatment. Researchers are exploring treatments for recurrent bacterial vaginosis. If your symptoms recur soon after treatment, talk with your doctor about treatments. One option may be extended-use metronidazole therapy.
How to boost the number of good bacteria in your vagina?
A self-help approach is lactobacillus colonization therapy — which attempts to boost the number of good bacteria in your vagina and re-establish a balanced vaginal environment — possibly accomplished by eating certain types of yogurt or other foods containing lactobacilli.
How long does Clindamycin last in vagina?
This medicine is available as a cream that you insert into your vagina. Clindamycin cream may weaken latex condoms during treatment and for at least three days after you stop using the cream. Tinidazole (Tindamax). This medication is taken orally.
Can bacterial vaginosis spread between male and female partners?
It's generally not necessary to treat an infected woman's male sexual partner, but bacterial vaginosis can spread between female sexual partners. Female partners should seek testing and may need treatment. It's especially important for pregnant women with symptoms to be treated to help decrease the risk of premature delivery or low birth weight.
What to do if you have a yeast infection while pregnant?
If the diagnosis of a yeast infection is confirmed by a medical professional, it is likely they will either suggest an over the counter treatment, or they may prescribe oral medication, antifungal creams, or suppositories. Read more about dealing with yeast infections during pregnancy.
What are the different types of vaginal infections?
Four types of vaginitis include trichomoniasis, yeast infections, bacterial vaginosis, and atrophic vaginitis. This article will focus on the two types most pertinent to pregnant women: yeast infections and bacterial vaginosis.
What is BV discharge?
Bacterial vaginosis (BV) (also known as nonspecific vaginitis) is caused by several different types of bacteria. Many women don’t experience any symptoms, but some may develop a white or grayish, fishy-smelling discharge. In some cases, the discharge may also appear frothy.
Can bacterial vaginosis be treated naturally?
Unfortunately, bacterial vaginosis cannot be treated naturally. It is important to take action and contact your healthcare provider because bacterial vaginosis has been associated with preterm delivery, low-birth-weight infants, preterm/pre-labor membrane rupture, and late-term miscarriages.
Can pregnant women get vaginal inflammation?
Treating vaginitis naturally during pregnancy is a frequent concern for expecting mothers. Vaginitis is a general term for the inflammation of the vagina. Vaginitis is common but can be very annoying as it tends to be reoccurring and may interfere with sexual intercourse.
Is there a foolproof way to protect against yeast infection?
While there is evidence to suggest that these natural treatments may aid in the prevention of yeast infections, there is no foolproof way to entirely safeguard yourself against infection.
Who is most susceptible to a bacterial infection?
Those who are most susceptible to these infections are pregnant women, women with diabetes, women taking antibiotics, corticosteroid medications, or oral contraceptives ( birth control pills ), and/or women with iron deficiencies.