Stylecraze.com
· Certain lifestyle changes, such as diet and exercise, are considered first-line treatment for adolescent girls and women with polycystic ovarian syndrome (PCOS). [ 45] Pharmacologic treatments are...
Healthline.com
· Because polycystic ovary syndrome (PCOS) has a broad range of symptoms, health care providers may use a variety of treatments for this condition and its symptoms. Because PCOS has a broad range of symptoms, health care providers may use a variety of treatments for this condition and its symptoms.1 The treatment(s) your health care provider …
Allremedies.com
Your doctor will create a treatment plan for you tailored to treat your individual symptoms. Menstrual problems Birth control is the most common PCOS treatment for …
What is the first-line treatment for polycystic ovarian syndrome (PCOS)?
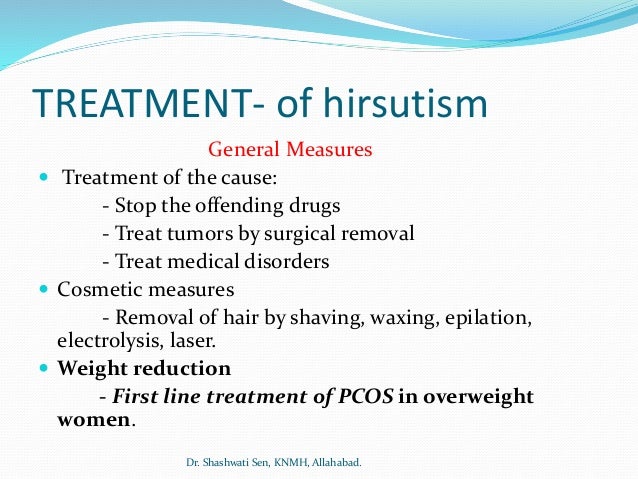
· Treatment. ANOVULATION AND INFERTILITY. Lifestyle modification and weight reduction reduce insulin resistance and can significantly improve ovulation. Therefore, ... MENSTRUAL IRREGULARITY. HIRSUTISM. ACNE. Acne is common in the general population and in patients with PCOS. Hormonal contraceptives ...
What drugs are used to treat PCOS?
16 rows · · First-line agents for the treatment of hirsutism in patients with PCOS include ...
How do I get rid of PCOS?
· Diabetes drugs are commonly used to treat insulin resistance in women with PCOS, the options of which include: 6 Glucophage (metformin), the first-line oral drug of choice that can control diabetes while promoting weight loss Actos (pioglitazone), an oral drug used to reduce high blood sugar
What blood tests are done for PCOS?
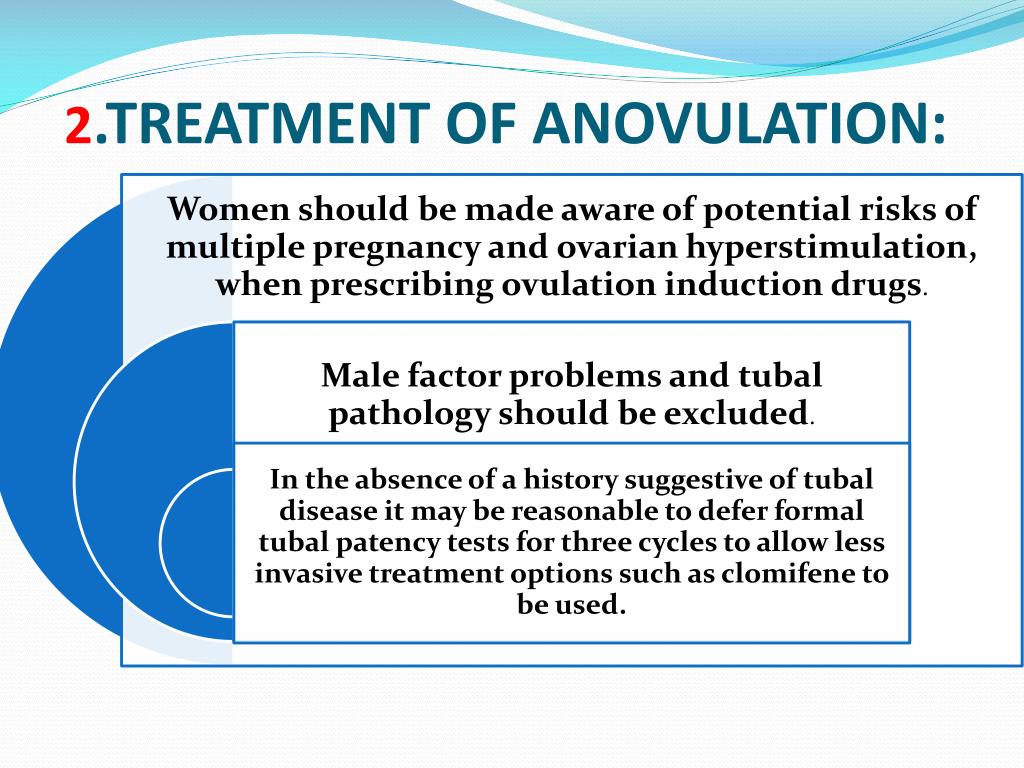
· Gonadotrophins could be considered as first line pharmacological therapy in anovulatory women with PCOS and no other infertility factors, as it is superior to both placebo or no treatment and clomiphene citrate in therapy naïve women, in the presence of ultrasound monitoring, following counselling on cost and the potential risk of multiple pregnancy.
What are the first line treatment options for PCOS?
Summary. Letrozole should be considered the first line pharmacological treatment of choice for ovulation induction in anovulatory women with PCOS and no other infertility factors, as it is superior to placebo or no treatment, metformin, clomiphene citrate and clomiphene citrate combined with metformin.
What is the primary treatment goal for PCOS?
However, the overall aims of treatment are to induce ovulation for women desiring conception, to reduce androgen levels, to reduce body weight and to reduce long-term health risks of diabetes mellitus and cardiovascular disease.
What is the standard treatment for PCOS?
Some of the most common treatments used for chronic management of PCOS include hormonal contraceptives, progestins and metformin. Treatment of infertility focuses on ovulation induction therapies which may involve drugs such as letrozole or clomiphene or gonadotropin therapy.
How long is the treatment of PCOS?
As a result, these anti-diabetes medications may improve ovulation and help make menstrual periods more regular, but this process can take four to six months.
Is metformin good for PCOS?
Metformin works as a treatment for PCOS by enhancing the body's sensitivity to insulin. This decreases the levels of circulating insulin and also produces a positive effect on adipose (fat) tissue. Doctors traditionally recommend metformin as a PCOS treatment for women who have a raised BMI (body mass index).
How do I start metformin for PCOS?
We start metformin at 500 mg once daily, increase to 500 mg twice a day after one week, then to 500 mg 3 times daily after another week. If the 3 times daily dose cannot be tolerated due to side effects, we remain on the twice-daily dose. The most effective dose of Glucophage for PCOS is generally 500mg 3 times daily.
How long metformin take to work for PCOS?
Metformin improves menstrual cycle regularity and lowers body mass index (BMI), testosterone, and luteinizing hormone (LH) within 6 months of treatment in women with polycystic ovary syndrome (PCOS) who are normal weight or overweight, new results show.
What is difference between PCOS and Pcod?
Difference between PCOD and PCOS PCOD is a condition in which ovaries produce many immature or partially mature eggs, this happen due to poor lifestyle, obesity, stress and hormonal imbalance. PCOS is a metabolic disorder and more severe form of PCOD can lead to anovulation where ovaries stop releasing eggs.
What supplements are best for PCOS?
Here are the current top 5 supplements that support insulin, metabolism and hormones in women with PCOS.Inositol. Inositol is a vitamin-like substance that helps with cellular insulin signalling. ... NAC (N-Acetyl-Cysteine) ... Vitamin D. ... Omega 3 Fatty Acids. ... Berberine.
How can I reduce my PCOS fast?
How to Lose Weight With PCOS: 13 Helpful TipsReduce Your Carb Intake. Lowering your carb consumption may help manage PCOS due to carbs' impact on insulin levels. ... Get Plenty of Fiber. ... Eat Enough Protein. ... Eat Healthy Fats. ... Eat Fermented Foods. ... Practice Mindful Eating. ... Limit Processed Foods and Added Sugars. ... Reduce Inflammation.More items...•
How is PCOS confirmed?
There's no single test for it, but a physical exam, ultrasound, and blood tests can help diagnose PCOS. You need to meet 2 of these 3 "official" criteria to be diagnosed: Irregular, heavy, or missed periods due to missed ovulation—the release of an egg from your ovaries. This also keeps you from becoming pregnant.
Can PCOS be treated without medication?
Researchers say the causes of PCOS are complicated, but insulin resistance and hormone regulation are key factors. You may be able to manage these factors and ease your symptoms through lifestyle changes and dietary supplements, but there's no one-size-fits-all approach to treatment.
What is PCOS in medical terms?
En Español. Because polycystic ovary syndrome (PCOS) has a broad range of symptoms, health care providers may use a variety of treatments for this condition and its symptoms. Because PCOS has a broad range of symptoms, health care providers may use a variety of treatments for this condition and its symptoms. 1.
Can PCOs cause pregnancy?
Because some of the common treatments for PCOS symptoms can prevent pregnancy or may harm the fetus during pregnancy, it's important to discuss your fertility goals with your health care provider while discussing treatment options.
What is the best treatment for PCOs?
Birth control is the most common PCOS treatment for women who don't want to get pregnant. Hormonal birth control -- pills, a skin patch, vaginal ring, shots, or a hormonal IUD (intrauterine device) -- can help restore regular periods.
What is PCOS treatment?
Treatments can help you manage the symptoms of polycystic ovary syndrome (PCOS) and lower your odds for long-term health problems such as diabetes and heart disease. You and your doctor should talk about what your goals are so you can come up with a treatment plan. For example, if you want to get pregnant and are having trouble, ...
Does birth control lower the chance of endometrial cancer?
These birth control methodsmay also lower your chance of having endometrial cancer, in the inner lining of the uterus.
Can PCOs cause hair growth?
Excessive hair growth. Sometimes PCOS causes unwanted hair growth, which your doctor can treat with medications and hair removal methods, such as: Depilatories: These are creams, gels, and lotions that break down the protein structure of hair so it falls out of the skin. Follow the directions on the package.
Does birth control help with acne?
Taking just a hormone called progestin could help get your periods back on track. It doesn't prevent pregnancies or treat unwanted hair growth and acne. But it can lower the chance of uterine cancer.
Does PCOs cause high blood sugar?
It may also help manage problems with blood sugar levels and ovulation. Since PCOS could lead to high blood sugar, your doctor may want you to limit starchy or sugary foods. Instead, eat foods and meals that have plenty of fiber, which raise your blood sugar level slowly.
How to deal with PCOs?
One of the best ways to deal with PCOS is to eat well and exercise regularly. Many women with PCOS are overweight or obese. Losing just 5% to 10% of your body weight may ease some symptoms and help make your periods more regular. It may also help manage problems with blood sugar levels and ovulation.
What is the first line of treatment for polycystic ovary syndrome?
For patients who are overweight, weight loss is recommended. Clomiphene and letrozole are first-line medications for infertility. Metformin is the first-line medication for metabolic manifestations, such as hyperglycemia.
What should a woman with PCOs be screened for?
All women diagnosed with PCOS should be screened for metabolic abnormalities (e.g., type 2 diabetes mellitus, dyslipidemia, hypertension), regardless of body mass index. All women with suspected PCOS should be screened for thyroid disease, hyperprolactinemia, and nonclassical congenital adrenal hyperplasia.
What should be screened for in women with PCOs?
All women diagnosed with PCOS should be screened for metabolic abnormalities (e.g., type 2 diabetes mellitus, dyslipidemia, hypertension), regardless of body mass index.
What is PCOS in medical terms?
PCOS is a multifaceted syndrome that affects multiple organ systems with significant metabolic and reproductive manifestations. Treatment should be individualized based on the patient's presentation and desire for pregnancy ( Figure 2 19, 29 – 35). Devices and medications used to treat manifestations of PCOS, and their associated adverse effects, are described in Table 2. 19, 29 – 33, 36
What is the differential diagnosis of PCOS?
The differential diagnosis of PCOS is broad and includes both endocrinologic and malignant etiologies. Figure 1 19 provides an algorithm for the workup of select presentations. For any woman with suspected PCOS, the Endocrine Society recommends excluding pregnancy, thyroid dysfunction, hyperprolactinemia, and nonclassical congenital adrenal hyperplasia. 19 Depending on presentation, conditions such as hypothalamic amenorrhea and primary ovarian insufficiency should also be excluded. In women with rapid symptom onset or significant virilization, such as deepening voice or clitoromegaly, an androgen-secreting tumor should be ruled out. Finally, Cushing syndrome or acromegaly should be excluded in patients with physical findings that suggest either condition. 19 There is no need to order laboratory testing for these conditions if the patient does not have suggestive physical findings.
How many follicles are in a polycystic ovary?
A polycystic ovary is defined as an ovary containing 12 or more follicles (or 25 or more follicles using new ultrasound technology) measuring 2 to 9 mm in diameter or an ovary that has a volume of greater than 10 mL on ultrasonography. A single ovary meeting either or both of these definitions is sufficient for diagnosis of polycystic ovaries. 23, 25 However, ultrasonography of the ovaries is unnecessary unless imaging is needed to rule out a tumor or the patient has met only one of the other Rotterdam criteria for PCOS. 19, 26 Polycystic ovaries meeting the above parameters can be found in as many as 62% of patients with normal ovulation, with prevalence declining as patients increase in age. 27
What are the three criteria for PCOs?
23 According to the Rotterdam criteria, diagnosis requires the presence of at least two of the following three findings: hyperandrogenism, ovulatory dysfunction, and polycystic ovaries.
What is the best contraceptive for PCOs?
Combination oral contraceptives, especially those with progestins of norgestimate, desogestrel, or drospirenone (because of their low androgenic effects), are among the most commonly used medications for hirsutism in women with PCOS. 2 However, they are not approved by the U.S. Food and Drug Administration (FDA) for this use. One study found that women taking desogestrel/ethinyl estradiol (Apri) had lower hirsutism scores on a standardized scale (i.e., the Ferriman-Gallwey hirsutism score). 34 Finasteride (Propecia) and flutamide (formerly Eulexin) are effective, but are FDA pregnancy categories X and D, respectively; the use of these agents for hirsutism is strictly off-label. 2
How to treat hirsutism in women with PCOs?
There are many nonpharmacologic treatment options, including electrolysis, waxing, bleaching, plucking, depilatory creams (a form of hair removal that dissolves the hair), thermolysis (use of heat), and laser therapy. Several medications have been studied for the treatment of hirsutism in women with PCOS. First-line agents include spironolactone (Aldactone) 22, 23, 28 – 30 and metformin, 13, 16, 20, 22, 31 – 33 as well as eflornithine (Vaniqa) for facial hirsutism. 9
What are the challenges of PCOS?
One of the biggest challenges in reviewing the evidence for PCOS treatment is that many manifestations of the condition may be components of other disease processes. For example, there may be a study of medications that are useful for hirsutism, but the patient population in the study did not explicitly have PCOS.
Does metformin help with PCOs?
Metformin can improve menstrual irregularities (e.g., oligomenorrhea) in patients with PCOS.
Is eflornithine safe for PCOs?
Food and Drug Administration for facial hirsutism; however, it has not been studied Specifically in women with PCOS.
Why is PCOS difficult to diagnose?
Diagnosis of PCOS may be difficult because the signs and symptoms can be subtle and varied. The most common manifestations include hirsutism, infertility, insulin resistance, and menstrual irregularities. 2 Physicians can diagnose PCOS when other causes of the symptoms or laboratory abnormalities are excluded; when oligo-ovulation or anovulation, usually manifested as oligomenorrhea or amenorrhea, is present; and when there is clinically confirmed hyperandrogenism (e.g., hirsutism, acne). Although the ovaries may be polycystic, this is usually not necessary for diagnosis. There is debate over which criteria should be used (e.g., 1990 National Institutes of Health criteria, 3 2003 Rotterdam consensus workshop criteria 4 ). Guidelines suggest screening women with PCOS for other disorders, such as hyperlipidemia, and treating accordingly. 5
Does metformin help polycystic ovary syndrome?
Metformin has the most data supporting its effectiveness.
What is the best medication for PCOs?
Diabetes drugs are commonly used to treat insulin resistance in women with PCOS, the options of which include: 6. Glucophage (metformin), the first-line oral drug of choice that can control diabetes while promoting weight loss. Actos (pioglitazone), an oral drug used to reduce high blood sugar. Avandia (rosiglitazone), an oral drug ...
What is the best pill for PCOs?
Inositol, a natural supplement used to improved egg quality in women with PCOS can also promote weight loss. Qsymia (phentermine/topiramate), an appetite suppressant that works similarly to Contrave. Saxenda (liraglutide), used to treat insulin resistance and obesity. Wegovy (semaglutide), a once-weekly injection that helps suppress appetite ...
How many women with PCOs develop diabetes?
Around 50% to 70% of women with PCOS will develop diabetes or prediabetes by the age of 40 due to the onset of insulin resistance (a condition influenced by imbalances in estrogen production). These women are also at greater risk of gestational diabetes, a condition caused by the impairment of glucose metabolism during pregnancy. 5. ...
What hormones are used when clomid or femara don't induce ovulation?
Gonadotropins, injectable hormones comprised of follicle-stimulating hormone (FSH) and/or luteinizing hormone (LH), are commonly used when Clomid or Femara don't induce ovulation.
What is the best fertility medicine for PCOs?
Clomid (clomiphene citrate), the most commonly used fertility drug that works better in some women with PCOS than others. Femara (letrozole) ., a medication mainly used to treat breast cancer that has also been shown to stimulate ovulation as well. Glucophage (metformin), a commonly prescribed diabetes drug that may enhance the effectiveness ...
Can PCOs cause anovulation?
Infertility. PCOS-related hormonal dysfunction can also cause irregular or absent ovulation ( anovulation ), making it difficult for many women with PCOS to conceive. There are medications that can improve ovulation in those experiencing infertility, used either alone or in combination.
Can medication help with menstrual cycle?
Some drug therapies can regulate hormones to restore a normal menstrual cycle .
What is the treatment for refractory ovulation?
For refractory ovulation disorders, patients can choose from among the latest treatments, including ovarian hippocampal signal path block theory, the theory of leptin, inositol treatment, bilateral ovarian drilling to stimulate ovulation and assisted reproductive technology.
What is LSM treatment?
Lifestyle modification (LSM) is considered the first-line treatment, regardless of fertility status, without the addition of metformin. Oral contraceptive (OC) pills should be used as a first-line treatment for long-term management for patients with no reproductive requirements.
What is PCOS treatment?
Polycystic ovary syndrome (PCOS) is a common endocrine disorder in reproductive-aged women, characterized by hyperandrogenism, oligo/anovulation, and polycystic ovarian morphology. Combined oral contraceptives (COCs), along with lifestyle modifications, represent the first-line medical treatment for the long-term management of PCOS. Containing low doses of estrogen and different types of progestin, COCs restore menstrual cyclicity, improve hyperandrogenism, and provide additional benefits such as reducing the risk of endometrial cancer. However, potential cardiometabolic risk associated with these agents has been a concern. COCs increase the risk of venous thromboembolism (VTE), related both to the dose of estrogen and the type of progestin involved. Arterial thrombotic events related to COC use occur much less frequently, and usually not a concern for young patients. All patients diagnosed with PCOS should be carefully evaluated for cardiometabolic risk factors at baseline, before initiating a COC. Age, smoking, obesity, glucose intolerance or diabetes, hypertension, dyslipidemia, thrombophilia, and family history of VTE should be recorded. Patients should be re-assessed at consecutive visits, more closely if any baseline cardiometabolic risk factor is present. Individual risk assessment is the key in order to avoid unfavorable outcomes related to COC use in women with PCOS.
What is PCOS in biology?
Polycystic ovary syndrome (PCOS) is a very common reproductive, endocrine, and metabolic disorder characterized by hyperandrogenism, oligo/anovulation and polycystic ovarian morphology. The prevalence of the syndrome varies from 6% to 10%, depending on which diagnostic criteria is used [1].
How much is the risk of ovarian cancer reduced with COC?
In COC users, the risk of both endometrial and ovarian cancer is reduced by nearly 30% compared to non-users [36–38]. The degree of risk reduction appears to be higher with a longer duration of COC use [36,37]. While one study reported a 20% reduced colorectal cancer risk with COC use [38], no such relationship was observed in another study [36].
What are the benefits of COC?
In particular, newer and lower-dose COC preparations reduce heavy menstrual bleeding. The E2V and dienogest combination has been effective in reducing heavy menstrual bleeding by 50% in about 80% of women [16,28]. When used continuously after surgery for endometriosis, COCs may reduce dysmenorrhea and recurrent endometriosis [29,30]. COC use has also decreased the risk of ectopic pregnancies [31], which has been attributed to the decreased risk of pelvic inflammatory disease among COC-users [32]. In cases of contraceptive failure, however, some data have indicated an increased risk of ectopic pregnancy [33]. In addition, COCs represent the second option following selective serotonin reuptake inhibitors in the treatment of physical and emotional symptoms of premenstrual dysphoric disorder [34], and combinations including drospirenone and EE might be favored [35].
How long is a COC cycle?
Most COC regimens have a 28-day cycle: 21 days of steroid and 7 days of pill-free interval or placebo. However, the duration of a placebo has been reduced to 2 or 4 days for some COCs that contain very low doses of steroids because of concerns about contraceptive failure and/or breakthrough bleeding [7,16,17].
What is the effect of COCs on ovulation?
The progestin component of COCs directly inhibits the secretion of gonadotropin-releasing hormone (GnRH) and suppresses the luteinizing hormone (LH) peak , which is essential for ovulation [14]. The absence of the LH peak causes a decrease in ovarian sensitivity to follicle-stimulating hormone (FSH), which leads to a reduction in estradiol production. Progestins also prevent sperm penetration and implantation by increasing the viscosity of cervical mucus, decreasing tubal motility, and thinning the endometrial lining [15]. The estradiol component of the drug potentiates the effect of progestin by suppressing the FSH surge in order to inhibit the selection and development of the dominant follicle, and also improves menstrual cycle control since it prevents breakthrough bleeding by maintaining endometrial proliferation [15].
Which progestins are anti-androgenic?
First- and second-generation progestins having androgenic and metabolic side effects are usually not favored in women with polycystic ovary syndrome. Third- and fourth-generation progestins cause fewer metabolic adverse effects, and fourth-generation progestins are also anti-androgenic.