Medication
Results: Osteomyelitis usually requires some antibiotic treatment, usually administered systemically but sometimes supplemented by antibiotic-containing beads or cement. Acute hematogenous osteomyelitis can be treated with antibiotics alone. Chronic osteomyelitis, often accompanied by necrotic bone, usually requires surgical therapy.
Procedures
· empiric antibiotics for acute hematogenous osteomyelitis should include an anti-staphylococcal antibiotic such as nafcillin or oxacillin, though vancomycin should be substituted when mrsa is suspected. 13, 15 additional coverage against gram-negative enteric bacteria, for example a third-generation cephalosporin such as cefotaxime, should be …
Self-care
· Osteomyelitis treatment requires a multifaceted approach that may include antibiotics, surgical intervention, and other modalities depending on multiple clinical factors, including clinical stage.
Nutrition
Treatments include: Antibiotics: Antibiotics kill infection-causing bacteria. You may need antibiotics for four to eight weeks, starting... Antifungals: To treat fungal infections, you may need to take oral antifungal medications for months. Needle aspiration: Your healthcare provider uses a …
What is the life expectancy of someone with osteomyelitis?
The goal for treatment of osteomyelitis is to cure the infection and minimize any long-term complications. Treatment may include: Medications. Administration of intravenous (IV) antibiotics, which may require hospitalization or may be given on an outpatient schedule. Intravenous or oral antibiotic treatment for osteomyelitis may be very extensive, lasting for …
Does osteomyelitis always require surgery?
· Acute hematogenous osteomyelitis in children typically can be treated with a four-week course of antibiotics. In adults, the duration of antibiotic treatment for chronic osteomyelitis is typically...
Does osteomyelitis ever heal?
· Most people with osteomyelitis are treated with antibiotics, surgery, or both. Antibiotics help bring the infection under control and often make it …
How long should osteomyelitis last?
Effective antimicrobial therapy is an essential component of most curative treatment regimens for osteomyelitis. In stage 1 osteomyelitis, such as acute medullary osteomyelitis of the long bones or vertebrae, appropriately targeted antimicrobial therapy alone without other therapeutic measures may be adequate to achieve eradication of infecting organisms and cure of …

What is the main cause of osteomyelitis?
Most cases of osteomyelitis are caused by staphylococcus bacteria, types of germs commonly found on the skin or in the nose of even healthy individuals. Germs can enter a bone in a variety of ways, including: The bloodstream.
Can osteomyelitis be cured?
Most cases of osteomyelitis are treatable. Chronic infections of the bone, however, may take longer to treat and heal, especially if they require surgery. Treatment should be aggressive because an amputation can become necessary sometimes.
What is the best treatment for osteomyelitis?
The most common treatments for osteomyelitis are surgery to remove portions of bone that are infected or dead, followed by intravenous antibiotics given in the hospital....SurgeryDrain the infected area. ... Remove diseased bone and tissue. ... Restore blood flow to the bone. ... Remove any foreign objects. ... Amputate the limb.
How long does it take to cure osteomyelitis?
Treatment for osteomyelitis You'll usually take antibiotics for 4 to 6 weeks. If you have a severe infection, the course may last up to 12 weeks. It's important to finish a course of antibiotics even if you start to feel better.
How serious is osteomyelitis?
Osteomyelitis is a serious condition that requires immediate treatment. Most bone infections go away when you take antibiotics. Be sure to take all your prescribed medication even if you start feeling better. Stopping medications too soon can allow the infection to return.
Is osteomyelitis an emergency?
Symptoms that might indicate a serious condition In some cases, osteomyelitis can be a serious condition that should be immediately evaluated in an emergency setting. Osteomyelitis may spread to the bloodstream and lead to a widespread infection.
Can osteomyelitis be cured without surgery?
Non-surgical treatment of osteomyelitis requires a multidisciplinary team approach including primary care, infectious disease specialist care, nutritionist care and wound care. These wounds will require antibiotic therapy for a duration of six to eight weeks.
What is the most common bone site of osteomyelitis?
Among children and teens, the long bones of the legs and arms are most frequently affected. In adults, osteomyelitis most often affects the vertebrae of the spine and/or the hips. However, extremities are frequently involved due to skin wounds, trauma and surgeries.
What are common local signs of osteomyelitis?
Osteomyelitis is often diagnosed clinically on the basis of nonspecific symptoms such as fever, chills, fatigue, lethargy, or irritability. The classic signs of inflammation, including local pain, swelling, or redness, may also occur and usually disappear within 5-7 days.
How do you get osteomyelitis?
Osteomyelitis is inflammation or swelling that occurs in the bone. It can result from an infection somewhere else in the body that has spread to the bone, or it can start in the bone — often as a result of an injury. Osteomyelitis is more common in younger children (five and under) but can happen at any age.
How quickly does osteomyelitis spread?
Acute osteomyelitis develops rapidly over a period of seven to 10 days. The symptoms for acute and chronic osteomyelitis are very similar and include: Fever, irritability, fatigue.
Can osteomyelitis lead to sepsis?
An infection of the bone, called osteomyelitis, could lead to sepsis. In people who are hospitalized, bacteria may enter through IV lines, surgical wounds, urinary catheters, and bed sores.
Who Is Affected by Osteomyelitis?
Osteomyelitis can affect both adults and children. The bacteria or fungus that can cause osteomyelitis, however, differs among age groups. In adult...
What Causes Osteomyelitis?
It can be caused by a variety of microbial agents (most common in staphylococcus aureus) and situations, including: 1. An open injury to the bone,...
What Are The Symptoms of Osteomyelitis?
The symptoms of osteomyelitis can include: 1. Pain and/or tenderness in the infected area. 2. Swelling, redness and warmth in the infected area. 3....
How is osteomyelitis managed?
Osteomyelitis is best managed by a multidisciplinary team. It requires accurate diagnosis and optimization of host defenses, appropriate anti-infective therapy, and often bone débridement and reconstructive surgery.
How to treat osteomyelitis?
Treating osteomyelitis: antibiotics and surgery. Osteomyelitis is best managed by a multidisciplinary team. It requires accurate diagnosis and optimization of host defenses, appropriate anti-infective therapy, and often bone débridement and reconstructive surgery.
Can osteomyelitis be chronic?
It can affect all ages and involve any bone. Osteomyelitis may become chronic and cause persistent morbidity. Despite new imaging techniques, diagnosis can be difficult and often delayed. Because infection can recur years after apparent "cure," "remission" is a more appropriate term.
What are the different types of osteomyelitis?
Osteomyelitis has traditionally been classified into three categories.1The first category, hematogenous osteomyelitis , is bone infection that has been seeded through the bloodstream. The second, osteomyelitis due to spread from a contiguous focus of infection without vascular insufficiency, is seen most often after trauma or surgery, and is caused by bacteria which gain access to bone by direct inoculation (for example, a contaminated compound fracture) or extension to bone from adjacent contaminated soft tissue (for example, a prosthetic joint contaminated at the time of implantation). The third category, osteomyelitis due to contiguous infection with vascular insufficiency, is seen almost exclusively in the lower extremities, most commonly as a diabetic foot infection. Each of these three categories of osteomyelitis can present in the acute or chronic phase, in virtually any bone, caused by a variety of bacteria and occasionally fungi. Thus, the approach to osteomyelitis should be guided by several principles, but must be individualized to each unique situation.
Why is osteomyelitis complex?
Because of the heterogeneity of disease severity, anatomic location, organism, and host, treatment of osteomyelitis is complex, and must be individualized. However, several general concepts guide therapy (Table 2).
What antibiotics should I use for acute hematogenous osteomyelitis?
Empiric antibiotics for acute hematogenous osteomyelitis should include an anti-staphylococcal antibiotic such as nafcillin or oxacillin, though vancomycin should be substituted when MRSA is suspected.13,15Additional coverage against gram-negative enteric bacteria, for example a third-generation cephalosporin such as cefotaxime, should be added in newborns, and considered in older children. Empiric gram-negative coverage is also warranted in adults; quinolones are useful in this population.
What is the gold standard for diagnosis of osteomyelitis?
The gold standard for the diagnosis of osteomyelitis is bone biopsy with histopathologic examination and tissue culture. When the patient is clinically stable, one should consider delaying empiric antimicrobial treatment until bone biopsy is performed. An open approach is ideal to ensure that adequate specimen is obtained, particularly when prosthetic material is involved.7Needle biopsy is often used, and the sensitivity and specificity using this modality has been reported as 87% and 93%, respectively.8Specimens should undergo both aerobic and anaerobic bacterial culture. In addition, fungal and mycobacterial cultures should be performed when clinical suspicion of these organisms is present.
What are the symptoms of osteomyelitis?
Patients usually present with signs of acute infection such as fever, chills, pain, and local signs of inflammation.4 In adults, the most common site is the vertebral bodies, followed by long bones, pelvis, and clavicle. The primary blood supply of the vertebrae is the segmental arteries, which divide to perfuse segments of two adjacent vertebrae. Thus, vertebral osteomyelitis often occurs in two contiguous vertebral bodies and the intervertebral disc.5
How does osteomyelitis affect bone?
In experimental models, a large inoculum of bacteria is typically required to induce osteomyelitis.2Bacteria possess a variety of virulence factors that contribute to the development and chronicity of osteomyelitis, such as proteins called adhesins which facilitate attachment to bone3, and the ability to form biofilm, a slime layer which shields the bacteria from antimicrobial agents.4In addition, the host's immune response to infection can damage bone. Several common cytokines have osteolytic properties, and phagocytes produce toxic oxygen radicals and proteolytic enzymes that can harm host cells. The inflammatory response leads to an increase in intraosseous pressure, which impairs blood flow and leads to ischemic necrosis. This dead bone, known as a sequestrum,1can act as a non-living surface for biofilm attachment, allowing bacteria to adopt a lower metabolic rate and to survive in an environment with lower oxygen tension.. Poor blood flow as well as biofilm make it difficult for antimicrobial agents and host immune cells to access the bacteria.4
Can osteomyelitis be diagnosed with an ulcer?
The diagnosis of osteomyelitis may be difficult. If an ulcer is present on exam, osteomyelitis is present if bone is visible, or if bone is encountered when the ulcer is probed with a sterile instrument.5However, the inability to probe to bone does not rule out osteomyelitis.
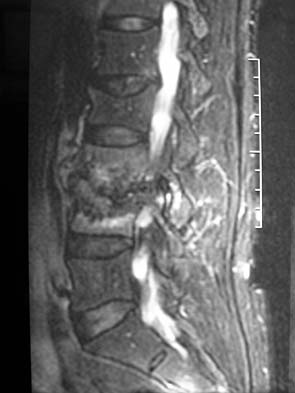
How to diagnose osteomyelitis?
Osteomyelitis is usually clinically diagnosed with support from imaging and laboratory findings. Bone biopsy and microbial cultures offer definitive diagnosis. Plain film radiography should be performed as initial imaging, but sensitivity is low in the early stages of disease. Magnetic resonance imaging with and without contrast media has a higher sensitivity for identifying areas of bone necrosis in later stages. Staging based on major and minor risk factors can help stratify patients for surgical treatment. Antibiotics are the primary treatment option and should be tailored based on culture results and individual patient factors. Surgical bony debridement is often needed, and further surgical intervention may be warranted in high-risk patients or those with extensive disease. Diabetes mellitus and cardiovascular disease increase the overall risk of acute and chronic osteomyelitis.
What are the symptoms of osteomyelitis?
A diagnosis of osteomyelitis should be considered in any patient with acute onset or progressive worsening of musculoskeletal pain accompanied by constitutional symptoms such as fever, malaise, lethargy, and irritability. Constitutional symptoms do not always occur in adults, especially in the setting of immunocompromise. The index of suspicion for osteomyelitis should be higher in patients with underlying conditions, including poorly controlled diabetes mellitus, neuropathy, peripheral vascular disease, chronic or ulcerated wounds, history of recent trauma, sickle cell disease, history of implanted orthopedic hardware, or a history or suspicion of intravenous drug use. A dedicated physical examination can increase the likelihood of diagnosing osteomyelitis if findings include erythema, soft tissue infection, bony tenderness, joint effusion, decreased range of motion, or exposed bone. The probe-to-bone test may be useful to rule out diabetic foot osteomyelitis in low-risk patients. 10, 11
What is the most common pathogen for osteomyelitis?
Methicillin-sensitive Staphylococcus aureus is the most frequently identified pathogen across all types of osteomyelitis, followed by Pseudomonas aeruginosa and methicillin-resistant S. aureus. Hematogenous osteomyelitis is often monomicrobial and can occur from aerobic gram-negative rods or from P. aeruginosa or Serratia marcescens in injection drug users. 4 Vertebral osteomyelitis is the most common type of hematogenous osteomyelitis and is polymicrobial in 5% to 10% of cases. 1 Blood cultures may be negative if osteomyelitis develops following bacterial clearance from the bloodstream. Nonhematogenous osteomyelitis can be polymicrobial; S. aureus is the most common pathogen in addition to coagulase-negative staphylococci and gram-negative aerobes and anaerobes. Polymicrobial diabetic foot infections and decubitus ulcers may include Streptococcus species and Enterococcus species. 1 Less common pathogens can be associated with certain clinical conditions, including immunocompromise ( Aspergillus species, Mycobacterium tuberculosis, Candida species), sickle cell disease ( Salmonella species), HIV infection ( Bartonella henselae ), and tuberculosis ( M. tuberculosis ). 1, 5, 6
What is the differential diagnosis of osteomyelitis?
The differential diagnosis of osteomyelitis includes soft tissue infection, gout, Char-cot arthropathy, fracture, malignancy, bursitis, osteonecrosis, sickle cell vasoocclusive pain crisis, and SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis). Uncertain clinical diagnosis should prompt further workup that includes laboratory evaluation and imaging ( Table 1 2, 9, 12, 13). Definitive diagnosis is made with a positive culture from biopsy of the affected bony structure. Polymerase chain reaction testing may help in the rapid diagnosis of organisms or for cultures taken after antibiotic therapy. 12, 14 Bone biopsy remains the diagnostic standard but is not always feasible. Some evidence suggests that biopsy should be reserved only for select cases because the results may not lead to treatment alterations. 15
What is the best diagnostic test for osteomyelitis?
The preferred diagnostic criterion for osteomyelitis is a positive bacterial culture from bone biopsy , but clinical, laboratory, and radiographic findings can also inform a clinical diagnosis. 9, 12
Can diabetic neuropathy cause osteomyelitis?
Patients with diabetic neuropathy are at higher risk of developing osteomyelitis secondary to local spread from diabetic foot infections and unrecognized wounds. 2 Smoking increases the risk of osteomyelitis from diabetic foot infections and healing fractures. 7 Peripheral vascular disease and poorly healing wounds (e.g., decubitus ulcers) are more likely to lead to bone inflammation. Osteomyelitis secondary to diabetic foot ulcers can be difficult to diagnose given chronic changes from vascular insufficiency and ischemia. 8
Can osteomyelitis be diagnosed with MRI?
MRI is more readily available and avoids radiation exposure, but positron emission tomography (PET) and single-photon emission computed tomography (SPECT) can also reliably diagnose osteomyelitis. 25 In patients in whom MRI is contraindicated, a tagged leukocyte scan, computed tomography (CT), PET/CT, or sulfur colloid marrow scan can be appropriate; however, diagnosis may be impeded because of false-positive results from recent surgery or trauma, healed osteomyelitis, arthritis, bony tumors, Paget disease of bone, or reduced uptake secondary to necrosis and poor blood flow. 13, 29, 30 Ultrasonography plays a complementary role to other modalities and may demonstrate inflammatory changes in the periosteum, particularly in children. Ultrasonography can be useful for identification of soft tissue abscess and helpful for abscess aspiration. 13
Why is it important to treat osteomyelitis?
The objective of treating osteomyelitis is to eliminate the infection and prevent the development of chronic infection. Chronic osteomyelitis can lead to permanent deformity, possible fracture, and chronic problems, so it is important to treat the disease as soon as possible.
How to treat osteomyelitis in the spine?
Instead, patients with spinal osteomyelitis are given intravenous antibiotics. After surgery, antibiotics against the specific bacteria involved in the infection are then intensively administered during the hospital stay and for many weeks afterward.
What is the disease that can cause bone tissue death?
Osteomyelitis. Osteomyelitis is an infection of the bone that can affect both adults and children. If left untreated, it can lead to bone tissue death over time. Appointments 216.444.2606. Appointments & Locations. Contact Us. Overview. Symptoms and Causes. Diagnosis and Tests.
What is osteomyelitis infection?
What is osteomyelitis? Osteomyelitis is a bacterial, or fungal, infection of the bone. Osteomyelitis affects about 2 out of every 10,000 people. If left untreated, the infection can become chronic and cause a loss of blood supply to the affected bone.
How do you know if you have osteomyelitis?
The symptoms of osteomyelitis can include: Pain and/or tenderness in the infected area. Swelling, redness and warmth in the infected area. Fever. Nausea, secondarily from being ill with infection. General discomfort, uneasiness, or ill feeling. Drainage of pus (thick yellow fluid) through the skin.
What causes a bone to break out?
It can be caused by a variety of microbial agents (most common in staphylococcus aureus) and situations, including: An open injury to the bone, such as an open fracture with the bone ends coming out through the skin.
Is osteomyelitis more common in the tibia or humerus?
They include the femur and tibia in the legs and the humerus and radius in the arms. Osteomyelitis is not more common in a particular race or gender. However, some people are more at risk for developing the disease, including: People with diabetes. Patients receiving hemodialysis.
How long does osteomyelitis last?
Intravenous or oral antibiotic treatment for osteomyelitis may be very extensive, lasting for many weeks.
Which immune system is more likely to develop osteomyelitis?
Individuals with weakened immune systems are more likely to develop osteomyelitis. This includes people with sickle cell disease or HIV or those receiving immunosuppressive medications like chemotherapy or steroids.
What tests are done to check for osteomyelitis in children?
The provider treating your child will first do a thorough history and physical exam that may indicate signs of osteomyelitis like those listed above. An additional workup generally includes blood tests that look at white blood cells as well as markers for inflammation that are usually elevated during an infection.
What is the term for swelling of bone tissue?
Osteomyelitis is an inflammation or swelling of bone tissue that is usually the result of an infection. Bone infection may occur for many different reasons and can affect children or adults. Osteomyelitis may occur as a result of a bacterial bloodstream infection, sometimes called bacteremia, or sepsis, that spreads to the bone.
What is the term for inflammation of the bone?
Osteomyelitis is inflammation or swelling that occurs in the bone. It can result from an infection somewhere else in the body that has spread to the bone, or it can start in the bone — often as a result of an injury. Osteomyelitis is more common in younger children (five and under) but can happen at any age. Boys are usually more affected ...
What are the long term complications of osteomyelitis?
Osteomyelitis requires long-term care to prevent further complications, including care to prevent the following: Fractures of the affected bone. Stunted growth in children (if the infection has involved the growth plate) Gangrene infection in the affected area.
How do you know if you have osteomyelitis?
The following are the most common symptoms of osteomyelitis; however, each individual may experience symptoms differently: Fever (may be high when osteomyelitis occurs as the result of a blood infection) Pain and tenderness in the affected area. Irritability in infants who can’t express pain. Feeling ill.
Where does osteomyelitis occur?
It typically involves the vertebrae, but can occur in the long bones, pelvis, or clavicle. Patients with vertebral osteomyelitis often have underlying medical conditions (e.g., diabetes mellitus, cancer, chronic renal disease) or a history of intravenous drug use. 12 Back pain is the primary presenting symptom.
How long does it take for osteomyelitis to recur?
In adults, the duration of antibiotic treatment for chronic osteomyelitis is typically several weeks longer.
Why is osteomyelitis a bacteremic disease?
Acute hematogenous osteomyelitis results from bacteremic seeding of bone. Children are most often affected because the metaphyseal (growing) regions of the long bones are highly vascular and susceptible to even minor trauma.
How to diagnose osteomyelitis in children?
Acute osteomyelitis in children is primarily a clinical diagnosis based on the rapid onset and localization of symptoms. Systemic symptoms such as fever, lethargy, and irritability may be present. The physical examination should focus on identifying common findings, such as erythema, soft tissue swelling or joint effusion, decreased joint range of motion, and bony tenderness. The identification of a bacterial infection may be difficult because blood cultures are positive in only about one-half of cases. 15 Because of the difficulty of diagnosis, the potential severity of infection in children, the high disease recurrence rate in adults, and the possible need for surgical intervention, consultation with an infectious disease subspecialist and an orthopedic subspecialist or plastic surgeon is advised. 16
What is the best diagnostic test for osteomyelitis?
The preferred diagnostic criterion for osteomyelitis is a positive bacterial culture from bone biopsy in the setting of bone necrosis.
Why is osteomyelitis more common in diabetics?
Chronic osteomyelitis from contiguous soft tissue infection is becoming more common because of the increasing prevalence of diabetic foot infections and peripheral vascular disease. Up to one-half of patients with diabetes develop peripheral neuropathy, which may reduce their awareness of wounds and increase the risk of unrecognized infections. 13 Peripheral vascular disease, which is also common in patients with diabetes, reduces the body's healing response and contributes to chronically open wounds and subsequent soft tissue infection. These conditions may act synergistically to significantly increase the risk of osteomyelitis in these patients. 14
How long does it take for osteomyelitis to show symptoms?
Acute osteomyelitis is associated with inflammatory bone changes caused by pathogenic bacteria, and symptoms typically present within two weeks after infection.
How to treat osteomyelitis?
Most people with osteomyelitis are treated with antibiotics, surgery, or both.
Why is it important to treat osteomyelitis early?
In cases of acute osteomyelitis, early treatment prevents the condition from becoming a chronic problem that requires ongoing treatment . Besides the pain and inconvenience of repeated infections, getting osteomyelitis under control early provides the best chance for recovery.
What is the condition where bone is infected?
Osteomyelitis. Osteomyelitis is an infection of the bone, a rare but serious condition. Bones can become infected in a number of ways: Infection in one part of the body may spread through the bloodstream into the bone, or an open fracture or surgery may expose the bone to infection.
How long does it take for osteomyelitis to develop?
Symptoms of Osteomyelitis. Acute osteomyelitis develops rapidly over a period of seven to 10 days. The symptoms for acute and chronic osteomyelitis are very similar and include: Osteomyelitis in the vertebrae makes itself known through severe back pain, especially at night.
What is the cause of osteomyelitis?
In most cases, a bacteria called Staphylococcus aureus, a type of staph bacteria, causes osteomyelitis. Certain chronic conditions like diabetes may increase your risk for osteomyelitis.
How to prevent osteomyelitis in children?
The best way to prevent osteomyelitis is to keep things clean. If you or your child has a cut, especially a deep cut, wash it completely. Flush out any open wound under running water for five minutes, then bandage it in sterile bandages.
How many people get osteomyelitis?
Only 2 out of every 10,000 people get osteomyelitis. The condition affects children and adults, although in different ways. Certain conditions and behaviors that weaken the immune system increase a person's risk for osteomyelitis, including: Diabetes (most cases of osteomyelitis stem from diabetes) Sickle cell disease.
How long should antimicrobial therapy be for osteomyelitis?
Consensus recommendations for duration of curative antimicrobial therapy for most patients with osteomyelitis who have received “stage-appropriate” surgical interventions remain a minimum of 4 to 6 weeks.1,5Patients with more extensive infections and limited surgery may require more prolonged treatment; those with Cierney type 2 disease and adequate surgery may only require 2 weeks of treatment. In practice, clinicians often adopt a “goal-directed” approach to treatment duration, using clinical assessment and normalization of inflammatory markers (C-reactive protein and/or sedimentation rates) to define duration of therapy. Inflammatory markers have been proved useful in managing acute hematogenous pediatric osteomyelitis and in one recent study correlated with success of therapy in pyogenic vertebral osteomyelitis, but their role in determining duration of therapy in adults has not been thoroughly evaluated.16,17
What animal model is used for osteomyelitis?
Much of the current approach to osteomyelitis is based on animal infection models. The most widely employed are variations of the rabbit Staphylococcus aureusmodel developed by Norden and colleagues in the late 1960s.11More recently developed sheep, goat, and dog large-animal models permit manipulation of surgical parameters as well as evaluation of antimicrobial therapy.12,13Animal models have contributed to understanding of revascularization and bone remodeling that occur after infection and debridement and have demonstrated effectiveness of agents such as clindamycin and rifampin-containing combinations in S. aureusinfections.11,12However, some drugs are toxic in animal models, and for others there is poor correlation between animal data and clinical experience. For example, vancomycin fared poorly in the rabbit models but has been used successfully in many human infections.12
What is daptomycin used for?
Daptomycin is a novel, parenteral cyclic lipopeptide with a unique bactericidal mechanism of action against gram-positive pathogens.43Daptomycin was noninferior to vancomycin for treatment of skin and soft tissue infections and for S. aureusand MRSA bacteremia. The approved dose for S. aureusbacteremia is 6 mg/kg every 24 hours. There is limited data on human daptomycin bone levels. Clinical experience with 67 osteomyelitis patients from a registry of patients receiving daptomycin was recently published.44Sixty-three percent were cured and 19% improved in this heterogeneous group of patients, most of whom had MRSA infections. Predominant toxicity is to skeletal muscle, and creatine phosphokinase should be monitored.
What is the best treatment for S. aureus?
Minocycline is extensively used as an oral option for community-acquired MRSA soft tissue infections. A recent review of clinical experience with tetracyclines for MRSA infections found few published reports of osteomyelitis treated with minocycline.38Several newer agents with good in vitro and in vivo activity against MRSA have recently been introduced. These include linezolid , daptomycin, and tigecycline. The optimal use of these agents and their role in treatment of acute and chronic osteomyelitis and comparative activity to intravenous vancomycin are still being evaluated. The best studied of these is linezolid, a bacteriostatic, protein synthesis inhibitor of the novel oxazolidinone class. Linezolid is active against S. aureusincluding nearly all MRSA strains, though resistance can very infrequently develop on therapy. Linezolid has nearly 100% oral bioavailability and demonstrates good bone penetration, with bone levels in healthy adults undergoing hip replacement surgery of 50% of serum levels.39Linezolid has demonstrated success rates comparable with or superior to those of vancomycin in clinical trials of skin and soft tissue infections and comparable with those of ampicillin-sulbactam for diabetic foot infections. Published experience with linezolid for osteomyelitis was recently reviewed by Falagas and colleagues, including case reports, analysis of data from the linezolid compassionate-use program, and several small prospective case series7,40,41,42Successful outcomes or cure were reported in 55 to 100% of published cases.41Toxicities of linezolid after more than 2 weeks include anemia and thrombocytopenia, thus hematologic parameters must be monitored, although in one small trial, rates were similar for vancomycin and linezolid therapy.42Other serious toxicities reported with prolonged linezolid therapy include lactic acidosis syndromes, optic neuritis, and peripheral neuropathy7,41In one study, 80% of 66 patients with chronic S. aureusosteomyelitis were cured after prolonged courses of linezolid (mean 13 weeks), but treatment-limiting toxicities occurred in one third of patients.7Thus, linezolid is not an ideal agent for very prolonged treatment courses or chronic suppressive therapy.
What is the best antibiotic for methicillin resistant Staphylococcus aureus?
Beta-lactam antimicrobials remain the drugs of choice for nonallergic patients with methicillin-susceptible Staphylococcus aureus(MSSA) infections.1Less than 5% of S. aureusis still susceptible to penicillin; for such strains, intravenous penicillin G is used at doses of 3 to 4 million units every 4 to 6 hours. For other MSSA, the penicillinase-resistant penicillin drugs (oxacillin, nafcillin, flucloxacin) given intravenously have traditionally been considered the drugs of choice.1The first-generation cephalosporin cefazolin allows more convenient every-8-hour dosing and may have a better safety profile with lower rates of neutropenia and hypersensitivity and has been found equivalent to nafcillin or oxacillin in a retrospective study.10Dosing for bone infection is 2 g every 8 hours in adults with normal renal function. Broad spectrum third- and fourth-generation cephalosporins have also been used for MSSA infections, due to their more convenient dosing schedules, though this must be weighed against the impact of their broader spectrum of action and suppression of normal host bacterial flora and impact on resistance. Ceftriaxone is particularly attractive due to its once-daily dosing schedule, although the MICs of ceftriaxone against MSSA are generally higher than those of cefazolin, raising concern for potential treatment failure. Two retrospective studies showed no difference in relapse rates for ceftriaxone or cefazolin therapy in patients with S. aureusosteomyelitis.10,20Serum levels of parenteral β-lactams exceed the MIC of susceptible MSSA throughout most of the dosing interval. Such levels cannot reliably be achieved with oral regimens, due to their more limited oral bioavailability. Bone levels, typically 10 to 20% of serum levels, are even less likely to remain above the MIC. Thus, parenteral therapy is almost always preferred for curative β-lactam regimens.1One exception to this is acute pediatric osteomyelitis, where oral “step-down” therapy with β-lactam agents has been successfully used after an initial 1- to 2-week course of parenteral therapy.21,22There is less data supporting use of oral β-lactam therapy in adults.
Why is antimicrobial therapy important?
The goal of administering antimicrobial therapy is to optimize antimicrobial activity at the site of infection. Generally, this also correlates with achievable serum levels of drug, though there are some exceptions where volume of distribution of a drug is large and drug concentrations in tissues may exceed achievable serum levels. The route of administration is much less important than whether desired blood and tissue levels can be achieved, thus drugs with good to excellent oral bioavailability such as fluoroquinolones and linezolid can be given orally or enterally in patients with functional gastrointestinal tracts.7,8Several studies have demonstrated equivalence of appropriately chosen oral agents compared with parenteral therapy.8,9For the patient, oral therapy has advantages of simplicity and convenience, especially for prolonged treatment regimens, and avoids the risks of intravenous catheters and the generally higher costs associated with long-term parenteral therapy. For some agents with both oral and parenteral formulations, especially penicillins and cephalosporins, parenteral therapy provides much higher serum levels, or may be better tolerated than the high oral doses necessary to achieve target serum levels. Many important antimicrobials, including broad-spectrum cephalosporins, vancomycin, aminoglycosides, and carbapenems, can only be delivered intravenously. Agents with parenteral and oral bioequivalence are listed in Table Table1.1. A major evolution in health care has been improvement in delivery of long-term parenteral antimicrobial therapy.10The availability of long-term intravenous access options such as peripherally inserted central catheters has simplified the process of antibiotic delivery. The proliferation of outpatient infusion services now permits patients to receive appropriately monitored treatment at home or at infusion centers rather than in acute- or intermediate-care hospitals. Insurance and social issues may still be barriers to arranging outpatient intravenous therapy. Therapy of bone and joint infection is the second most common indication for outpatient intravenous antimicrobial therapy.10In addition to the primary considerations of spectrum of action and toxicity for choosing antimicrobial agents, other factors such as drug costs and convenience of the treatment regimen (e.g., dosing frequency, need for laboratory monitoring) must be considered.
What is the most important parameter in selecting an antimicrobial agent for treatment of bone infection?
The single most important parameter in selecting an antimicrobial agent for treatment of bone infection is its spectrum of activity —is the drug active against the targeted pathogen? Standard susceptibility tests provide in vitro data to assess a particular “drug-bug” combination, and generally lack of susceptibility in vitro correlates with clinical failure. However, susceptibility as determined by minimal inhibitory concentration (MIC) or disk diffusion testing does not necessarily predict clinical success. Susceptibility interpretations are based on achievable serum levels, and these may differ significantly from levels achievable in bone in surrounding tissue. In healthy bone specimens removed at surgery, levels of cefazolin and other cephalosporins may range from 10 to 20% of serum levels,1and levels may be even lower in diseased tissues with poor vascular perfusion. Drugs also differ in ability to penetrate biofilms or function in the specific pH and oxidative microenvironment where infection occurs. Infecting organisms, especially those in more chronic infections, may also be slowly replicating or in near-stationary growth phase and thus less responsive to many classes of antimicrobial agents. Much information regarding activity of different agents has been extrapolated from well-established animal models, but there remains a paucity of published clinical experience in humans with many of the newer antimicrobial agents and even some of the older drugs.3,4,5The mechanism of activity of an antimicrobial agent and whether it is bactericidal (lethal) or bacteriostatic (inhibitory) in vitro is not as important for successful treatment of osteomyelitis as it is for other difficult-to-eradicate infections such as bacterial endocarditis. However, the pharmacodynamic properties (i.e., the relationship between drug concentration and activity against the target organism over time) of an antibiotic and the relative ease of selection of antimicrobial-resistant mutants for different agents are theoretical parameters that may be important in antibiotic selection.6
