Medication
Sep 02, 2021 · Top Best Treatment of Ventricular Tachycardia Related Articles Ablation Therapy for Arrhythmias This procedure is used to treat abnormal heart rhythms. Depending on the type of arrhythmia and the presence of other heart disease, a nonsurgical ablation or a surgical ablation, may be performed.
Procedures
What Is the Best Treatment of Ventricular Tachycardia? Center Ventricular tachycardia treatment aims to restore your heart rate to normal, control a fast heart rate when it occurs, and prevent future episodes.
Self-care
Ventricular tachycardia (VT or V-tach) is a type of abnormal heart rhythm, or arrhythmia. It occurs when the lower chamber of the heart beats too fast to pump well and the body doesn't receive enough oxygenated blood. A normal heartbeat begins with an electrical impulse from the sinus node, a small area in the heart's right atrium (right upper ...
Nutrition
Ablation of ventricular tachycardia has a long history of safety and success. For some patients, ablation completely cures the abnormal rhythm, and no other treatment is needed. Ablation can also improve treatment with an implantable cardioverter …
How dangerous is ventricular tachycardia?
Dec 05, 2017 · Options, depending on the severity of symptoms and degree of structural heart disease, include the following [ 9, 14] : Antiarrhythmic medications: Effective in reducing the arrhythmia burden but have no demonstrated mortality benefit [ 9]... Implantable cardioverter-defibrillator (ICD): Aids in the ...
What is ventricular Tacha Cardia and how is it treated?
Medicine treatment may include beta-blockers, calcium channel blockers, or other antiarrhythmic medicines. In people who have frequent episodes, treatment with medicines can decrease how often these occur. But these medicines may have side effects. Many people with SVT have a procedure called catheter ablation.
How do you treat ventricular tachycardia?
Mar 03, 2022 · What Is The Best Treatment For Ventricular Tachycardia? medications called anti-arrhythmics given under the direction of doctors, such as medications such as heart patches can slow the fast speed and severity of your ventricular tachycardia symptoms.
Does ventricular tachycardia go away?

What is the drug of choice for ventricular tachycardia?
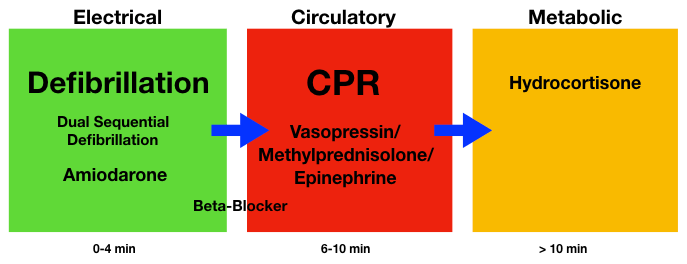
Amiodarone is the drug of choice for the treatment of hemodynamically unstable VT that is refractory to other antiarrhythmic agents. Prehospital studies currently suggest that amiodarone is safe and efficacious for use in out-of-hospital cardiac arrest.Dec 5, 2017
What is the first line treatment for ventricular tachycardia?
Anti-arrhythmic medications are the first-line therapy in emergency departments and CCUs, as discussed earlier. Amiodarone is most commonly used, along with lidocaine, and in some cases procainamide.Aug 3, 2018
Can ventricular tachycardia be cured?
Ablation of ventricular tachycardia has a long history of safety and success. For some patients, ablation completely cures the abnormal rhythm, and no other treatment is needed. Ablation can also improve treatment with an implantable cardioverter defibrillator.May 10, 2019
What is the best way to treat ventricular tachycardia?
Treatment for ventricular tachycardia may include medication, a shock to the heart (cardioversion), catheter procedures or surgery to slow the fast heart rate and reset the heart rhythm.Feb 2, 2022
Does a pacemaker help ventricular tachycardia?
Overdrive pacing may prevent certain cases of ventricular arrhythmias, and antitachycardia devices may be useful in terminating paroxysmal ventricular tachycardia. In certain circumstances, internal cardioversion or defibrillation may be an alternative.
Can a pacemaker treat ventricular tachycardia?
The U.S. Food and Drug Administration (FDA) recently approved the first of a new type of pacemaker that paces both ventricles of the heart to coordinate their contractions and improve their pumping ability.
Can ventricular tachycardia be reversed?
Ventricular Tachycardia (VT) in patients without structural heart disease. Ventricular tachycardia can also occur in patients with structurally normal hearts, unrelated to any history of coronary artery disease. It can occur in both the young and the old, and can be a benign, potentially treatable and curable condition ...
Do beta blockers prevent ventricular tachycardia?
Beta-blockers are the first-line treatment for long-term symptomatic rate control in patients with a range of cardiac arrhythmias, including atrial fibrillation and ventricular tachycardia.Jul 21, 2017
What triggers ventricular tachycardia?
Ventricular tachycardia most often occurs when the heart muscle has been damaged and scar tissue creates abnormal electrical pathways in the ventricles. Causes include: Heart attack. Cardiomyopathy or heart failure.
Is amiodarone used for ventricular tachycardia?
Amiodarone is used to manage virtually all forms of supraventricular and ventricular tachycardia and has therefore become one of the most frequently used antiarrhythmic drugs in clinical practice.Jun 19, 2010
What is amiodarone used to treat?
Amiodarone is used to treat life-threatening heart rhythm problems called ventricular arrhythmias. This medicine is used in patients who have already been treated with other medicines that did not work well.Feb 1, 2022
Does Kardia detect ventricular tachycardia?
Yes, with Kardia's Advanced Determinations, both Premature Ventricular Contractions (PVCs) and Premature Atrial Contractions (PACs) can now be detected in ECG recordings taken in the Kardia app.Jul 2, 2021
What causes ventricular tachycardia?
Your heart rate is regulated by electrical signals sent to your heart muscle. Certain conditions can interfere with normal electrical signals and cause ventricular tachycardia:
What are the signs and symptoms of ventricular tachycardia?
Ventricular tachycardia goes away on its own in 30 seconds. However, sustained ventricular tachycardia can last more than 30 seconds and requires emergency treatment.
How is ventricular tachycardia diagnosed?
Your doctor will ask you about your symptoms and take a complete medical history. They may order tests that include:
What can you do to prevent ventricular tachycardia?
Following your doctor’s treatment recommendations can help you prevent or manage episodes of the disease. In some cases, the causative factor (cardiovascular disorder, tumor, drugs, electrolyte imbalance, etc.) may need to be addressed and treated. It is also advised to adopt a healthy lifestyle that includes:
Top Best Treatment of Ventricular Tachycardia Related Articles
This procedure is used to treat abnormal heart rhythms. Depending on the type of arrhythmia and the presence of other heart disease, a nonsurgical ablation or a surgical ablation, may be performed. During a catheter ablation, catheters are advanced to the heart via blood vessels in the groin, neck, and arm.
Heart Disease: Causes of a Heart Attack
Heart disease prevention includes controlling risk factors like diet, exercise, and stress. Heart disease symptoms in women may...
Am I Having a Heart Attack? Symptoms of Heart Disease
Heart attacks symptoms vary greatly for men and women, from anxiety and fatigue to nausea and sweating. Learn the warning signs...
Heart Palpitations: 14 Possible Causes and Should You Worry?
Heart palpitations are caused by stress, exercise, caffeine, nicotine, hormone changes, fever, medications, low blood sugar,...
Cardiac Arrest: What You Should Know
Cardiac arrest is a serious medical emergency that requires immediate medical care. Use this WebMD slideshow to know whether you...
Stroke Quiz: Test Your Medical IQ
Take the Stroke Quiz to learn about stroke risks, causes, treatment, and most importantly, prevention.
Sudden Cardiac Arrest - Test Your Heart Health IQ
Take the Sudden Cardiac Arrest Quiz. Learning about this potentially deadly condition may save a life.
What causes tachycardia in the heart?
Ventricular tachycardia most often occurs when the heart muscle has been damaged and scar tissue creates abnormal electrical pathways in the ventricles. Causes include: 1 Heart attack 2 Cardiomyopathy or heart failure 3 Myocarditis 4 Heart valve disease
Where does ventricular tachycardia start?
Ventricular tachycardia begins in the lower chambers (ventricles) and is quite fast. When it lasts only a few seconds, ventricular tachycardia may cause no problems.
What is a CPVT?
Catecholaminergic polymorphic ventricular tachycardia (CPVT) is a genetic condition that can cause a fast abnormal heart beat from the ventricles. CPVT may cause a loss of consciousness or sudden death due to the lack of blood pumped to the body.
What is radiofrequency ablation?
Radiofrequency ablation: a minimally invasive procedure to destroy the cells that cause ventricular tachycardia; less effective when there is structural heart disease. Implantable cardioverter defibrillator (ICD): an implanted device that delivers an electrical pulse to the heart to reset a dangerously irregular heartbeat.
Can a person with no heart disease have ventricular tachycardia?
Sometimes, people with no known heart disease can develop ventricular tachycardia, often due to an irritable focus — when cells outside the sinus node start generating an electrical impulse automatically on their own. This form of ventricular tachycardia is easier to address and is usually not life threatening.
Can tachycardia cause lightheadedness?
When it lasts only a few seconds, ventricular tachycardia may cause no problems. But when sustained, ventricular tachycardia can lower the blood pressure, resulting in syncope (fainting) or lightheadedness. Ventricular tachycardia can also lead to ventricular fibrillation (a life-threatening arrhythmia) and cardiac arrest.
What is the procedure to treat tachycardia?
Open-heart surgery may be needed in some cases to destroy an extra electrical pathway causing tachycardia. Tachycardia may also be treated with a maze procedure. During this procedure, a surgeon makes small incisions in heart tissue to create a pattern or maze of scar tissue.
How to diagnose tachycardia?
A thorough physical exam, medical history and testing is required to diagnose tachycardia. To diagnose your condition and determine the specific type of tachycardia, your doctor will evaluate your symptoms, perform a physical examination, and ask you about your health habits and medical history. Several heart tests also may be necessary ...
How does an echocardiogram work?
An echocardiogram can help your doctor diagnose heart conditions. To complete a coronary angiogram, a catheter is inserted in an artery in your groin or arm and threaded through your blood vessels to your heart. Your doctor uses the angiogram to check for blocked or narrowed blood vessels in your heart.
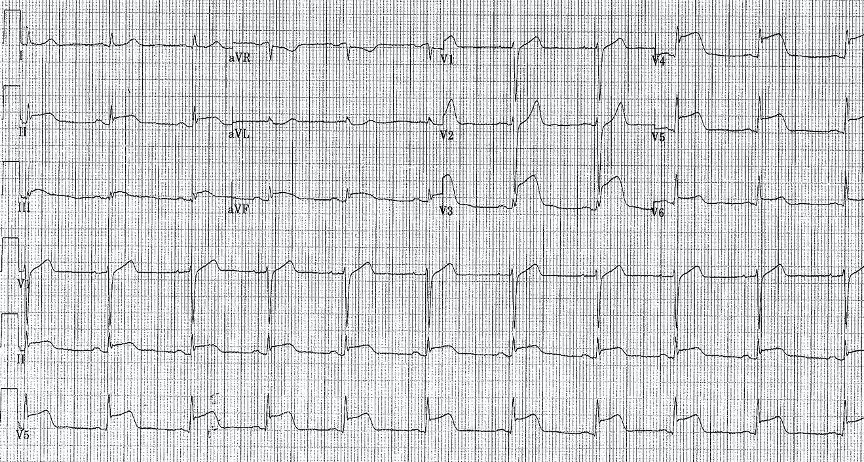
What is an EKG?
An electrocardiogram (ECG or EKG) records the electrical signal from your heart to check for different heart conditions. Electrodes are placed on your chest to record your heart's electrical signals, which cause your heart to beat. The signals are shown as waves on an attached computer monitor or printer. An electrocardiogram, also called an ECG ...
How does ablation work?
Cardiac ablation is a procedure to scar or destroy tissue in your heart that's allowing incorrect electrical signals to cause an abnormal heart rhythm. Diagnostic catheters are threaded through blood vessels to your heart where they are used to map your heart's electrical signals. Ablation catheters transmit heat or cold to scar or destroy tissue. This illustration shows ablation catheters being applied near the pulmonary veins in a type of cardiac ablation called pulmonary vein isolation, which is often used to treat atrial fibrillation.
What is an ECG device?
Portable, or remote, ECG devices include: Holter monitor. This portable ECG device is carried in your pocket or worn on a belt or shoulder strap. It records your heart's activity for an entire 24-hour period, which provides your doctor with a prolonged look at your heart rhythms.
Why is scar tissue used for tachycardia?
Because scar tissue doesn't conduct electricity, it interferes with stray electrical impulses that cause some types of tachycardia. Surgery is usually used only when other treatment options don't work or when surgery is needed to treat another heart disorder. Tachycardia consultation at Mayo Clinic.
What is the heart rate of ventricular tachycardia?
Ventricular tachycardia starts in the heart’s lower chambers. Most patients who have ventricular tachycardia have a heart rate that is 170 beats per minute or more. Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission.
What causes tachycardia in the heart?
When something goes wrong and signals are sent too quickly, it can cause tachycardia. Most patients with ventricular tachycardia have another heart problem, such as coronary artery disease, high blood pressure, an enlarged heart (cardiomyopathy) or heart valve disease.
What is an ICD device?
Implantable Cardioverter Defibrillator. An ICD is a device that is implanted under the skin. It monitors and controls the heart’s rhythm. If it detects an episode of ventricular tachycardia, it acts quickly to get your heart back to a normal rhythm.
What is the second step of a cardiac ablation procedure?
In the second step, the doctor uses a catheter with a special tip that emits a high-frequency form of electrical current. The current is used to destroy a tiny amount of tissue in the area of the ventricle where the abnormal rhythm begins. This is called an ablation procedure.
How long do you have to wear a Holter monitor?
Your doctor may also want to track your heart rhythm at home. If so, you will wear a Holter monitor at home for 24 to 48 hours. Normal Heart Rhythm recorded on EKG. Ventricular Tachycardia recorded on EKG. Your doctor may refer you to a specialist to electrophysiology testing.
What is the normal heart rate for tachycardia?
The ventricles are the heart’s two lower chambers. Blood flows from the top chambers of the heart (atria) into the ventricles, then it moves to the lungs and through the aorta to be circulated throughout the body. Tachycardia is a heart rate higher than 100 beats per minute. A normal resting heart rate is 60 to 100 beats per minute.
What happens if your heart rate is too high?
When the heart rate is extremely high or the ventricular tachycardia persists for more than a few seconds, it can cause fainting, unconsciousness or cardiac arrest and death. If you experience unexplained fainting, dizziness, lightheadedness, shortness of breath or palpitations, you should be evaluated for possible ventricular tachycardia.
What are the symptoms of tachycardia?
Unstable patients have signs or symptoms of insufficient oxygen delivery to vital organs as a result of the tachycardia. Such manifestations may include the following: 1 Dyspnea 2 Hypotension 3 Altered level of consciousness
Why do you need to have a catheter ablation?
In these patients, ablation is used to treat symptoms rather than to reduce the risk of sudden death. In patients with structurally normal hearts, catheter ablation can eliminate symptomatic VT arising from the right or left ventricle. Catheter ablation may also be used in patients with cardiomyopathy.
Can tachycardia cause cardiomyopathy?
Prolonged exposure to this (or any other) tachycardia may cause a tachycardia-induced cardiomyopathy, which typically improves with medical or ablative treatment of the VT. [ 19] Pulseless VT. Pulseless VT, in contrast to other unstable VT rhythms, is treated with immediate defibrillation.
Can antiarrhythmics be used for VT?
Combinations of these therapies are often used when structural heart disease is present. Antiarrhythmic drugs have traditionally been the mainstays of treatment for clinically stable patients with VT. However, some patients experience unacceptable side effects or frequent recurrence of VT with drug therapy.
Is magnesium good for QT?
Magnesium is unlikely to be effective in patients with a normal QT interval. [ 40] In patients with electrolyte imbalances (eg, hypokalemia or hypomagnesemia from diuretic use), correction of the abnormality may be necessary for successful cardioversion.
Does polymorphic VT recur?
Polymorphic VT in stable patients typically terminates on its own. However, it tends to recur. After sinus rhythm returns, the ECG should be analyzed to determine whether the QT interval is normal or prolonged. Polymorphic VT in patients with a normal QT interval is treated in the same manner as monomorphic VT.
Can VT cause hemodynamic collapse?
Sustained ventricular tachycardia (VT) may lead to hemodynamic collapse. Consequently, these patients require urgent conversion to sinus rhythm. The strategy for conversion depends on whether the patient is hemodynamically stable or unstable.
How is supraventricular tachycardia treated?
How is supraventricular tachycardia (SVT) treated? Your treatment for SVT depends on a few things. They include what type of SVT, how often you have episodes, and how severe your symptoms are. The goals of treatment are to prevent episodes, relieve symptoms, and prevent problems.
What is the treatment for recurring SVT?
Ongoing treatment of recurring SVT. If you have recurring episodes of SVT, you may need to take medicines, either on an as-needed basis or daily. Medicine treatment may include beta-blockers, calcium channel blockers, or other antiarrhythmic medicines.
How to tell if you have SVT?
SVT is usually treated if: 1 You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. 2 Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
What is an electric shock to the heart called?
Other treatment. An electric shock to the heart is called electrical cardioversion. It may be needed if you are having severe symptoms of SVT and your heart rate doesn't go back to normal using vagal maneuvers or fast-acting medicines. Types.
What are the symptoms of SVT?
SVT is usually treated if: You have symptoms such as dizziness, chest pain, or fainting that are caused by your fast heart rate. Your episodes of fast heart rate are occurring more often or do not return to normal on their own.
How to treat sudden onset SVT?
Your doctor will teach you how to do these safely. These are things such as bearing down or putting an ice-cold wet towel on your face.
What is it called when you have an electric shock?
An electric shock to the heart is called electrical cardioversion. It may be needed if you are having severe symptoms of SVT and your heart rate doesn't go back to normal using vagal maneuvers or fast-acting medicines.
Diagnosis
Clinical Trials
Coping and Support
Preparing For Your Appointment
Specialist to consult
Diagnosis
Treatment
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Clinical Trials
- If you have a plan in place to deal with an episode of a fast heartbeat, you may feel calmer and more in control when one occurs. Talk to your doctor about: 1. How to take your pulse and what a normal pulse rate is for you 2. When and how to use a variety of maneuvers or take additional medications if they are appropriate for you 3. When to call your doctor 4. When to seek emergen…
Lifestyle and Home Remedies
- Whether you first see your family doctor or get emergency care, you'll likely be referred to a doctor trained in heart conditions (cardiologist) for one or more appointments for a complete evaluation. If possible, bring along a family member or friend who can give some moral support and help you keep track of new information. Because there may be a lot to discuss, it will be helpful to prepar…
Alternative Medicine
Coping and Support
- The goals of tachycardia treatment are to slow a rapid heartbeat when it occurs and to prevent future episodes of a fast heart rate. If another medical condition is causing tachycardia, treating the underlying problem may reduce or prevent episodes of a fast heartbeat.
Preparing For Your Appointment
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.