What is the correct treatment for syncope?
To immediately treat someone who has fainted from vasovagal syncope, help the person lie down and lift their legs up in the air. This will restore blood flow to the brain, and the person should quickly regain consciousness. The person should lie down for a little while afterwards.
What are the initial orders for a patient with history of syncope?
Patients presenting with syncope should have orthostatic blood pressure measurements and standard 12-lead electrocardiography. Laboratory and imaging studies should be ordered for patients with syncope only if clinically indicated by the history and physical examination.
How is pre syncope treated?
How Is Presyncope Treated?Being careful when you stand up.Raising the head of your bed while you're sleeping.Medications.Discontinuing or changing existing medications.Avoiding the situations that cause your presyncope.Treating any heart conditions you may have.A pacemaker, if needed.More items...•
What makes syncope an emergency?
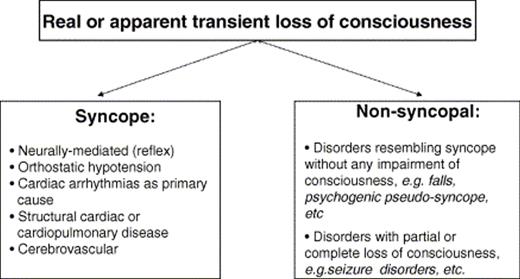
Syncope is defined as a transient loss of consciousness due to cerebral hypoperfusion with spontaneous return to baseline function without intervention. It is a common chief complaint of patients presenting to the emergency department.
Is syncope a medical emergency?
Syncope, also known as faint, is a temporary loss of consciousness and balance usually related to insufficient blood flow to the brain. The majority of syncope patients are those whose the autonomic nervous system (Vasovagal Syncope) works unusually.
What are the 4 classifications of syncope?
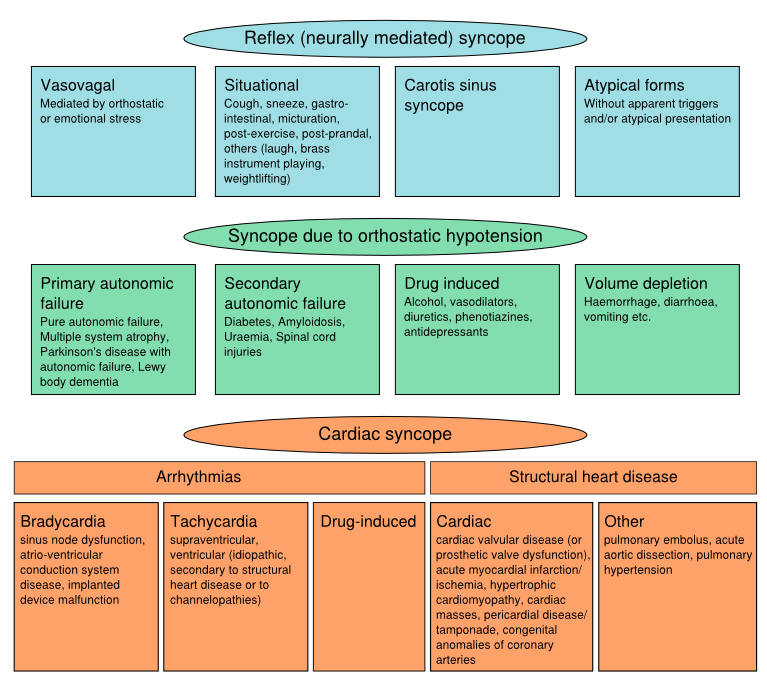
Syncope is classified as neurally mediated (reflex), cardiac, orthostatic, or neurologic (Table 1).
What is the most common cause of syncope?
Syncope is a temporary loss of consciousness usually related to insufficient blood flow to the brain. It's also called fainting or "passing out." It most often occurs when blood pressure is too low (hypotension) and the heart doesn't pump enough oxygen to the brain.
What is the difference between syncope and presyncope?
Basically, presyncope (pre-sin-co-pee) is the sensation that you're going to faint. You might feel lightheaded and weak, among other symptoms, but you don't actually pass out. You typically feel better within a few minutes. If you do faint and regain consciousness, that's called syncope.
What is the first step in evaluating a patient for syncope?
In the evaluation of patients with syncope, the critical first step is a detailed medical history. A diagnostic strategy based on initial evaluation is warranted. The importance of the initial evaluation goes well beyond its capability to make a diagnosis as it determines the most appropriate subsequent diagnostic pathways and risk evaluation.
When is situational syncope diagnosed?
Situational syncopeis diagnosed if syncope occurs during or immediately after urination, defaecation, cough or swallowing.
What happens if a diagnosis is confirmed?
If the diagnosis is confirmed, treatment may be initiated; if not, a reappraisal process may be useful.
What is the diagnostic strategy based on?
THE DIAGNOSTIC STRATEGY BASED ON THE INITIAL EVALUATION
Can neurally mediated syndromes be evaluated?
If cardiac evaluation does not show evidence of arrhythmia as a cause of syncope, evaluation for neurally‐mediated syndromes is recommended only in those with recurrent or severe syncope. It includes tilt testing, carotid sinus massage, and ECG monitoring, and often further requires implantation of an implantable loop recorder (ILR). The majority of patients with single or rare episodes in this setting have a high likelihood of neurally‐mediated syncope and tests for confirmation are usually not necessary.
Can ischaemia be diagnosed with syncope?
Cardiac ischaemia‐related syncopeis diagnosed when symptoms are present with ECG evidence of acute ischaemia with or without myocardial infarction. However, in this case further determination of the specific ischaemia‐induced aetiology may be necessary (for example, neurally‐mediated hypotension, tachyarrhythmia, ischaemia‐induced atrioventricular block, etc).
Can seizures cause syncope?
Neurologic disease may cause transient loss of consciousness (for example, certain seizures), but is almost never the cause of syncope. Thus, neurologic testing may be needed to distinguish seizures from syncope in some patients, but these should not be considered as essential elements in the evaluation of the basis of true syncope. The possible contribution of electroencephalography (EEG), computed tomography and magnetic resonance imaging of the brain is to disclose abnormalities caused by epilepsy; there are no specific EEG findings for any loss of consciousness other than epilepsy. Accordingly, several studies conclusively showed that EEG monitoring was of little use in unselected patients with syncope. Thus, EEG is not recommended for patients in whom syncope is the most likely cause for a transient loss of consciousness. Carotid TIAs are not accompanied by loss of consciousness. Therefore, carotid Doppler ultrasonography is not required in patients with syncope.4
What is considered a pre-syncope?
Getting an injection or having blood drawn (not considered serious) Standing up quickly (a "head rush" is considered pre-syncope) Standing upright for a long time. Sudden and unexpected trauma, stress or pain, such as being hit. Blood donation.
Why does syncope occur?
Syncope occurs when there is not enough blood flow to the brain. There are many potential causes, but the most common ones include:
What is the most common form of reflex syncope?
Vasovagal syncope — the common faint — occurs in one third of the population. It is by far the most common form of reflex syncope. Vasovagal syncope is often triggered by a combination of dehydration and upright posture. But it can also have an emotional trigger such as seeing blood ("fainting at the sight of blood").
What is reflex syncope?
Reflex Syncope (Neurally Mediated Syncope, Vasovagal Syncope, Vasodepressor Syncope, the Common Faint) Reflex syncope is the result of a reflex response to some trigger, in which the heart slows or blood vessels dilate (widen). This causes blood pressure to drop, so less blood flows to the brain and fainting (syncope) or near-fainting (pre-syncope) ...
What is situational syncope?
Situational syncope, a sudden reflex response to a trigger other than those listed above. Triggers include:
What causes syncope in the heart?
Common causes of cardiac syncope: Arrhythmia and abnormal heart rhythm: During episodes of heart arrhythmia, the heart works inefficiently and not enough oxygenated blood can circulate to the brain. There are many types of cardiac arrhythmias that may cause syncope.
What is post-micturition syncope?
Urinating ( post-micturition syncope: occurs in men while standing to urinate) Eating a meal. Sudden abdominal pain. Blowing a brass instrument or lifting weights. Carotid Sinus Syncope, a response in older adults that occurs when pressure is applied to the carotid artery in the neck.
What is the best treatment for autonomic mediated syncope?
Various medications have been used to treat Autonomic Mediated Syncope (Neurocardiogenic Syncope, Vasovagal Syncope). Beta blockers (Antihypertensive and antianginal drugs) such as Bisoprolol at low dose can be effective.
How to avoid syncope?
• Avoid situations likely to induce syncope – for example, standing in a queue, taking a long hot bath, eating a large carbohydrate-rich meal in a warm restaurant, or failing to drink sufficient fluid in a hot nightclub.#N#• Take immediate action at the first warning of an impending collapse. If a collapse is imminent lie down flat propping your legs up on a chair or against a wall or sit down with your head between your knees. Squatting down on ones heels can be very effective and is less likely to attract attention in public . All these manoeuvres help reverse venous pooling of blood in the limbs, swiftly restoring blood flow to the brain and alleviating symptoms. When sufficiently recovered get up carefully. If your symptoms return or worsen squat down, or lie down again.
How to prevent vasovagal syncope?
It may also be helpful in preventing vasovagal syncope. Ensuring adequate intake, as determined by the clear appearance of urine, may help prevent collapses. • Increase your dietary intake of salt if your oral intake is low – 24 hour urinary sodium excretion is a proxy measure.
Which is the strongest drug for autonomic mediated syncope?
SSRIs and Midodrine currently have the strongest scientific evidence. The fact that so many different medications are used in the treatment of Autonomic Mediated Syncope (Neurocardiogenic Syncope, Vasovagal Syncope) indicates that none is entirely effective. Sometimes, a combination of drugs is required.
Is autonomic mediated syncope benign?
Reassurance about the benign nature of Autonomic Mediated Syncope (Neurocardiogenic Syncope, Vasovagal Syncope), avoidance of situations likely to induce an attack, and use of simple non-drug counter-measures is often all that is required in the management of the condition. However, treatment with low dose medication may be necessary. Occasionally pacemaker implantation may be required.
What tests are needed for syncope?
Other tests, such as exercise stress test, Holter monitor and an echocardiogram, may be needed to rule out other cardiac causes. An ECG also is recommended for children and young adults with syncope. Other noninvasive diagnostic testing may be needed if they're suspected of having congenital heart disease, cardiomyopathy or a heart rhythm disorder. ...
What are the signs of syncope?
People who experience the warning signs of fainting of dizziness, nausea and sweaty palms should sit or lie down. Anyone with syncope should receive an initial evaluation, including detailed physical and history examinations and measurement of blood pressure and heart rate, by a physician.
What causes syncope in the heart?
Cardiac or cardiovascular syncope is caused by various heart conditions, such as bradycardia, tachycardia or certain types of hypotension . It can increase the risk of sudden cardiac death. People suspected of having cardiac syncope but who don't have serious medical conditions may be managed as outpatients.
What is the cause of NMS?
It happens when the part of the nervous system that regulates blood pressure and heart rate malfunctions in response to a trigger, such as emotional stress or pain.
Can heart failure cause syncope?
If evaluation suggests cardiac vascular abnormalities, an ambulatory external or implantable cardiac monitor may be required. Heart failure, atrial fibrillation and other serious cardiac conditions can cause recurrent syncope in older adults, with a sharp increase after age 70.
Can other disorders cause syncope?
Other disorders can cause syncope, which also can be a side effect of some medicines.
Can you drive after a syncope?
When it comes to driving after a syncope episode, there are no restrictions for VVS patients who had no fainting spells in the previous year. Still, it may be helpful for healthcare providers to discuss regional driving laws, restrictions and implications with all patients.
What is the best medicine for vasovagal syncope?
A drug called fludrocortisone acetate that's normally used to treat low blood pressure may be helpful in preventing vasovagal syncope. Selective serotonin reuptake inhibitors also may be used. Therapies. Your doctor may recommend ways to decrease the pooling of blood in your legs.
How to diagnose vasovagal syncope?
Diagnosis. Diagnosing vasovagal syncope often begins with a physical examination. During the physical exam, your doctor will listen to your heart and take your blood pressure. He or she may also massage the main arteries in your neck to see if that causes you to feel faint. Your doctor may also recommend several tests to rule out other possible ...
What tests are done to see if you have a fainting spell?
Blood tests. Your doctor may look for conditions, such as anemia, that can cause or contribute to fainting spells. Tilt table test. If no heart problems appear to cause your fainting, your doctor may suggest that you undergo a tilt table test.
What is the best test for fainting?
Echocardiogram. This test uses ultrasound imaging to view the heart and look for conditions, such as valve problems, that can cause fainting.
How to tell if you're fainting?
What you can do 1 Write down details of your symptoms, including any triggers that may have caused you to faint. 2 Make a list of any medications, vitamins and supplements you're taking. 3 Write down questions you want to ask your doctor, including questions about potential tests and treatments.
Can a pacemaker help with syncope?
Surgery. Very rarely, inserting an electrical pacemaker to regulate the heartbeat may help some people with vasovagal syncope who haven't been helped by other treatments.
What is the best treatment for syncope?
Simple reassurance, proper hydration, anticipatory guidance, safety precautions, and increased salt intake are helpful for common type fainting (vasovagal syncope) especially in children and young adults. Insertion of a pacemaker is the standard treatment for syncope caused by a slow heartbeat (bradycardia).
Why do I get syncope?
It may be explained by factors such as stress, grief, overheating, dehydration, painful stimuli, exhaustion, or illness. Profound blood loss or fluid loss (severe diarrhea or vomiting) may also cause syncope. Many causes of syncope, however, are not easy to explain and are not serious.
What is the most dangerous type of fainting?
Cardiovascular syncope - The most dangerous but rare type of fainting is caused by an abnormal heart rhythm (arrhythmia) or by structural damage to the heart. Non-cardiovascular syncope - The most common type (also called vasovagal type). There are a variety of causes not necessarily related to the heart.
How do you know if you have a heart attack or a syncope?
Cardiovascular syncope is usually sudden. There may be no warning signs that an individual is about to faint. Some people do feel the following: Shortness of breath. Heart palpitations (feeling like your heart is racing, pounding, or fluttering) Pain, pressure, tightness, or discomfort in the chest. Loss of consciousness.
What are the risk factors for cardiovascular syncope?
Risk Factors for Cardiovascular Syncope. The risk of cardiovascular syncope increases with age. Those at greatest risk are people who have any of the following conditions: Coronary artery disease (clogged blood vessels to the heart) Chest pain caused by angina (lower blood supply to the heart)
Can syncope be stopped?
Depending on the diagnosis, cardiovascular syncope may be stopped or controlled with one or more of the following therapies:
Does syncope increase with age?
The risk of cardiovascular syncope increases with age. Cardiovascular syncope usually is sudden. There may be no warning signs that an individual is about to faint.
When does syncope occur?
Most episodes of syncope occur either in early adulthood or after the age of 70.
What is the most common cause of syncope?
Vasovagal. This type of presyncope is caused by a drop in blood flow to your brain due to low blood pressure. This is the most common cause of syncope and presyncope. It's usually caused by a combination of being dehydrated and standing or sitting up too quickly. Vasovagal presyncope can also have emotional triggers such as:
What is situational presyncope?
Situational presyncope is another type of vasovagal presyncope. This occurs when you have a reflex response to a specific trigger. Your heart may slow or your blood vessels may widen. This causes a drop in your blood pressure, decreasing blood flow to your brain.
What causes neurologic presyncope?
Other, less common causes of neurologic presyncope include migraines and normal pressure hydrocephalus (NPH), which is a type of brain disorder. Postural orthostatic tachycardia syndrome ( POTS ).
What is it called when your blood vessels get smaller?
Orthostatic hypotension. This is also a type of vasovagal syncope or presyncope. When you stand, your blood vessels normally get smaller to keep blood from collecting in your legs. This doesn't happen in people with orthostatic hypotension.
How to treat heart problems?
Treating any heart conditions you may have. A pacemaker, if needed. Wearing compression stockings to help your circulation. Changing your diet, which may mean consuming more salt or potassium, eating smaller meals more frequently, drinking more fluids, or avoiding caffeine and alcohol.
Can a pacemaker cause presyncope?
Other types of heart arrhythmias, or abnormal rhythms, can also cause presyncope. Cardiac presyncope or syncope can be caused by problems with a pacemaker. They might also indicate a tear in the large artery that carries blood to the rest of your body.