Medication
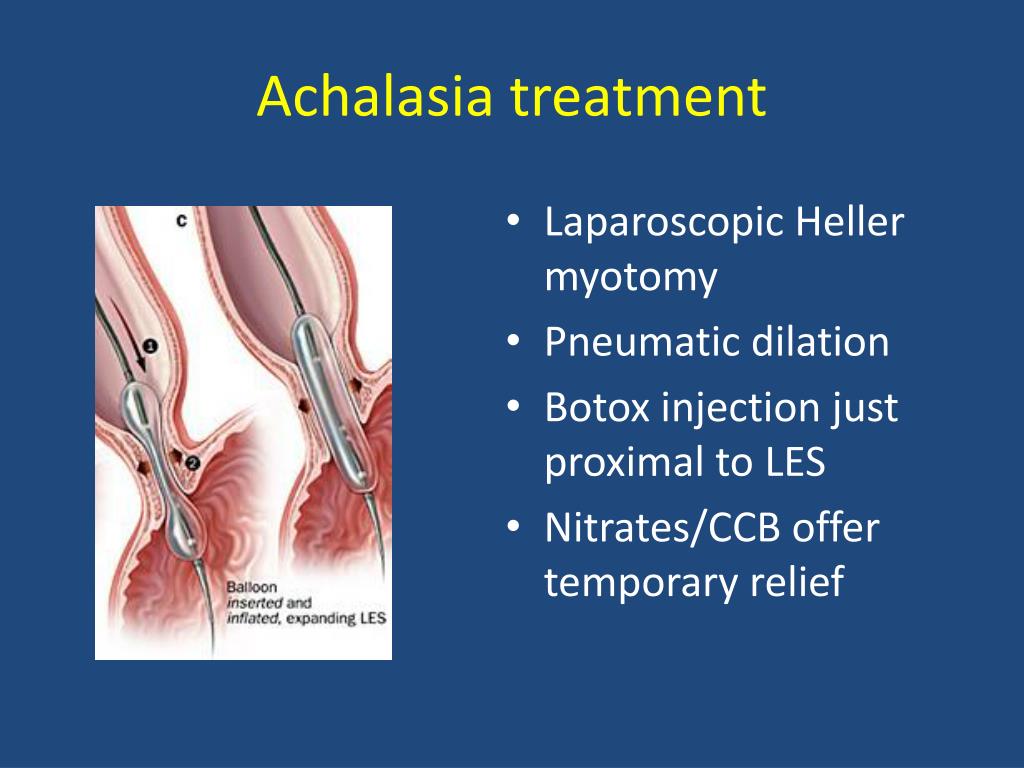
Laparoscopic myotomy should be the initial treatment for most patients with achalasia. Pneumatic dilatation is the most cost-effective alternative but its long-term efficacy is less than that of surgical myotomy.
Procedures
If both procedures are available by skilled operators, pneumatic dilation and surgery are equally effective in the treatment of achalasia. Treatment of achalasia: the best of …
Self-care
Apr 08, 2022 · Achalasia Treatment: Surgery. If you are a good candidate, and surgery is the best treatment option for you, your doctor may recommend that you go under the knife to treat your achalasia. Surgical treatment is often the best, most lasting treatment for those with type 1 achalasia (those that have an over-tightened LES).
Nutrition
Aug 12, 2021 · There is no cure for achalasia. The only treatment is surgery, where the lower esophageal sphincter can be opened so air can pass through. Achalasia is only diagnosed after extensive testing and should be suspected in certain patients. Diet: A usual diet such as fruits, nuts, vegetables high in roughage can help.
What are the surgical options for achalasia?
Durable achalasia treatments. Until recently, the only durable treatment options for achalasia were pneumatic dilation (PD) or laparoscopic Heller myotomy (LHM). Pneumatic dilation is done with a 30-, 35-, or 40-mm cylindrical balloon positioned across the LES fluoroscopically and inflated using a handheld manometer.
What should I eat if I have achalasia?
What outcome can I expect from the various treatment options? Balloon dilation improves symptoms in 50% to 93% of people with achalasia. Keep in mind that the procedure may need to... Minimally invasive surgery/laparoscopic Heller myotomy is effective in 76% to 100% of people with achalasia. Keep ...
Can achalasia be cured?
Treatment of patients with achalasia has evolved in recent years with the introduction of peroral endoscopic myotomy. Other treatment options include botulinum toxin injection, pneumatic dilation, and Heller
What is achalasia Cardia and its treatment options?

What is the latest treatment for achalasia?
Peroral Esophageal Myotomy (POEM) is a newer treatment for achalasia, and is considered an important advance in gastroesophageal surgery. POEM combines the use of an endoscope, a thin tube with a camera on the end, with a more minimally invasive surgical technique than Laparoscopic Heller Myotomy (LHM).Feb 26, 2018
How do you fix an achalasia?
There's no cure for achalasia. Once the esophagus is paralyzed, the muscle cannot work properly again. But symptoms can usually be managed with endoscopy, minimally invasive therapy or surgery.Mar 5, 2022
How do you treat achalasia without surgery?
Nonsurgical options include:Pneumatic dilation. A balloon is inserted by endoscopy into the center of the esophageal sphincter and inflated to enlarge the opening. ... Botox (botulinum toxin type A). This muscle relaxant can be injected directly into the esophageal sphincter with an endoscopic needle. ... Medication.Mar 5, 2022
How long can you live with achalasia?
In group A, the estimated 20-year survival rates in patients with achalasia [76% (95% confidence interval (CI): 66-85%)] did not significantly differ from those in controls 80% (95% CI: 71-89%). In group B, 25-year survival rates were also similar in patients [87% (95% CI: 78-97%)] and controls [86% (95% CI: 76-97%)].
Does a myotomy for achalasia?
The Heller myotomy is a laparoscopic (minimally invasive) surgical procedure used to treat achalasia. Achalasia is a disorder of the esophagus that makes it hard for foods and liquids to pass into the stomach.
What triggers achalasia?
What causes achalasia? In most cases, it's caused by loss of the nerve cells that control the swallowing muscles in the esophagus. Healthcare providers don't yet know why these nerve cells are lost. In rare cases, achalasia is caused by a tumor.
How do you fix a tortuous esophagus?
Esophagectomy: For patients experiencing severe symptoms such as severe dilation or tortuous esophagus, removal of the esophagus, or esophagectomy, may be recommended. This procedure removes and replaces a portion or the entire length of the esophagus to restore comfortable swallowing.
How do you strengthen your esophagus sphincter?
By lifting and holding the neck from a supine position for 60 seconds at a time, you create enough tension in the muscle associated with the upper esophageal sphincter that it can strengthen the valve.May 16, 2016
Why are calcium channel blockers used in achalasia?
For people with achalasia, these medications relax the muscles of the lower esophageal sphincter, allowing food and liquid to pass more easily into the stomach. Calcium channel blockers and nitrates are taken by mouth 10 to 30 minutes before a meal. They are available in tablets that can be absorbed under the tongue.
What can I drink with achalasia?
Achalasia patients will participate hot water drinking therapy: to drink 200ml of hot water before and after a meal, as well as 2 hours before sleep and to chew food carefully and swallow with hot soup. Patients are followed by achalasia associated symptom scores, barium esophagram and endoscopy.May 29, 2013
What foods to avoid if you have achalasia?
Achalasia is a disorder of the esophagus, or food pipe, which causes the cells and muscles to lose function....Foods to avoid include:citrus fruits.alcohol.caffeine.chocolate.ketchup.Sep 30, 2019
How serious is achalasia?
Is achalasia serious? Yes, it can be, especially if it goes untreated. If you have achalasia, you'll gradually experience increased trouble eating solid foods and drinking liquids. Achalasia can cause considerable weight loss and malnutrition.Apr 6, 2021
How to treat achalasia?
Surgical options for treating achalasia include: 1 Heller myotomy. The surgeon cuts the muscle at the lower end of the esophageal sphincter to allow food to pass more easily into the stomach. The procedure can be done noninvasively (laparoscopic Heller myotomy). Some people who have a Heller myotomy may later develop gastroesophageal reflux disease (GERD).#N#To avoid future problems with GERD, a procedure known as fundoplication might be performed at the same time as a Heller myotomy. In fundoplication, the surgeon wraps the top of your stomach around the lower esophagus to create an anti-reflux valve, preventing acid from coming back (GERD) into the esophagus. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. 2 Peroral endoscopic myotomy (POEM). In the POEM procedure, the surgeon uses an endoscope inserted through your mouth and down your throat to create an incision in the inside lining of your esophagus. Then, as in a Heller myotomy, the surgeon cuts the muscle at the lower end of the esophageal sphincter.#N#POEM may also be combined with or followed by later fundoplication to help prevent GERD. Some patients who have a POEM and develop GERD after the procedure are treated with daily oral medication.
How does achalasia work?
Achalasia treatment focuses on relaxing or stretching open the lower esophageal sphincter so that food and liquid can move more easily through your digestive tract. Specific treatment depends on your age, health condition and the severity of the achalasia.
Why is achalasia misdiagnosed?
Diagnosis. Achalasia can be overlooked or misdiagnosed because it has symptoms similar to other digestive disorders. To test for achalasia, your doctor is likely to recommend: Esophageal manometry.
What is endoscopy used for?
Endoscopy can be used to define a partial blockage of the esophagus if your symptoms or results of a barium study indicate that possibility. Endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications of reflux such as Barrett's esophagus. Read more about esophageal manometry and upper endoscopy.
What is a Heller myotomy?
Heller myotomy. The surgeon cuts the muscle at the lower end of the esophageal sphincter to allow food to pass more easily into the stomach. The procedure can be done noninvasively (laparoscopic Heller myotomy). Some people who have a Heller myotomy may later develop gastroesophageal reflux disease (GERD).
What is the procedure to remove acid from the stomach?
Fundoplication is usually done with a minimally invasive (la paroscopic) procedure. Peroral endoscopic myotomy (POEM).
What is a POEM procedure?
In the POEM procedure, the surgeon uses an endoscope inserted through your mouth and down your throat to create an incision in the inside lining of your esophagus. Then, as in a Heller myotomy, the surgeon cuts the muscle at the lower end of the esophageal sphincter.
What Are The Causes Of Achalasia
Actually is a disorder that affects the muscles of the esophagus, and it’s often referred to as a “reflux-type disorder.” Since the esophagus is a muscular tube, it can’t handle strong reflux (spitting up) for long periods of time.
What Are The Symptoms Of Achalasia?
Searching for symptoms of Achalasia can be a bit confusing since there are many different conditions that can cause problems with the brain and nerves. Brain fog can arise from a number of problems, some serious and some not so serious. Sometimes Achalasia is the result of a disease or a medication and can be very disabling.
What is the treatment for achalasia?
Several treatments are available for achalasia including nonsurgical options (balloon dilation, medications, and botulinum toxin injection) and surgical options. The goal of treatment is to relieve your symptoms by relaxing your lower esophageal sphincter (LES).
What is the procedure for achalasia?
The surgery used to treat achalasia is called laparoscopic esophagomyotomy or laparoscopic Heller myotomy. In this minimally invasive surgery, a thin, telescopic-like instrument called an endoscope is inserted through a small incision. The endoscope is connected to a tiny video camera – smaller than a dime –that projects a view of the operative site onto video monitors located in the operating room. In this operation, the muscle fibers of the LES are cut. The addition of another procedure called a partial fundoplication helps prevent gastroesophageal reflux, a side effect of the Heller myotomy procedure.
Why do nerve cells degenerate?
Your nerve cells, which control muscle function, slowly degenerate for reasons that are not currently understood. This results in excessive contractions in the LES. If you have achalasia, the LES fails to relax and food and liquids can’t pass through your esophagus into your stomach.
What is the condition where the esophagus is damaged?
Achalasia is a rare disorder in which damaged nerves in your esophagus prevent it from working as it should. Muscles at the lower end of your esophagus fail to allow food to enter your stomach. Symptoms include trouble swallowing, heartburn and chest pain. Treatment includes both nonsurgical (Botox injections, balloon dilation, medicines) and surgical options.
How many people have achalasia?
Achalasia develops in about 1 in every 100,000 people in the U.S. each year. It is typically diagnosed in adults between the ages of 25 and 60, but can occur in children as well (less than 5% of cases are in children under age 16).
What is the ring of muscle that allows food to enter the stomach?
At the area where your esophagus meets your stomach is a ring of muscle called the lower esophageal sphincter (LES). This muscle relaxes (opens) to allow food to enter your stomach and contracts (tightens to close) to prevent stomach content from backing up into your esophagus. If you have achalasia, the LES doesn’t relax, ...
How long does achalasia last?
Achalasia symptoms develop slowly, with symptoms lasting for months or years. Symptoms include: Trouble swallowing ( dysphagia ). This is the most common early symptom. Regurgitation of undigested food. Chest pain that comes and goes; pain can be severe. Heartburn. Cough at night.
