Medication
Dec 23, 2020 · The first treatment option is insulin (i.m.) rather than oral antidiabetics in CF-DM patients after the endocrinologic consultation, unlike the typical type-2 DM patients. 18 The intravenous (iv) administration of aminoglycoside and CF-DM are the major causes of renal failure in CF patients. 19
Procedures
10 rows · Nov 17, 2021 · One of the primary goals of cystic fibrosis treatment is to clear mucus from the lungs using ...
Therapy
a combination of 3 medicines (Kaftrio) to treat the root cause of cystic fibrosis in people age 12 and over medicines to make the mucus in the lungs thinner and easier to cough up – for example, dornase alfa, hypertonic saline and mannitol dry powder
Nutrition
Treatments for CF focus on improving breathing and digestion, preventing and treating infections, and thinning mucus. Treatments include medicines, therapy to clear mucus out of the lungs, and in some cases, lung transplant. Pharmacogenomic approaches have led to the development of medicines that target the underlying cause of the disorder.
See more
May 01, 2016 · Physiotherapy to aid clearance of airway secretions has been one of the mainstays of treatment for CF and, in our opinion, is likely to be responsible for much of the improved prognosis over the last few decades. However, multiple different techniques are used, and the optimal approach is not clear.
How many people die from cystic fibrosis?
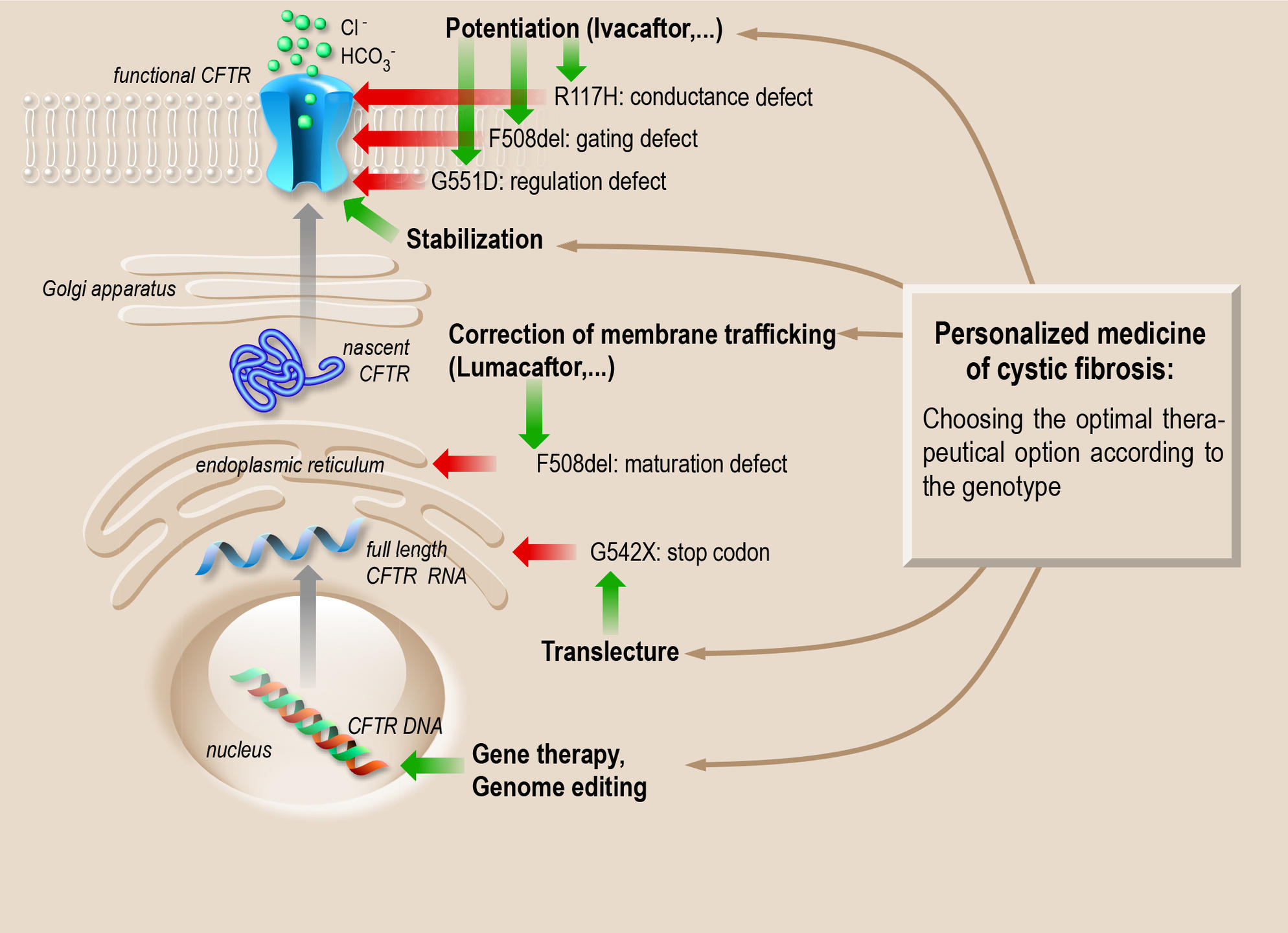
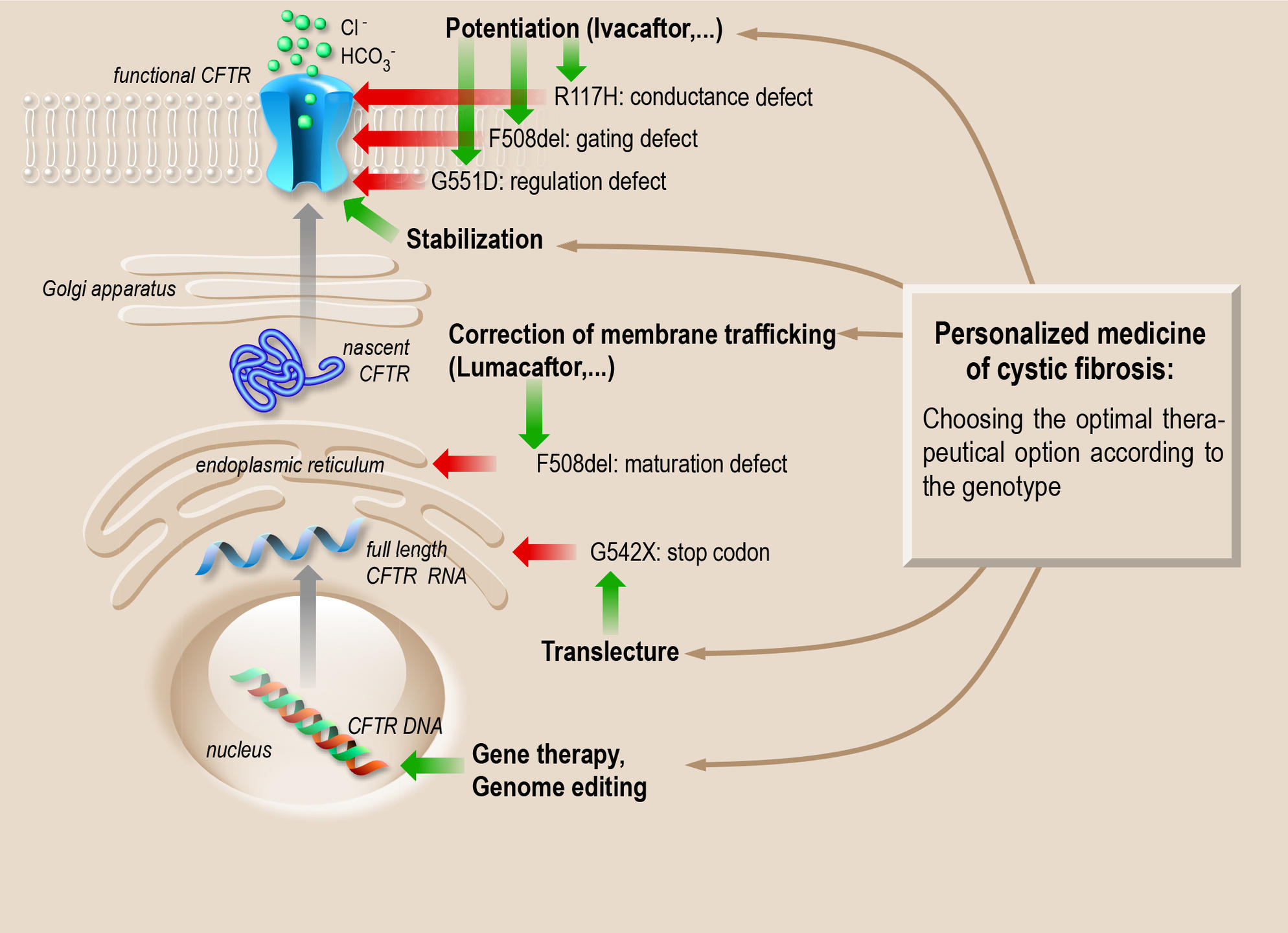
The arrival of new cystic fibrosis transmembrane conductance-regulator (CFTR)-correcting therapies will bring more opportunities to prevent the disease, apart from only treating chronic lung infection. In this review, a summary of the current knowledge of early CF lung disease is provided, based on animal model studies, as well as on data ...
Can you get cystic fibrosis at any age?
Some treatments attempt to loosen up the mucus from the lungs and thus decrease the frequency of lung infections. Treatment is broken up into medications, respiratory therapies, nutritional support, and exercise. Medications for cystic fibrosis include constant antibiotics, which can prevent and reduce the frequency of lung infections.
Who are some famous people with cystic fibrosis?
Apr 14, 2022 · Triple combination therapies, a mix of CFTR correctors and potentiators, significantly improve lung function, reduce sweat chloride, and enhance the quality of life for people with cystic fibrosis (CF), a meta-analysis of pooled results from …
What is the prognosis of cystic fibrosis (CF)?
that use vibrations to loosen mucus and help clear the airways • Chest physical therapy Certain medications, such as: • Bronchodilators, or mucus thinners, as prescribed by a doctor • Antibiotics to reduce infections • New medicines that make the CFTR protein function better • Lung transplantation,

What is the most effective treatment for cystic fibrosis?
Antibiotics to treat and prevent lung infections. Anti-inflammatory medications to lessen swelling in the airways in your lungs. Mucus-thinning drugs, such as hypertonic saline, to help you cough up the mucus, which can improve lung function.Nov 23, 2021
What is the latest treatment for cystic fibrosis?
The U.S. Food and Drug Administration today approved Trikafta (elexacaftor/ivacaftor/tezacaftor), the first triple combination therapy available to treat patients with the most common cystic fibrosis mutation.Oct 21, 2019
What are common treatments for cystic fibrosis?
antibiotics to prevent and treat chest infections. a combination of 3 medicines (Kaftrio) to treat the root cause of cystic fibrosis in people age 12 and over. medicines to make the mucus in the lungs thinner and easier to cough up – for example, dornase alfa, hypertonic saline and mannitol dry powder.
How has treatment for cystic fibrosis improved?
New genetic therapies lead to major advances in treatment of cystic fibrosis. A new therapy for cystic fibrosis (CF) that targets the genetic root of the disease has been shown to dramatically improve patients' lung function and could benefit the vast majority of patients with the disease.
Is Trikafta a pill?
You may report side effects to FDA at 1-800-FDA-1088. TRIKAFTA is a co-package of elexacaftor, tezacaftor and ivacaftor fixed-dose combination tablets and ivacaftor tablets. Both tablets are for oral administration.
How do I get Trikafta?
Check Your Eligibility. TRIKAFTA is for people age 6 years and older with at least one F508del mutation or at least one other mutation in the CF gene that is responsive to TRIKAFTA. Enter your mutations to see if at least one of them is eligible. See if the CF gene mutation you entered is correct and search again.
Can you prevent cystic fibrosis?
Since CF is a genetic disease, the only way to prevent or cure it would be with gene therapy at an early age. Ideally, gene therapy could repair or replace the defective gene.
Is there hope for a cure for CF?
While advancements in research have vastly improved the quality of life and life expectancy of people with CF, most will need to treat the condition for their entire lives. Currently, there's no cure for CF, but researchers are working toward one.
What famous person has cystic fibrosis?
List of people diagnosed with cystic fibrosisNameLifeChristopher Davies(1978—)Alexandra Deford(1971–1980)Gunnar Esiason(1991—)Bob Flanagan(1952–1996)25 more rows
How well does Trikafta work?
Data from both studies showed significant improvements in lung function in Trikafta-treated patients, with ppFEV1 improving by an average of 14.3% for this group in AURORA F/MF, and by 10% for those in AURORA F/F. Patients generally tolerated the treatment well.
What is CF in medical terms?
Cystic fibrosis (CF) is a hereditary, multisystemic disease caused by different mutations in the CFTRgene encoding CF transmembrane conductance regulator. CF is mainly characterized by pulmonary dysfunction as a result of deterioration in the mucociliary clearance and anion transport of airways. Mortality is mostly caused by bronchiectasis, ...
What is CFTR in the body?
CFTR acts as a cAMP regulated chlorine channel in apical membranes, providing Na+and water transport from epithelial cells in many organs and glands.4CFTR dysfunction primarily affects epithelial cells and causes chronic microbial infection and subsequently airway inflammation. Mortality from CF is commonly caused by bronchiectasis, ...
Where is CFTR located?
CF is caused by different mutations in the CFTR gene encoding CF transmembrane conductance regulator (CFTR), which regulates the mucociliary clearance and anion transport in airways.3The CFTR gene is located on the long arm of chromosome 7 and the CFTR protein product is 1,480 amino acids in length. CFTR acts as a cAMP regulated chlorine channel in ...
Is CFTR a heterogeneous disease?
Organoids. As CF is a genetically heterogeneous disease, currently available treatment options do not cover all CFTR mutations. Many of the known CFTR mutations are associated with a variety of disease expression and this complicates the estimation of individual disease phenotypes.
What is the first CFTR potentiator?
The first small molecule defined as a CFTR potentiator (potential enhancer) is ivacaftor, which was developed as VX-770 at first.69Ivacaftor facilitates the transport of chloride by enhancing the channel opening of the CFTR protein on the cell surface.
What is a tezacaftor?
Tezacaftor (VX-661) enhances the processing and transfer of CFTR proteins, including both normal and mutant ones (including ΔF508-CFTR), and thus increases the amount of protein reaching the cell surface. The tezacaftor/ivacaftor combination was approved by the FDA in 2018.
Is CF a hereditary disease?
Cystic fibrosis (CF) is a hereditary, multifactorial, multisystemic disease characterized by obstruction of airways, microbial infection, digestive disorders, and other complications. CF is known as the most common autosomal recessive disease in Caucasians.1. Although the incidence of disease varies greatly throughout the world, ...
Who treats cystic fibrosis?
This team will include pulmonologists, gastroenterologists, endocrinologists, nutritionists, nurses, and physical therapists.
What are the treatments for fibrosis?
Cystic fibrosis affects systems and organs throughout the body, so many other types of drugs will be relied on to treat symptoms, such as anti-inflammatory medications, prokinetics to treat gastroesophageal reflux, laxatives for intestinal obstruction, bile acids for liver blockage, and insulin for diabetes.
Why is mucus sticky in the lungs?
This is the basic mechanism responsible for cystic-fibrosis-related diseases throughout the body: Mucus in the lungs is too sticky to clear out and provides a rich environment for bacteria growth , resulting in chronic lung infections, bronchial damage (bronchiectasis), and scarring (fibrosis).
What causes mucus to be sticky?
Cystic fibrosis (or mu coviscidosis) is an inherited condition that reduces the water content of secretions within the body, causing thick and sticky mucus which fills up and blocks the lungs and other organs. It is one of the most common heritable genetic disorder in Caucasians in the US.
How many mutations are there in cystic fibrosis?
There are over 2000 genetic mutations that are responsible for cystic fibrosis. All are related to the CFTR protein. Based on the type of mutation, cystic fibrosis is divided into five classes of decreasing severity. Class 1 CF means cells are unable to produce working copies of CFTR proteins.
How to clear mucus from lungs?
One of the primary goals of cystic fibrosis treatment is to clear mucus from the lungs using physical therapy combined with mucus thinners taken through an inhaler or nebulizer. Mucolytics, such as dornase alfa, break up substances in the mucus, making it less sticky and easier to expel. Secretolytics, such as inhaled hypertonic saline solution, make mucus more watery by drawing water out of the tissues and into the airways. The effects of mucus thinners are temporary, so cystic fibrosis patients need to perform physical airway clearance to clear the thinned mucus.
Can a sweat test show CF?
A sweat test might show higher than normal salt levels, but not high enough for a CF diagnosis. A DNA test will then be used that looks for at least two copies of a cystic fibrosis mutation. There must be one copy on both chromosomes. The disease usually does not manifest if only one mutated gene is present.
What is the best treatment for cystic fibrosis?
bronchodilators to widen the airways and make breathing easier. steroid medicine to treat small growths inside the nose (nasal polyps) It's also important that people with cystic fibrosis are up-to-date with all routine vaccinations and have the flu jab each year once they're old enough.
How to clear mucus from lungs?
Exercise . Any kind of physical activity, like running, swimming or football, can help clear mucus from the lungs and improve physical strength and overall health. A physiotherapist can advise on the right exercises and activities for each individual.
How to avoid malnutrition?
A dietitian will advise on how to take in extra calories and nutrients to avoid malnutrition. They may recommend a high-calorie diet, vitamin and mineral supplements, and taking digestive enzyme capsules with food to help with digestion. The Cystic Fibrosis Trust has more information on nutrition and eating well.
What is an airway clearance device?
airway clearance devices – handheld devices that use breathing techniques, vibration and air pressure to help remove mucus from the airways (for example, a positive expiratory pressure, or PEP, device) The Cystic Fibrosis Trust has more information on airway clearance techniques and physiotherapy.
Can cystic fibrosis be treated with a lung transplant?
In severe cases of cystic fibrosis, when the lungs stop working properly and all medical treatments have failed to help, a lung transplant may be recommended. A lung transplant is a serious operation that carries risks, but it can greatly improve the length and quality of life for people with severe cystic fibrosis.
Is there a cure for cystic fibrosis?
There's no cure for cystic fibrosis, but a range of treatments can help control the symptoms, prevent or reduce complications, and make the condition easier to live with. Regular appointments to monitor the condition are needed and a care plan will be set up based on the person's needs.
What is cystic fibrosis?
Cystic fibrosis (CF) is a genetic disorder that causes problems with breathing and digestion. CF affects about 35,000 people in the United States. People with CF have mucus that is too thick and sticky, which.
How many people in the US have CF?
CF affects about 35,000 people in the United States. People with CF have mucus that is too thick and sticky, which. blocks airways and leads to lung damage; traps germs and makes infections more likely; and. prevents proteins needed for digestion from reaching the intestines, which decreases the body’s ability to absorb nutrients from food.
Is cystic fibrosis a weakened immune system?
People with cystic fibrosis (CF) are among those who might be at an increased risk for severe illness from COVID-19. In addition, some people with CF are immunocompromised (have a weakened immune system) because they have had lung or other solid organ transplants and are at increased risk for severe illness ...
Diagnosis
Clinical Trials
Coping and Support
Preparing For Your Appointment