Explore
(Conditional Recommendation; Evidence Level: Grade C) Physicians may offer patients with stress urinary incontinence and concomitant neurologic disease affecting lower urinary tract function (neurogenic bladder) surgical treatment of stress urinary incontinence after appropriate evaluation and counseling have been performed. (Expert Opinion)
When is surgery indicated in the treatment of stress urinary incontinence?
There is a wide spectrum of treatment options available for patients with symptomatic stress urinary incontinence (SUI). Strong opinions exist as to the “best” nonsurgical and surgical therapies for this condition. However, the perfect therapy for SUI has not yet been identified (Table 1).
What are the treatment options for stress urinary incontinence (SUI)?
Physicians may offer patients with stress urinary incontinence and concomitant neurologic disease affecting lower urinary tract function (neurogenic bladder) surgical treatment of stress urinary incontinence after appropriate evaluation and counseling have been performed. (Expert Opinion)
Should physiotherapists treat stress urinary incontinence and neurogenic bladder?
In the initial evaluation of patients with stress urinary incontinence desiring to undergo surgical intervention, physicians should include the following components: (Clinical Principle) History, including assessment of bother Physical examination, including a pelvic examination
What is included in the initial evaluation of stress urinary incontinence?

What is the best surgery for stress incontinence?
Colposuspension involves making a cut in your lower tummy (abdomen), lifting the neck of your bladder, and stitching it in this lifted position. If you have a vagina, a colposuspension can help prevent involuntary leaks from stress incontinence.
What is a surgery of choice in a major part of patients with stress urinary incontinence?
When considering a primary surgical correction of stress urinary incontinence women should be informed that, according to current available evidence, a retropubic procedure provides the best assurance of a durable cure. (I-A). 2. Some surgeons offer laparoscopic Burch as an alternative to the open Burch.
What is stress urinary incontinence treatment?
Behavior therapies may help you eliminate or lessen episodes of stress incontinence. The treatments your doctor recommends may include: Pelvic floor muscle exercises. Your provider or physical therapist can help you learn how to do Kegel exercises to strengthen your pelvic floor muscles and urinary sphincter.
What is the surgery for overactive bladder?
Augmentation cystoplasty increases the size of your bladder. It's often used in severe cases when other treatments have failed. During the procedure, your surgeon will take a small piece of tissue from your intestine and add it to the wall of your bladder. This enables your bladder to store more urine.
Is there surgery for urinary incontinence?
The Burch procedure, the most common suspension surgery, adds support to the bladder neck and urethra, reducing the risk of stress incontinence.
Is there surgery for male incontinence?
Urethral Sling Surgery The male sling procedure is a minimally invasive surgical solution for male stress incontinence. This procedure involves the placement of a soft sling of mesh to reposition the urethra and provide support to surrounding muscles.
Can stress incontinence be cured without surgery?
No matter where a person is along the spectrum of urinary incontinence, it's not a pleasant condition. The good news is that for most people, simple lifestyle changes and/or medical treatment can ease the discomfort of incontinence, or even stop it altogether, without having to resort to surgery.
What is the pathophysiology of stress incontinence?
Stress incontinence occurs when the muscles and other tissues that support the urethra (pelvic floor muscles) and the muscles that control the release of urine (urinary sphincter) weaken. The bladder expands as it fills with urine.
What are the main causes of stress incontinence?
Risk factors for stress incontinence include:Pregnancy and childbirth (particularly vaginal birth).Menopause.Nerve injuries to the pelvis or lower back.Obesity.Pelvic surgery, such as a hysterectomy.Chronic coughing.Diabetes.Surgery for prostate cancer or an enlarged prostate (benign prostatic hyperplasia).More items...•
What is bladder suspension surgery?
Bladder suspension surgery, also known as bladder neck suspension, is a procedure that is used to treat stress incontinence in women. There are a variety of types of bladder suspension surgeries that use stitches to support the bladder and urethra.
Is stress incontinence surgery covered by insurance?
Will my insurance cover stress incontinence surgery? Most insurance plans, including Medicare, cover these procedures.
What factors should be considered before surgery?
Some factors you should consider before deciding whether to undergo surgery include: the severity of your SUI symptoms and their effect on your daily activities; your desire for future pregnancy as vaginal delivery can cause recurrence of SUI symptoms, which could require future surgery.
What is SUI in a sneeze?
Stress urinary incontinence (SUI) is a leakage of urine during moments of physical activity that increases abdominal pressure, such as coughing, sneezing, laughing, or exercise.
What are the risk factors for SUI?
Other risk factors for SUI include chronic coughing or straining, obesity and smoking. It is important for you to consult with your health care provider for proper diagnosis of SUI. Image Source: National Kidney and Urologic Diseases Information Clearinghouse. Back to top.
Can you use mesh slings for SUI?
Ask your surgeon about all SUI treatment options, including non-surgical options and surgical options that do and do not use mesh slings. It is important for you to understand why your surgeon may be recommending a particular treatment option to treat your SUI.
What is a sling for incontinence?
Sling procedures to treat stress incontinence. A sling is a piece of human or animal tissue or a synthetic tape that a surgeon places to support the bladder neck and urethra. Two sling techniques are shown — the retropubic and transobturator. Both are designed to reduce or eliminate stress incontinence in women.
Where is the surgical incision?
To perform the procedure, your surgeon makes an incision in your lower abdomen or performs the surgery through small incisions using thin instruments and a video camera (laparoscopic surgery). Your surgeon secures stitches (sutures) in the tissue near the bladder neck.
What is bladder neck suspension?
Bladder neck suspension. Bladder neck suspension adds support to the bladder neck and urethra, reducing the risk of stress incontinence. The surgery involves placing sutures in vaginal tissue near the neck of the bladder — where the bladder and urethra meet — and attaching them to ligaments near the pubic bone.
How long does it take to recover from bladder neck suspension?
For bladder neck suspension performed abdominally, you'll need general or spinal anesthesia. Recovery takes several weeks, and you might need to use a urinary catheter until you can urinate normally. Recovery time is likely to be shorter with laparoscopic surgery.
Is urinary incontinence surgery invasive?
Urinary incontinence surgery is more invasive and has a higher risk of complications than do many other therapies, but it can also provide a long-term solution in severe cases. The surgical options available to you depend on the type of urinary incontinence you have.
Can you use stitches to attach a tension free sling?
No stitches are used to attach the tension-free sling, which is made from a strip of synthetic mesh tape. Instead, body tissue holds the sling in place. Eventually scar tissue forms in and around the mesh to keep it from moving. For a tension-free sling procedure, your surgeon may use one of three approaches:
Can you have surgery for stress urinary incontinence?
If you have severe symptoms of stress urinary incontinence or overactive bladder, surgery may provide a permanent solution to your problems. But surgery isn't for everyone. Find out what procedures may help in treating urinary incontinence.
What is a sui?
What is Stress Urinary Incontinence (SUI)? Stress Urinary Incontinence (SUI) is when urine leaks out with sudden pressure on the bladder and urethra, causing the sphincter muscles to open briefly . With mild SUI, pressure may be from sudden forceful activities, like exercise, sneezing, laughing or coughing.
What is UDS in medical terms?
Urodynamic studies (UDS) are done to test how well the bladder, sphincters and urethra hold and release urine. Once your provider understands the type of incontinence you have and rules out other conditions, he/she will offer you treatment options to feel better.
How many women with SUI have OAB?
Urinary incontinence increases with age. Over half of women with SUI also have OAB. About one-third (1 out of 3) of women age 60 find that they sometimes leak urine. About half (1 out of 2) of women age 65 and above find that they sometimes leak urine.
What is the purpose of a urinalysis?
A urinalysis or urine sample to test for a urinary tract infection or blood in the urine. A bladder scan after urinating to show how much urine stays in your bladder after you urinate. A Cystoscopy uses a narrow tube with a tiny camera to see into the bladder to rule out more serious problems.
What is the urinary tract?
The urinary tract includes two kidneys, two ureters, a bladder, aurethra and a sphincter. The bladder is secured in place by fascia in the pelvic floor. This system works together to store and remove waste, specifically urine, from our bodies. The kidneys make urine.
How long does it take for a balloon to refill a urethral cuff?
This opens your urethra and you can urinate. Once urination is complete, the balloon reservoir automatically refills the urethral cuff in 1-3 minutes. Artificial sphincter surgery can cure or greatly improve urinary control in more than 7 out of 10 men with SUI. Results may vary in men who have had radiation treatment.
What is UI in medical terms?
What is urinary incontinence (UI)? A person who is affected by urinary incontinence (UI), loses control of their urinary sphincter, the two muscles which control the passage of urine into the bladder, resulting in an involuntary leakage of urine. UI is a symptom of other conditions, rather than a medical condition in its own right.
How to diagnose UI?
To diagnose UI, a doctor will review a person’s medical history, carry out urinalysis; an analysis of the composition of the person’s urine; and urodynamic testing; tests which ascertain the function of the individual’s urinary system. Doctors who specialise in problems related to the urinary system are called urologists.
What is UI in urination?
People affected by urinary incontinence (UI), experience loss of control over their urinary system. This can result in many different kinds of difficulties related to urinating, ranging from involuntary leakage to becoming unable to fully empty the bladder during urination. UI can be transient:
Why does UI affect females?
Because of the differences between the sexes in terms of pelvic and genital structure and the way the genitalia are connected to the urinary system , UI generally affects females and males differently in terms of the type of UI experienced, and for different reasons.
Why do men have UI?
UI primarily occurs in males because of developing problems with nerve function, such that the brain no longer sends signals to the bladder effectively. This can include suffering from a stroke or a spinal cord injury (SCI), both of which affect the nervous system, interrupting the transmission of the nerve signals required for control of the urinary sphincter. Those who are affected by problems related to the prostate gland are also at risk of experiencing UI.
Why are women more likely to get UI than men?
Women are more likely to experience UI than men because they are, physiologically, more likely to undergo bodily changes which compromise the normal function of the urinary system. Women can be affected by all types of UI and at any age. However, UI in women is primarily associated with ageing and with natural biological processes.For example, UI often accompanies pregnancy and also commonly affects women during or after they experience the stages of menopause.
What is the most common type of UI?
The most common types of UI are stress incontinence, i.e.placing stress on the bladder during involuntary physical activities, such as sneezing or laughing causes an involuntary release of urine, and urge incontinence, which is a sudden and uncontrollable need to urinate.
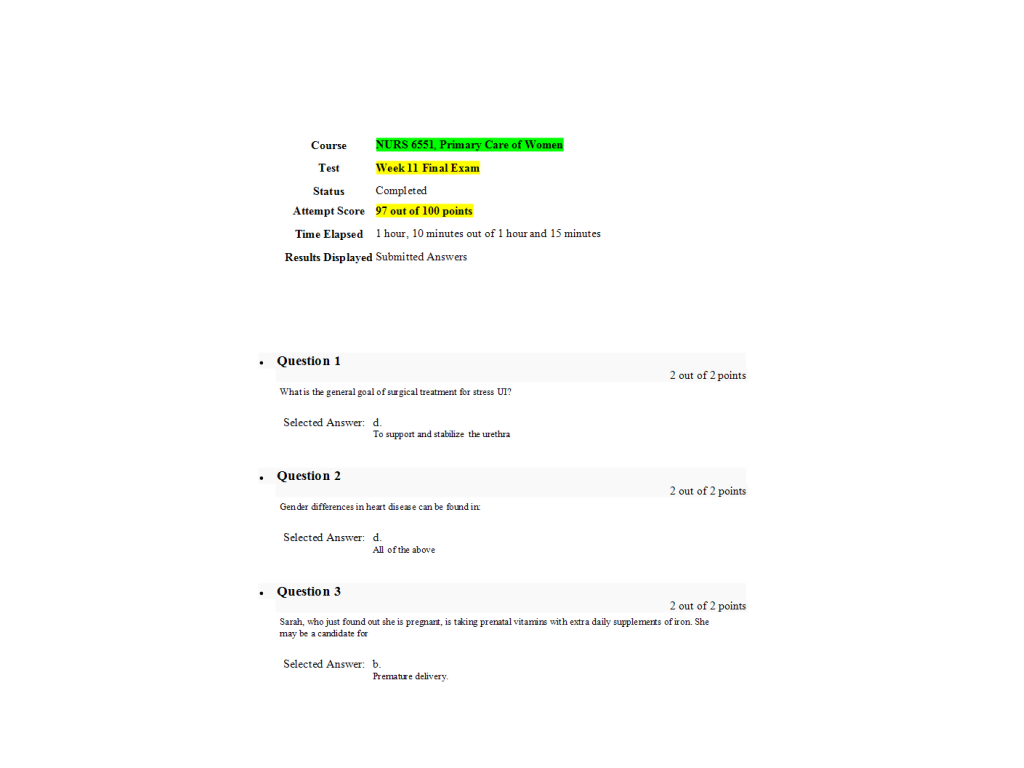
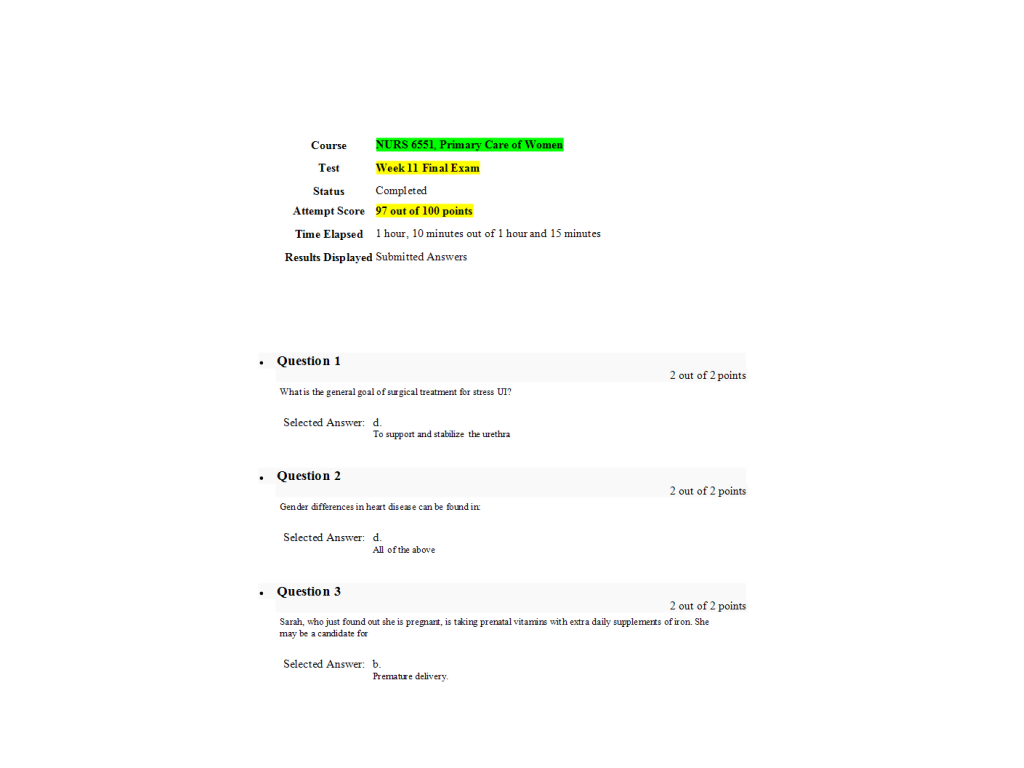
Treatment Goal
- If you have stress incontinence, pressure on your bladder affects how well the urethra and bladder neck function. The urethra is the tube that carries urine out of the bladder. The bladder neck is where the urethra joins the bladder. A group of muscles called the external urethral sphincter help control the release of urine by closing the urethra. ...
Possible Risks
- Like any surgery, urinary incontinence surgery comes with risks. Although uncommon, potential complications include: 1. Temporary difficulty urinating 2. Temporary difficulty emptying your bladder (urinary retention) 3. Development of overactive bladder 4. Urinary tract infection 5. Wound infection 6. Difficult or painful sex 7. Surgical material sticking out into the vagina 8. Groi…
Other Things to Consider
- Before deciding about surgery, consider these factors: 1. Get an accurate diagnosis.Different types of incontinence require different therapies. Your health care provider might refer you to an incontinence specialist (urogynecologist or urologist) for further diagnostic testing. 2. Understand that surgery only corrects the problem it's designed to treat.Surgery to treat stress incontinence …
Slings
- The most common procedure uses a sling to support the urethra or bladder neck. The sling is usually made from a synthetic material or a strip of your own body tissue. Your surgeon will discuss the benefits and risks of different surgical materials and different approaches for the placement of a sling. Although rare, a synthetic mesh may erode. Recovery times will vary with d…
Suspension Procedures
- Suspension procedures provide support for the urethra or bladder neck by lifting tissues around the urethra toward structures in the pelvis. The most common method is the Burch procedure. The surgeon attaches one end of surgical threads to the outer wall of the vagina and the other end to ligaments near the top of the pelvic bone. The stitches (sutures) essentially suspend the vagi…
One Step at A Time
- Finding an effective remedy for stress urinary incontinence might take time, with several steps along the way. If a conservative treatment isn't working for you, ask your doctor if there might be a surgical option for you.