
What is a sham procedure in clinical trials?
A sham procedure can be defined as one performed on a control group participant to ensure that he or she experiences the same incidental effects of the operation or procedure as do those participants on whom a true operation is performed ( 7 ). Sham control arms, like other placebo control arms in controlled clinical trials, ...
What is a sham treatment group?
The purpose of a sham treatment group is to identify any specific benefit of one element of a medical treatment above and beyond all benefits that might be attributed to everything else about that treatment.
Does sham surgery really work?
Although this seems to defy common sense, many other trials of sham surgery have had positive results. In a Finnish study published in 2013, sham surgery was performed on patients suffering from torn knee ligaments, and in severe pain.
When are Sham Sham procedures justified?
Sham procedures are easily justified when they are of relatively low risk and used to evaluate invasive treatments for conditions with subjective outcomes, such as relief of pain. Thomas J. Krizek MD, in Plastic Surgery Secrets Plus (Second Edition), 2010
What is a sham procedure in research?
A sham procedure can be defined as one performed on a control group participant to ensure that he or she experiences the same incidental effects of the operation or procedure as do those participants on whom a true operation is performed (7).
How is sham surgery performed?
This is an aspect of the placebo effect known as “sham surgery.” This is when surgeons literally pretend to do an operation, doing everything they would normally do - for example, making an incision, picking up instruments, giving instructions to colleagues, then closing the incision - but without actually making an ...
What is a sham injection?
The injection of a placebo or agent that simulates a drug being administered in a clinical trial.
What is sham dosing?
Delivering drugs orally is often done by gavage, where a thin tube is inserted briefly into the stomach through the mouth. “Sham dosing” (dosing without administering the drug) is typically used before the treatment, on the basis that it should help familiarise dogs with the procedure.
Why is sham surgery used?
Sham surgery (placebo surgery) is an intervention that omits the step thought to be therapeutically necessary. In surgical clinical trials, sham surgery serves an analogous purpose to placebo drugs, neutralizing biases such as the placebo effect.
What is a sham in medical terms?
Sham surgery (placebo surgery) is a faked surgical intervention that omits the step thought to be therapeutically necessary.
What is the full form of sham?
SHAMAcronymDefinitionSHAMSelf Help and Actualization MovementSHAMSlope Height Area Moment (pharmacokinetic analysis)
What is a sham block?
In a sham block, the same intervention is performed, i.e., the block under investigation but instead of local anaesthetic (LA) or a pharmacologically active substance, a placebo (usually normal saline) is used.
Is sham surgery ethical?
Surgical clinical trials have seldom used a "sham" or placebo surgical procedure as a control, owing to ethical concerns. Recently, several ethical commentators have argued that sham surgery is either inherently or presumptively unethical.
What is a sham comparator?
A group of participants that receives a procedure or device that is made to be indistinguishable from the actual procedure or device being studied but does not contain active processes or components.
How does a placebo work?
A placebo is any treatment that has no active properties, such as a sugar pill. There are many clinical trials where a person who has taken the placebo instead of the active treatment has reported an improvement in symptoms. Belief in a treatment may be enough to change the course of a person's physical illness.
What are the different phases of clinical trials?
Phases of Clinical TrialsPhase 1 Clinical Trial. The purpose of Phase 1 is to ensure that the treatment is safe in humans and to determine how and where it distributes within the body. ... Phase 2 Clinical Trial. ... Phase 3 Clinical Trial. ... Monitoring Post-FDA Approval.
Why is sham procedure justified?
Sham procedures are easily justified when they are of relatively low risk and used to evaluate invasive treatments for conditions with subjective outcomes, such as relief of pain.
What is the gold standard for clinical evaluation of surgical or other treatment modalities?
The scientific gold standard for clinical evaluation of surgical or other treatment modalities is the randomized double-blind study. In such studies, the patients are randomly distributed among possible treatment groups.
What is Huang et al. (2011)?
Huang et al. (2011) searched for studies comparing no treatment, placebo or sham treatment, alarms , simple behavioral treatment, desmopressin, imipramine and miscellaneous drugs and interventions. There was weak evidence to support the use of hypnosis, psychotherapy, acupuncture, chiropractic and medicinal herbs but the studies were single small trials, some of dubious methodological rigor. Robust randomized trials are required with efficacy, cost-effectiveness and adverse effects clearly reported. They concluded that, as of the date of publication, alarms offer the best chance of a cure, and desmopressin may be used to reduce or stop wet nights during treatment.
What is a no treatment group?
The inclusion of a no-treatment group (e.g., wait list ) or putative sham treatment (e.g., pill placebo) in a study design is required to validly answer causal questions like “Does an intervention have certain effects?” A no-treatment or placebo condition to which subjects are randomly assigned and which continues for the same duration as a putative active treatment allows several rival explanations for a relationship between a treatment and outcomes to be dismissed. For example, if the outcomes associated with an active treatment are statistically better than the outcomes associated with a control treatment, then the active treatment outcomes cannot be attributed solely to changes that occur naturally with the passage of time, maturation, or “spontaneous remission.”
How can contamination of a control treatment occur?
Another way contamination of a control treatment can occur is via contact between the control subjects and those receiving the active treatments. For example, subjects in active treatments might give control subjects intervention materials (e.g., copies of intervention self-help workbooks).
Why is aesthetic surgery important?
Because the same apparent disfigurement, distortion, or merely disagreeable features can have such different meaning to different patients, the ability to establish objective criteria for correcting such problems is a true challenge. Although many studies have been done to interpret the psychological implications of such aesthetic problems, the best that has come from such studies are general patterns of patient concerns. Even more challenging is the problem of determining the actual degree of improvement or satisfaction that an operation accomplishes. The concept of impartiality is particularly true in these circumstances. Every surgeon anticipates and dearly wishes the end result to be happy and pleasing to both surgeon and patient. It makes scientific objectivity very difficult.
How large was the effect size of the invasive procedure?
The effect size of this study was moderate to large (0.69) and of the combined studies was 0.43, which is statistically significant (p < 0.03). 13,26 While it appears that invasive procedures can be effective beyond sham, one should note that the two studies were not consistent (one was effective and one was not) and the procedures and populations were markedly different from each other. More research is needed before such a procedure can be recommended.
Why is sham procedure justified?
Sham procedures are easily justified when they are of relatively low risk and used to evaluate invasive treatments for conditions with subjective outcomes, such as relief of pain.
What is the gold standard for clinical evaluation of surgical procedures?
The scientific gold standard for clinical evaluation of surgical or other treatment modalities is the randomized double-blind study. In such studies, the patients are randomly distributed among possible treatment groups. After the treatment the evaluation is accomplished by impartial persons not involved in the study and who themselves have no stake in profiting from the results, no matter what the outcome. Particularly with medications, neither the physicians nor the patients are aware of which drug is being administered lest any placebo effect be introduced. Such studies are ethically and scientifically difficult when surgical procedures are involved. “Sham” operations, involving only skin incisions as the control group, are ethically challenging. And yet, in several situations such as ligation of internal mammary operations for angina and some reconstructive procedures on the knee, the sham operation was equally effective.
What is Huang et al. (2011)?
Huang et al. (2011) searched for studies comparing no treatment, placebo or sham treatment, alarms , simple behavioral treatment, desmopressin, imipramine and miscellaneous drugs and interventions. There was weak evidence to support the use of hypnosis, psychotherapy, acupuncture, chiropractic and medicinal herbs but the studies were single small trials, some of dubious methodological rigor. Robust randomized trials are required with efficacy, cost-effectiveness and adverse effects clearly reported. They concluded that, as of the date of publication, alarms offer the best chance of a cure, and desmopressin may be used to reduce or stop wet nights during treatment.
What is a no treatment group?
The inclusion of a no-treatment group (e.g., wait list ) or putative sham treatment (e.g., pill placebo) in a study design is required to validly answer causal questions like “Does an intervention have certain effects?” A no-treatment or placebo condition to which subjects are randomly assigned and which continues for the same duration as a putative active treatment allows several rival explanations for a relationship between a treatment and outcomes to be dismissed. For example, if the outcomes associated with an active treatment are statistically better than the outcomes associated with a control treatment, then the active treatment outcomes cannot be attributed solely to changes that occur naturally with the passage of time, maturation, or “spontaneous remission.”
Why is aesthetic surgery important?
Because the same apparent disfigurement, distortion, or merely disagreeable features can have such different meaning to different patients, the ability to establish objective criteria for correcting such problems is a true challenge. Although many studies have been done to interpret the psychological implications of such aesthetic problems, the best that has come from such studies are general patterns of patient concerns. Even more challenging is the problem of determining the actual degree of improvement or satisfaction that an operation accomplishes. The concept of impartiality is particularly true in these circumstances. Every surgeon anticipates and dearly wishes the end result to be happy and pleasing to both surgeon and patient. It makes scientific objectivity very difficult.
How can contamination of a control treatment occur?
Another way contamination of a control treatment can occur is via contact between the control subjects and those receiving the active treatments. For example, subjects in active treatments might give control subjects intervention materials (e.g., copies of intervention self-help workbooks). To help prevent this threat to IV, subjects can be required, as part of the study informed consent, to refrain from sharing information about their respective treatments while a study is in progress.
Is the inclusion of control treatment conditions of some type compelling?
The inclusion of control treatment conditions of some type is logically very compelling as a way to increase an intervention study's IV. Unfortunately, the compelling logic is not mirrored in practice. Reams have been written on problems associated with designing placebo therapies that meet IV goals (e.g., O'Leary & Borkovec, 1978 ). For example, credibility is one issue ( Parloff, 1986 ). How can a placebo psychotherapy be developed that has no theoretically active therapeutic ingredients but that seems equally credible to subjects as a putative active treatment?
Why is sham surgery important?
This is because it isolates the specific effects of the treatment as opposed to the incidental effects caused by anesthesia, the incisional trauma, pre- and postoperative care, and the patient's perception of having had a regular operation.
Can sham animals be used as controls?
Historically, studies in animals also allowed the removal or alteration of an organ; using sham-operated animals as control, deductions could be made about the function of the organ. Sham intervention s can also be performed as controls when new surgical procedures are developed.
Is sham surgery good?
A review of studies with sham surgery found 53 such studies: in 39 there was improvement with the sham operation and in 27 the sham procedure was as good as the real operation. Sham-controlled interventions have therefore identified interventions that are useless but had been believed by the medical community to be helpful based on studies without the use of sham surgery.
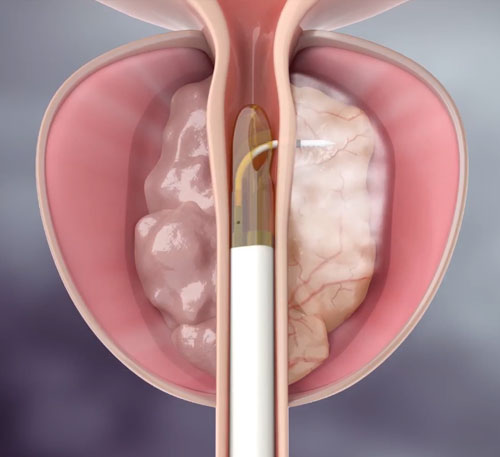
Can a sham procedure be performed under IRB approval?
With the progress in minimally invasive surgery, sham procedures can be more easily performed as the sham incision can be kept small similarly to the incision in the studied procedure.
Does arthroscopic surgery help with knee locking?
The fact that all three groups improved equally points to the placebo effect in surgical interventions. In a recent study it was found, that arthroscopic partial meniscectomy does not offer any benefit over sham (or fake) surgery in relieving symptoms of knee locking or catching in patients with degenerative meniscal tears.
Why are sham controls used in clinical trials?
These examples from the clinical trial literature support the conclusion that there is a role for sham controls in clinical trials of devices and procedures, particularly when used either to confirm or refute the results of open-label trials and in circumstances in which outcomes that are partially or entirely subjective are primary. However, while the use of sham controls is likely to provide the highest quality and potentially most generalizable clinical trial data, the use of a sham control must be carefully contemplated in light of its appropriateness and feasibility and applied within a formalized ethical framework. Only through a careful assessment of the risks to research subjects of being exposed to a sham control and of the knowledge that will be gained through direct comparison of a placebo to active device or procedure can investigators decide whether the use of a sham control versus a usual care control is most advantageous.
Why are sham controls useful?
Thus, sham controls are particularly useful for trials of devices or procedures with subjective endpoints (e.g., symptoms) and provide a robust means of controlling for the ancillary effects of a procedure, optimizing the ability of the investigator to evaluate for a placebo or procedural effect in an unbiased fashion.
What is the challenge of balancing trials?
The challenge when studying an intervention based on a procedure or medical device is one of balancing issues of trial design that optimize generalizability of the findings with those issues that optimize the protection of human subjects. This balance is alluded to in criteria for Institutional Review Board approval of research as outlined in the Code of Federal Regulations (45 CFR part 46), which indicates that risk to subjects must be minimized by using procedures that are consistent with sound research design but that do not unnecessarily expose subjects to risk. Furthermore, the risk to subjects should be considered to be reasonable in relationship to anticipated benefits and the importance of the knowledge that may be reasonably expected to result (5). In the example of clinical trials of orally administered agents, balancing safety and efficacy is often relatively straightforward, as a placebo tablet or capsule is typically associated with minimal to no risk when administered to a research subject. In trials of devices or procedures, however, the placebo control is often a sham intervention that differs only minimally from the active or effective procedure and that may expose subjects to a degree of risk similar to that of the active procedure. A recent search of the ClinicalTrials.gov database (6) revealed that studies using a sham control are relatively infrequent, with only 65 of 15,805 actively recruiting protocols (0.4%) involving a sham control.
Is placebo a sham?
In trials of devices or procedures, however, the placebo control is often a sham intervention that differs only minimally from the active or effective procedure and that may expose subjects to a degree of risk similar to that of the active procedure.
Is a sham control arm attractive?
The attractiveness of including a sham control arm increases in cases in which the risk of the sham procedure is particularly low, and studies considering a sham control should carefully consider risk versus benefit.
Is sham surgery a placebo?
One example from the medical literature in which sham surgery has been used as a form of placebo control is Parkinson's Disease, a disorder of motor function with loss of dopaminergic neurons in the substantia nigra. Its clinical course is notable for marked variability in both the magnitude and duration of response to medical therapy, and multiple clinical trials in Parkinson's Disease have shown a substantial placebo effect, with a 20 to 30% improvement in motor scores seen over periods as long as six months ( 9 ), with deterioration in clinical status after the discontinuation of placebo and with an apparent cumulative dose–response increase to placebo therapy over time ( 10 ). Early open-label trials of surgical transplantation of embryonic dopaminergic tissue transplantation into the brain had suggested that both clinical and radiographic benefits could be observed ( 10 ). In these studies, the surgical intervention required stereotactic frame placement, MRI targeting of the transplantation site, general anesthesia, a skin incision, creation of a burr hole and then transplantation of fetal tissue, followed by cyclosporine for 6 months in addition to continued medical therapy. When sham-controlled clinical trials were performed to follow up prior open-label studies, in which control subjects underwent a nearly identical procedure but with only a partial burr hole and no transplantation of fetal tissue, it was determined that the active procedure was associated with no significant improvement in outcomes versus the sham procedure, and the authors of one study concluded that “fetal nigral transplantation currently cannot be recommended as a therapy for Parkinson's disease based on these results” ( 4 ). Although ethical issues were raised about the appropriateness of these studies as they were being designed and conducted ( 10, 11 ), ultimately the inclusion of a sham control arm in these rigorous studies demonstrated that the procedure had little apparent clinical effect, a result that stood in contrast to prior uncontrolled studies. Although issues of small sample size and questions about the effect on recruitment of public discourse on the ethics of these trials reduce the definitive nature of these results, this example from the literature appears to be one where, had sham-controlled studies not been performed, clinicians might have continued to expose patients to an ineffective surgical therapy.
