- Cognitive-behavioral therapy. A child learns how to better solve problems, communicate, and handle stress. ...
- Family therapy. This therapy helps make changes in the family. ...
- Peer group therapy. A child develops better social and interpersonal skills.
- Medicines.
Therapy
The primary form of treatment for conduct disorder in teens is therapy, although medication may be used to treat co-occurring issues.
Self-care
Although it may not be possible to prevent conduct disorder, recognizing and acting on symptoms when they appear can minimize distress to the child and family, and prevent many of the problems associated with the condition.
What are the treatment options for conduct disorder in teens?
No medications have been formally approved for conduct disorders in general, so medications are directed at specific symptoms. Symptom control may help the child participate in family or systemic interventions or treatments. Symptom-control medications include:
Is there a way to prevent conduct disorder?
As with adults, mental illnesses in children are diagnosed based on signs and symptoms that suggest a particular problem. If symptoms of conduct disorder are present, the doctor may begin an evaluation by performing complete medical and psychiatric histories.
What medications are used to treat conduct disorders?
How is conduct disorder diagnosed in children?
Is there a cure for conduct disorder?
Medication: Although there is no medication formally approved to treat conduct disorder, various drugs may be used (off label) to treat some of its distressing symptoms (impulsivity, aggression, dysregulated mood), as well as any other mental illnesses that may be present, such as ADHD or major depression.
What is the first line treatment for conduct disorder?
Psychosocial intervention should be used as a first-line treatment for conduct disorder symptoms that persist after comorbidities such as ADHD are treated. Risperidone (Risperdal) may benefit patients with conduct disorder who have severe aggression or explosive anger after comorbid ADHD is treated (if applicable).
How do you discipline a child with conduct disorder?
Oppositional Defiant Disorder Strategies: 8 Discipline Rules forTreat before you punish.Exercise away hostility.Know your child's patterns.Be clear about rules and consequences.Stay cool-headed and under control.Use a code word like 'bubble gum. 'Stay positive.Call in the professionals.
Can a child grow out of conduct disorder?
The majority of children, about 70%, who do display symptoms of conduct disorder will grow out of it by adolescence. The children that do not grow out of it and progress on to adolescence have a poorer prognosis than those with the adolescent-onset type.
What therapy is best for conduct disorder?
Treatment for conduct disorder may include: Cognitive-behavioral therapy. A child learns how to better solve problems, communicate, and handle stress. He or she also learns how to control impulses and anger.
At what age does conduct disorder usually begin?
Conduct disorder can have its onset early, before age 10, or in adolescence. Children who display early-onset conduct disorder are at greater risk for persistent difficulties, however, and they are also more likely to have troubled peer relationships and academic problems.
Is conduct disorder a disability?
“Disability” can include behavioral and other mental health disorders, such as depression, anxiety disorder, obsessive-compulsive disorder, phobias, or conduct disorder, to the extent that it interferes with the child's ability to thrive at school.
Is conduct disorder a result of trauma?
Some experts believe that a series of traumatic experiences occurs for a child to develop a conduct disorder. These experiences then often lead to depressed mood, behavior problems, and involvement in a deviant peer group.
What are the symptoms of conduct disorder?
Symptoms of conduct disorder include:Not caring about social norms of good behavior.Ignoring the rights and feelings of other people.Enjoying causing harm, lying or manipulating people.Committing physical or sexual violence.Hurting animals.More items...
How can I help my teen with conduct disorder?
Communicate rules and consequences clearly. Be patient, understanding that it will take time for your teen to break old patterns of behavior and develop a more positive attitude. Don't take your teen's negative behavior personally. Encourage your teen to use the skills he or she is learning in therapy at home.
Does conduct disorder turn into antisocial?
Conduct disorders in childhood are also associated with a significantly increased rate of mental health problems in adult life, including antisocial personality disorder - up to 50% of children and young people with a conduct disorder go on to develop antisocial personality disorder.
What is dual diagnosis treatment?
Dual diagnosis treatment is recommended for adolescents who have both conduct disorder and a substance use disorder. This type of treatment often occurs in a residential treatment setting or as part of an intensive outpatient treatment program.
What is the most effective form of therapy for conduct disorder?
Talk Therapy – Three of the most effective and common forms of talk therapy used in the treatment of conduct disorder include cognitive behavioral therapy (CBT), multisystemic therapy, behavior therapy, and family therapy.
What are the signs of conduct disorder in teens?
Frequent acting out, cruelty to people or animals, defiance, and aggressive behavior are just some of the warning signs of conduct disorder in children and teens. While some of these behaviors can be alarming to parents, they can also have serious consequences for you teen – including getting suspended or expelled from school or landing in ...
How to overcome conduct disorder as a teenager?
Understand that conduct disorder isn’t something your teen can simply overcome with sheer willpower, nor is it merely a phase of adolescence. Actively participate in your teen’s treatment and consult with his or her treatment provider regarding concerns and questions. Strive to create and maintain a low-stress, safe, ...
How to know if your child has conduct disorder?
To get your child the help he or she needs as early as possible, which is crucial with conduct disorder, you need to know what to look for. Signs and symptoms of conduct disorder include: Aggression towards people or animals. Threatening harm towards others. Frequently starting fights with others.
What are the challenges of parenting children with conduct disorder?
One of the greatest challenges of parenting children and adolescents with conduct disorder is that they can be highly impulsive and unpredictable. As a result, things can quickly escalate and lead to a crisis. If your child is threatening to harm or actively harming you or anyone – other family members, family pets or other animals, classmates, etc. – then everyone’s safety is your highest priority. Turning a blind eye or assuming things will calm down on their own can lead to disastrous outcomes.
How to deal with a teenager with conduct disorder?
If your observations and instincts lead you to suspect your adolescent has conduct disorder, the first three steps to take towards handling the situation are to: 1 – Talk to your teen. Sit down with your teen and express your concerns about the troubling behaviors you’ve noticed.
What is layered treatment of conduct disorder?
A layered or multisystemic treatment of conduct disorder includes working with the family, peers, neighborhood, and school to approach the behaviors as being linked to various sources. For instance, peers may contribute to encouraging bad behavior or schools may have ineffective consequences for handling bad behavior.
How to stay committed to child therapy?
It’s important for parents to remain committed to treatment for their child. Commit to regular appointments, show up on time, and follow through with any assignments the therapist asks you to do between sessions.
What can a therapist do for you?
A therapist can help you work through feelings of blame toward yourself or toward your child.
How to treat conduct disorder?
Seek therapy. Conduct disorder is very hard to treat without therapeutic intervention. Seek a therapist experienced with working with children and families around issues of conduct disorder. A comprehensive therapist may gather information from the parents, child, and family, in addition to information from the school, community, and the legal system (if applicable). [3]
What is a child's behavior disorder?
Conduct disorder (CD) is identified in a child or adolescent through symptoms including aggression, deliberate property damage, repeated violations at home, school, or work, and persistent lying to avoid consequences. Conduct disorder also can include bullying, starting fights, theft, vandalism, shoplifting, skipping school, ...
Why is medication important?
Medication helps to cope with symptoms, not fully treat a disorder. Therapy is often most beneficial, and medications can accompany treatment in tandem. If obtaining medication, seek a psychiatrist whom you trust to talk to about your moods, symptoms, medication, and overall well-being.
What are the symptoms of conduct disorder?
While parental involvement in important, many parents struggle with their own mental health issues: many parents of children with conduct disorder tend to exhibit symptoms of depression, substance abuse, or antisocial personality traits.
What Are the Symptoms of Conduct Disorder?
Symptoms of conduct disorder vary depending on the age of the child and whether the disorder is mild, moderate, or severe. In general, symptoms of conduct disorder fall into four general categories:
How Is Conduct Disorder Diagnosed?
If symptoms of conduct disorder are present, the doctor may begin an evaluation by performing complete medical and psychiatric histories. A physical exam and laboratory tests (for example, neuroimaging studies, blood tests) may be appropriate if there is concern that a physical illness might be causing the symptoms. The doctor will also look for signs of other disorders that often occur along with conduct disorder, such as ADHD and depression.
What Is the Outlook for Children With Conduct Disorder?
A child or teen with conduct disorder is at risk for developing other mental disorders as an adult if left untreated. These include antisocial and other personality disorders, mood or anxiety disorders, and substance use disorders.
Can Conduct Disorder Be Prevented?
Although it may not be possible to prevent conduct disorder, recognizing and acting on symptoms when they appear can minimize distress to the child and family, and prevent many of the problems associated with the condition. In addition, providing a nurturing, supportive, and consistent home environment with a balance of love and discipline may help reduce symptoms and prevent episodes of disturbing behavior.
What factors contribute to conduct disorder?
Environmental: Factors such as a dysfunctional family life, childhood abuse, traumatic experiences, a family history of substance abuse, and inconsistent discipline by parents may contribute to the development of conduct disorder.
What is the best way to control anger in children?
Psychotherapy: Psychotherapy (a type of counseling) is aimed at helping the child learn to express and control anger in more appropriate ways. A type of therapy called cognitive-behavioral therapy aims to reshape the child's thinking (cognition) to improve problem solving skills, anger management, moral reasoning skills, and impulse control. ...
What is the purpose of a psychologist's assessment?
Psychiatrists and psychologists use specially designed interview and assessment tools to evaluate a child for a mental disorder. The doctor bases their diagnosis on reports of the child's symptoms and their observation of the child's attitudes and behavior.
What is conduct disorder?
Conduct disorder is a behavioral disorder that occurs when children engage in antisocial behaviors, have trouble following rules, and struggle to show empathy to others. They may also threaten the safety of others or themselves. Conduct disorder typically emerges in children under the age of 16, but can be diagnosed in adults as well.
What is the difference between autism and conduct disorder?
One is that people with conduct disorder have trouble with social interaction because of deficits in social learning, whereas people with autism have trouble socializing due to developmental challenges.
What are the causes of conduct disorder in children?
Children diagnosed with conduct disorder may have a history of the following: abuse. poverty. parental substance abuse. other mental health problems. family conflict or violence. brain damage. other trauma. Researchers also believe that genetics may play a role in the development of conduct disorder.
How long does it take to get diagnosed with conduct disorder?
Signs must have been present for at least a year in order to receive a diagnosis.
Why is early diagnosis important?
Early diagnosis and treatment is vital to preventing additional mental health and behavioral challenges. With the right support, children and teens can begin to engage more positively with their peers and adults and learn to correct harmful behaviors. Article Sources. American Psychiatric Association. (2013).
Why is it so hard to treat conduct disorder?
Treatment can prove difficult because children are often uncooperative and distrustful of adults.
How can positive parenting help with conduct disorder?
Researchers believe that positive parenting as well as providing a safe and supportive environment for a child can reduce the risk of conduct disorder. Reducing the risk factors that can increase the possibility of conduct disorder, such as poverty and abuse, is likely to ensure the best outcome for the child.
What happens if an adolescent is arrested?
If the adolescent is arrested and incarcerated, experiences with other deviant peers in the juvenile justice setting create advanced learning opportunities in deviant behavior. Promising Treatments. A number of different interventions have been used to treat youth with conduct disorder.
What is the effect of aggression on a child?
Continued aggression makes the conduct-disordered preadolescent and adolescent unattractive to peers. This occurs during a development period where social and physical status is critically important. Aggressive and noncompliant actions in the classroom create an environment where teachers and other school staff reject the individual. Also, parents of the student with conduct disorder may have negative interactions with school staff due to the child's continuing disruptive behavior. An unfortunate result is that parents may lose interest in their child's activities and friends.
How does conduct disorder affect adolescents?
The greatest difficulty arises from the fact that conduct disorders impacts not only the adolescent but also his or her family, school, and community. Family-based interventions have consistently demonstrated the ability to positively alter behavior.
What are the four categories of conduct disorder?
The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) defines conduct disorder as a "persistent pattern of behavior in which the basic rights of others or major age-appropriate societal norms or rules are violated." The manual breaks the behavior patterns into four areas or criteria: 1 aggression (such as physical fights, cruelty to animals, and forced sexual activity) 2 destruction of property (such as fire setting or inflicting other types of property damage) 3 deceitfulness or theft (such as breaking into someone else's home or stealing items without confronting the owner) 4 serious violation of rules (such as truancy and running away from home)
What is an adolescent onset?
Adolescent-ons et type is defined by the absence of any criterion characteristic of conduct disorder prior to age ten. These individuals tend to be less aggressive and have more normative peer relationships. Often, their aggressive tendencies come out while involved in a group action. The prognosis for an individual with adolescent-onset type is ...
Why do people with conduct disorder need an observer?
Because individuals diagnosed with conduct disorder tend to tell lies, the use of "observers" is often necessary. An observer is any individual (employer, teacher, parent, and so on) who can provide independent and accurate information about the individual's behavior. Middle School and High School Years.
What is the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders?
The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) defines conduct disorder as a "persistent pattern of behavior in which the basic rights of others or major age-appropriate societal norms or rules are violated.".
Why should comorbid disorders be identified in making the diagnosis?
Comorbid disorders such as the following should be identified in making the diagnosis because their existence can influence presentation and treatment options: Attention deficit hyperactivity disorder (ADHD), which has features of disinhibition, inattention and distractability.
How to treat conduct disorder?
Treatment options for conduct disorder are family therapy, behavioral modification and pharmacotherapy, often in combination. The clinician must assess the severity of the individual child’s disorder and should refer the child and family to a subspecialist if any of the following conditions apply: there are concerns about safety, diagnostic behaviors escalate rapidly, psychoeducational interventions are ineffective, there is conflicting information from multiple sources or many comorbid symptoms exist [4]. Substance abuse problems should be treated first with appropriate interventions and rehabilitation.
Why do parents need to be involved in administering stimulants?
Parents may need to be involved in administering or monitoring the medication because of its street value and potential for abuse by peers.
Why is lithium used in bipolar disorder?
Anticonvulsants including lithium have been used to treat aggression and mood lability symptoms associated with bipolar disorder. Because monitoring side effects and blood levels is important, a family’s ability to comply with treatment and follow-up should be considered.
What is the best medication for bipolar?
Vital signs, dizziness, sedation and potential tolerance or dose changes should be monitored. Atypical antipsychotics such as risperidone are used to treat aggression. These medications are also used to treat mood lability and bipolar symptoms. Weight gain and risk for metabolic disorder should be followed closely.
What percentage of boys have conduct disorder?
As many as 5 percent of preadolescent boys, 8 percent of adolescent boys and a quarter to a half that percentage of girls of those same ages fulfill criteria for a diagnosis of conduct disorder [1]. In contrast to isolated behavior problems, this diagnosis requires a repeated, persistent pattern of violating the rights of others and age-appropriate societal rules for six months or more. Multiple factors are probably responsible for this developmental pathway [2]. The primary features of conduct disorder are:
What are the characteristics of conduct disorder?
The primary features of conduct disorder are: Aggression. Vandalism. Theft. Frequent lying. Violation of rules, running away. About 40 percent of children with the diagnosis of conduct disorder will grow into adults with antisocial personality disorder.
Why is it important to manage symptoms?
Managing Symptoms: Staying Healthy. Being healthy is important for all children and can be especially important for children with behavior or conduct problems. In addition to behavioral therapy and medication, practicing certain healthy lifestyle behaviors may reduce challenging and disruptive behaviors your child might experience.
What is behavior disorder?
Children sometimes argue, are aggressive, or act angry or defiant around adults. A behavior disorder may be diagnosed when these disruptive behaviors are uncommon for the child’s age at the time, persist over time, or are severe. Because disruptive behavior disorders involve acting out ...
What are the behaviors of children with ODD?
Children with ODD are more likely to act oppositional or defiant around people they know well, such as family members, a regular care provider, or a teacher. Children with ODD show these behaviors more often than other children their age. Often arguing with adults or refusing to comply with adults’ rules or requests.
How to treat disruptive behavior disorder?
Treatment for disruptive behavior disorders. Starting treatment early is important. Treatment is most effective if it fits the needs of the specific child and family. The first step to treatment is to talk with a healthcare provider.
Why do children have disruptive behavior?
It is known that children are at greater risk when they are exposed to other types of violence and criminal behavior, when they experience maltreatment or harsh or inconsistent parenting, or when their parents have mental health conditions like substance use disorders#N#external icon#N#, depression#N#external icon#N#, or attention-deficit/hyperactivity disorder (ADHD). The quality of early childhood care also can impact whether a child develops behavior problems.
What is external icon?
external icon. , or attention-deficit/hyperactivity disorder (ADH D). The quality of early childhood care also can impact whether a child develops behavior problems. Although these factors appear to increase the risk for disruptive behavior disorders, there are ways to decrease the chance that children experience them.
When does oppositional defiant disorder start?
ODD usually starts before 8 years of age, but no later than by about 12 years of age. Children with ODD are more likely to act oppositional ...
How do you know if you have a CD?
Symptoms develop earlier in boys than girls. The usual age of presentation is 10–12 years in boys, whereas it is 14–16 in case of girls. Individual having CD shows behavioral manifestations in the following four categories as per DSM-5: Aggression to people and animals, destruction of property, deceitfulness or theft and serious violations of rules. Aggression to people and animals includes behaviors such as threatening, frequent physical fights, using weapon that can cause damage to others or showing physical cruelty to people or animals. Setting fire or deliberately destroying others property are included in the destruction of property. Deceitfulness or theft involves setealing or breaking into others house, building. Individual often shows disobedient to parental prohibitions or truancy from school. All this should begin before the age 13 years. DSM-5 requires the persistent presence of three behaviors over period of 12 months with atleast one of them present in the last 6 months. The disturbance in behaviour causes significant impairment in social, academic or occupational functioning. When at least 1 symptom appear before the age 10 then it is specified as childhood-onset while no symptoms before 10 years for CD are classified as adolescent-onset type CD. DSM-5 has introduced a new specifier– “with limited prosocial emotion.” Individual must show at least two of the following interpersonal and emotional pattern: (1) Lack of empathy, (2) Lack of guilt or remorse, (3) Unconcerned about performance, (4) Shallow of deficient affect. Depending on the severity of behaviors CD is classified into mild, moderate, or severe type. As per ICD-10 for diagnosis of CD child's developmental level should be taken into consideration. For example, the presence of temper tantrum would not classify for CD. Behavioral manifestation should be present for at least 6 months before making a diagnosis of CD. It has classified CD into three types based on setting in which behaviors are manifested: CD confined to the family, unsocialized CD and socialized CD. In CD confined to family, outside the family environment the conduct symptoms are negligible. Hence, there are no significant disturbances in child's social relationships outside the family context. Main differentiating feature between unsocialized and socialized CD is based on integration into a peer group. Children who meet these criteria exhibit aggressive behavior in different forms such as physical aggression, and bullying. In severe cases, it leads to the destruction of property, physical violence. There is frequent use of substance and involvement in promiscuous sexual activity. They have difficulty in having a relationship with family and peers. They have less concern for others feeling and also have low self-esteem. They frequently blame others for their behavior. Severe punishment for such behavior invariably increases their aggression rather than improvement. In the evaluation complete psychiatric assessment along with appropriate history taking should be carried out. Assessment should be carried out in different settings. Additional information may need to be collected from teachers and other family members. Family history reveals frequents fights in parents, disharmony, frequent use of the substance, high rates of psychiatric disorder and harsh parenting.
What is antisocial behavior?
Conduct disorder (CD) and associated antisocial behavior is one of the most common mental and behavioral problems in children and young people. In the United States, CDs associated behaviors are primary presenting complains in children and adolescent. CD are characterized by a repetitive and persistent pattern of dissocial, aggressive, or defiant conduct (ICD-10). Associated behaviors are outside the socially accepted norms that results into persistent and significant violations of age appropriate social expectations. CD is classified along with the diagnosis of oppositional defiant disorder (ODD) in the spectrum of disruptive behavior disorders. ODD can be seen as precursor to the development of CD. Behaviors include stealing and lying, excessive physical and verbal aggression, rule breaking and violence. Persistence of these behaviors into adulthood leads to antisocial personality disorder (ASPD). As these behaviors are present in some children during the course of development, it is essential for the clinician to differentiate between normalcy and pathological behavior. Remote antisocial or illicit acts are not enough to support a diagnosis of CD. CD must be differentiated from other term like delinquency. CD is a mental and behavioral disorder while delinquency is a legal term. It is comorbid with many other psychiatric conditions, including attention deficit hyperactive disorder (ADHD), depression, substance use disorders, etc. CD in early life has been found to be strongly associated with significant decline in educational performance. They are more likely to remain socially isolated with increase in substance misuse during adolescence. There is increase involvement in criminal acts resulting in frequent contact with the criminal justice system. This adverse effect continues even in adult life with resulting poorer educational and occupational outcomes. There are limited data available about the prevalence of CD across the world. Using the diagnostic and statistical manual of mental disorders-III (DSM-III) and DSM-III-R diagnostic guidelines, the prevalence of CD in the United States was found to be 6%–16% in males and from 2% to 9% in females. With a clinical interview as a method of detection, the prevalence of CD in the general population is found to be between 1.5% and 4%. Boys are likely to have these conditions two times more than girls. Those with early-onset exhibit lower IQ compared to children with later age of onset. They have more attention deficits and impulsivity problems. It is comorbid with many other psychiatric conditions including ADHD, depression, substance use disorders, etc., Children with CD also find difficulty in interacting and integrating with peer group and are more likely to had adverse family circumstances. Increased risk factors include poor prenatal care and poor infant nutrition, poverty, physical abuse, and more crime in the neighborhood society. Families of children and adolescent with CD are more likely to exhibit parents with low income, substance abuse, depression, somatization, and ASPD. CD in early life has been found to be strongly associated with significant decline in educational performance. They are more likely to remain socially isolated with increase in substance misuse during adolescence. There is increase involvement into criminal acts resulting into frequent contact with the criminal justice system. This adverse effect continues even in adult life with resulting poorer educational and occupational outcomes.
How to manage CDs?
Nonpharmacological management has been the mainstay of treatment in managing the CDs. The preventive programs as discussed in the later section should form the most important of the intervention strategies while talking about this issue. In preschool children such programs, for example, Head Start has been tried. They provide parent education about normal development; provide children with stimulation and crisis management to the parents. In the clinical setting, the interventions are targeted toward the temperament of the child, the interpersonal relations in the family, and increasing the parental efficiency in addressing the child's behavioral issues. In the school-aged children, the primary target of intervention is the child, family, and the school. Both parenting skills training and training for the child to improve peer relationships, social competence, academic performance, and compliance with demands from parents/teachers are effective for CD. As in adolescent period the relative importance of peers is increased than that of the family, the interventions should also be targeted toward the peer group. The multi-systemic therapy is imparted in the family environment to the adolescents with conduct problems. It combines intensive case management in the home setting with family interventions, and this has been found to be cost effective. Psychoeducational intervention to inculcate social skills, address conflict resolution and anger control skills to target adolescents and parents are found to be helpful.
How does CD develop?
This evolves to stage where consistent enduring pattern develops which involves violation of basic rights of others. Behavior develops in continuum where ODD forms least severe clinical presentation to ASPD as most severe. As these behaviors are present in some children during development, it is essential for the clinician to differentiate between normalcy and pathological behavior. Remote antisocial or illicit acts are not enough to support a diagnosis of CD. CD must be differentiated from other term like delinquency. CD is a mental and behavioral disorder while delinquency is a legal term.
What is parent management training?
The major objective of parent management training (PMT) is to teach parents the skill of developing and implementing a systematic contingency management plan in home setting. This aims to improve the interaction between parent and child at home and to change the antecedents to behavior to increase the possibility that the child will show prosocial behavior. It also helps parents to improve their capability to keep an eye on their children and teaches them more efficient discipline strategies. Deficiencies in the above-mentioned areas of parenting strategy have been constantly associated with child CD. A randomized study on PMT has shown decrease in the child conduct problem reported by mother. The effect sizes were largest among mothers who were present for >50% of the group sessions. There was no significant effect of the intervention on conduct problems and social competence in kindergarten or school as reported by teachers. Internet-based PMT also showed a greater reduction in conduct problems compared to the waitlist children. It has also been found that during 18 months period after the intervention, child conduct problems continued to decrease whereas parenting skills declined somewhat from post-treatment of internet-based PMT. A Cochrane review of thirteen trials on 1078 participants (646 in the intervention group; 432 in the control group) found that parent training produced a statistically significant reduction in child conduct problems, whether assessed by parents or independently assessed. It also found that there was a significant improvement in the mental health of the parents. There was an improvement in positive parenting skills and a reduction in negative or harsh parenting practices which are found to be statistically significant. This observation was based on both parent reports and independent assessments. The intervention was found to be cost-effective. When the costs of program delivery was compared with the long-term health, social, educational, and legal costs associated with childhood conduct problems they were found to be modest. The researcher concluded that behavioral and cognitive-behavioral group-based parenting interventions are effective. They are cost effective for short-term to improve child conduct problems, parental mental health and parenting skills. However, the long-term assessment of outcomes is still needs to be done. Meta-analytical studies of PMT and cognitive-behavioral Therapy for the child have revealed a positive effect of these interventions on a child with CD. However, majority of the studies included in this meta-analysis were carried out in research conditions and are not representative of the treatment effectiveness in everyday clinical practice. In Germany, “START NOW” group-based behavioral skills training program have been developed to target the specific needs of girls with CD in residential care. It aims at enhancing emotional regulation capacities in females with CD or ODD to appropriately deal with day to day life demands. It is intended to enhance psychosocial adjustment and well-being as well as reduce oppositional and aggressive behavior. The primary aim is to decrease the number of CD/ODD symptoms as assessed by a standardized, semi-structured psychiatric interview between baseline and the end of the intervention, in addition to that between baseline and 3 months follow-up point. Secondary objectives include pre- and post-change in CD/ODD-related outcome measures, most notably emotional regulation aspects on a behavioral and neurobiological level. However, this study is underway.
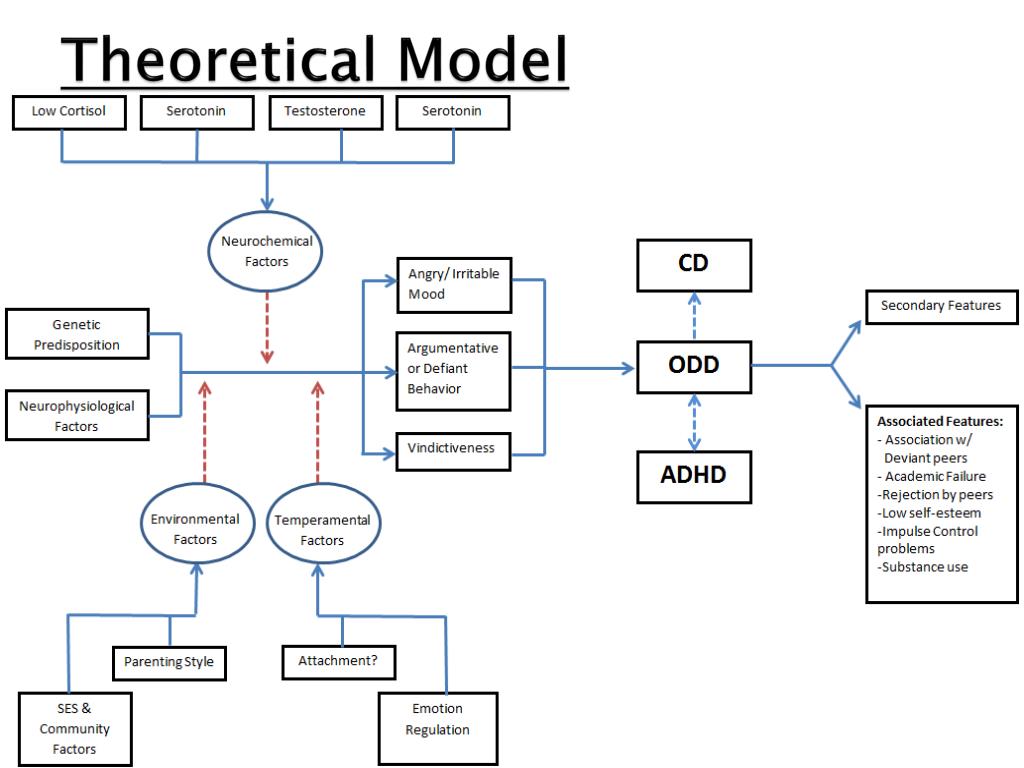
What are the etiological factors of CD?
Genetic liability along with various environmental factors acts together for the manifestation of behavioral symptoms of CD. Magnetic resonance imaging has been used to compare structural brain differences between children with CD and normal controls and have documented smaller brain structures and lower brain activity in children with CD. Abnormalities are primarily detected in the bilateral amygdala, right striatum, bilateral insula and left medial/superior frontal gyrus as well as the left precuneus in individuals having ODD/CD. Higher plasma levels of serotonin in blood are positively associated with aggressive behavior in children. Impulsiveness and aggression along with violent behavior have been found to be associated with alteration in the activity of certain brain structures. Areas mainly associated and affected are limbic structures and the anterior cingulate and orbitofrontal areas of the prefrontal cortex . Parental psychopathology along with harsh parenting is associated with CD in their children. The presence of antisocial behavior in children has been found to be associated with parental reinforcement, their responsiveness to the child and punishment given by them. Frequent marital conflicts between parents and interparental violence predict adolescent antisocial behavior. Children with CD have been found disproportionately coming from low-income family and with unemployed parents. Inadequate housing, poverty, and crowding exerts negative influence on the development of the child. Exposure to and prevalence of substance use in the community have also been found significantly associated with the development of CD. Availability of drugs and increased crime in the neighborhood increases the risk of children developing CD. Peer relation also significantly affects the development and maintenance of these behaviors.
What is the Achenbach's child behavior checklist?
The Achenbach's child behavior checklist had an Indian adapted version and known as childhood psychopathology measurement schedule (CPMS). It is a semi-structured interview schedule having 75 symptoms and has a designated section on CD symptoms, and it gives a dimensional score. It is standardized on Indian children with good reliability (0.88–0.98) and validity. With a cut-off score of >10, CPMS has 82% sensitivity and 87% specificity.
