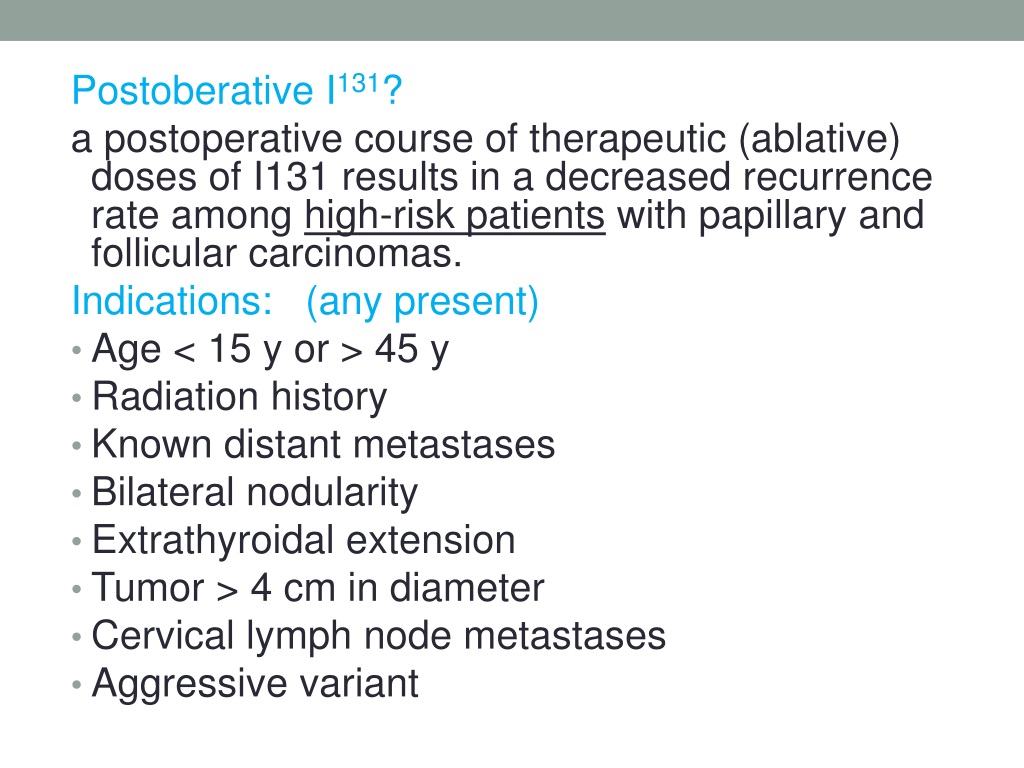
Thyroid cancer is the most frequent type of endocrine cancer and its incidence has been increasing worldwide in recent decades. 1 The standard treatment modality for these patients includes total or near-total thyroidectomy, followed by radioactive iodine-131 (I-131) therapy in selected cases and lifelong thyroid hormone suppression. 2 Eradication of normal thyroid remnants with I-131 can result in an undetectable level of serum thyroglobulin (Tg), which can facilitate biochemical follow up.
Full Answer
Can I-131 be used to treat thyroid cancer?
If your cancer cells are able to do this, then I-131 may also destroy microscopic residual thyroid cancer cells or be used as a treatment for thyroid cancer that has spread to lymph nodes or other areas of the body. Doctors cannot tell by simply looking at the thyroid cells under the microscope if they can take up iodine.
How do I prepare for I-131 therapy?
To prepare you for I-131 therapy and to maximize the effects I-131, there are two things that must happen. First, you must follow a low iodine diet for 1-2 weeks to deplete your body of iodine. Iodine is found in many foods that we eat.
What happens after taking the I-131 form?
After taking the I-131, you will be sent home or, rarely, you may be required to remain in the hospital for a few days. You will be asked to return to the nuclear medicine department 7-10 days later to have another whole body scan, also known as the "post-therapy scan," that will show where the I-131 was deposited in your body.
How can I increase my TSH level for my I-131?
You may receive injections of a medication called Thyrogen over two days prior to your I-131 therapy. Thyrogen is recombinant TSH and these injections will elevate the TSH level in your blood, which in turn stimulates the thyroid cells to take up the I-131.
What should thyroglobulin levels be after total thyroidectomy?
The normal value for thyroglobulin is 3 to 40 nanograms per milliliter in a healthy patient. If a patient's thyroglobulin level is found to be increasing after all of the thyroid gland has been removed, the patient may have a recurrence of a differentiated thyroid cancer.
What should thyroglobulin level be after Rai?
Post-Tg level increased significantly after RAI therapy compared to the pre-Tg level (mean 13.8 ± 32.2 ng/mL vs. 2.5 ± 8.9 ng/mL). In 422 patients whose pre-Tg level was < 1 ng/mL, 205 had post-Tg levels < 1 ng/mL, while 167 had post-Tg levels of 1 to 10 ng/mL, and 50 had levels > 10 ng/mL.
What is the normal range for thyroglobulin antibodies?
In a healthy individual, Thyroglobulin Antibodies need to be less than 20 IU/mL. When levels are higher than 20, this usually indicates a high level of antibodies, which means that the body's immune system is attacking the thyroid gland.
What level of thyroglobulin indicates cancer?
Tg ≥10 ng/mL: Tg levels must be interpreted in the context of TSH levels, serial Tg measurements, and radioiodine ablation status. Tg levels ≥10 ng/mL in athyrotic individuals on suppressive therapy indicate a significant risk (>25%) of clinically detectable recurrent papillary/follicular thyroid cancer.
What are high levels of thyroglobulin?
Your thyroglobulin levels are high and/or have increased over time. This may mean thyroid cancer cells are growing, and/or cancer is starting to spread. Little or no thyroglobulin was found. This may mean that your cancer treatment has worked to remove all thyroid cells from your body.
What is a normal thyroglobulin tumor marker?
However, the normal serum TG level depends on the gender and the level of iodine intake of the patient. The gender specific reference range has been given as 1.40-29.2 ng/mL for males and 1.50-38.5 ng/mL for females[6].
Is 1.0 high for a thyroglobulin antibody?
Thyroglobulin, Tumor Marker (Includes Anti-TG) Reference values apply to all ages. Interpretive Data: Current guidelines recommend measurement of Tg with a sensitive immunoassay - limit of quantification <1.0 ng/mL; for measurements of unstimulated Tg, the detection limit should be in the 0.1 to 0.2 ng/mL range.
What is high thyroglobulin antibody?
A positive test result means that you have thyroglobulin antibodies in your blood. This may mean you have a problem with your thyroid gland. A positive thyroglobulin antibody test result may also mean that your thyroglobulin test measurement is incorrect.
Can thyroglobulin fluctuate after thyroidectomy?
During the follow up of patients who underwent total thyroidectomy, the rise in thyroglobulin levels or in thyroglobulin antibodies without rise in thyroglobulin levels are usually indicative of recurrence of thyroid cancer.
Can thyroglobulin be high without cancer?
Thyroglobulin is produced in all healthy individuals, and normally its level in blood is low. Thyroglobulin levels increase in both benign (Graves disease, subacute thyroiditis, Hashimoto thyroiditis) and thyroid cancer.
What should my thyroglobulin be after cancer?
The authors showed that a thyroglobulin level > 50 ng/dl after initial surgery and without thyroid hormone replacement is able to accurately predict future reappearance of thyroid cancer in 97% of high risk patients, while an undetectable thryoglobulin level was a good predictor of an excellent outcome from thyroid ...
Remnant Ablation
Rai Effect on Cancer Cells
Preparing For Treatment
Treatment Procedure
Safety After Treatment
- I-131 remains in your system for up to a few weeks and excess not taken up by the thyroid is excreted in urine, stool, saliva and perspiration over the first 1-2 days following treatment. As the radioactivity of the I-131 in your system is a concern for those around you, you need to follow radiation safety precautions after receiving I-131. The len...
Resources For More Information