HALO ablation, or radiofrequency ablation, is a treatment option for patients who have suffered from abnormal cell growth in the esophagus known as Barrett’s esophagus. The condition occurs when chronic acid reflux or gastroesophageal reflux disease (GERD) goes untreated over time, causing damage to the lining of your esophagus.
What is Barrett’s esophagus and how is it treated?
Barrett’s Esophagus is a change in the type of esophageal tissue that regrows in place of esophageal tissue that is damaged by acid reflux. Not everyone that has reflux symptoms has Barrett’s Esophagus; however, if one develops Barrett’s Esophagus there is a chance of developing esophageal cancer.
What is Halo treatment for esophageal cancer?
If a longer segment is present, the HALO device is advanced into the esophagus and the same time of controlled and directed heat treatment is applied with the scope along side the device. Since it is a minimally invasive procedure, the patient will be under monitored anesthesia care throughout the process.
Can Halo ablation eliminate Barrett’s disease completely?
More than one upper endoscopy and ablation may be needed, but studies have shown that in 98.4% of patients, Barrett’s tissue can be completely eliminated with HALO ablation. What are the complications of HALO ablation treatments?
What is cryoablation for Barrett's esophagus?
Cryoablation involves freezing the Barrett’s esophagus cells to purposefully injure them and stimulate regeneration of normal tissue.

What is the best treatment for Barrett's esophagus?
Preferred treatments include: Endoscopic resection, which uses an endoscope to remove damaged cells to aid in the detection of dysplasia and cancer. Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue. Radiofrequency ablation may be recommended after endoscopic resection.
Is esophageal ablation painful?
The procedure itself is not usually painful, as the patient is sedated during the procedure. It is, however, common for the patient to feel chest pain and discomfort swallowing for no longer than seven days after the procedure.
How do you keep your Barrett's esophagus from progressing?
Getting plenty of fiber in your daily diet is good for your overall health. Medical research shows that it may also help prevent Barrett's esophagus from worsening and lower your risk of cancer in the esophagus. Add these and other fiber-rich foods to your daily diet: fresh, frozen, and dried fruit.
What is Halo treatment esophagus?
The Halo procedure uses heat energy (radiofrequency ablation) combined with EGD (esophagogastroduodenoscopy). The heat from electrodes at the end of the tube (endoscope) used in the procedure destroys abnormal tissue in the esophagus. The heat is exact to the abnormal area and doesn't damage healthy tissue.
How long does it take for the esophagus to heal after ablation?
A modified diet is recommended for the first three days after the procedure to allow time for healing. Patients may return to work the day after the procedure. All patients with Barrett's esophagus will also be treated with high-dose antacids (typically in the proton pump inhibitor family) indefinitely.
How often should someone with Barrett's esophagus be checked?
Surveillance endoscopy is recommended every three to five years for patients with Barrett esophagus without dysplasia, every six to 12 months for those with low-grade dysplasia, and every three months for those with high-grade dysplasia (if not eradicated).
What are the signs that Barrett's esophagus is getting worse?
The development of Barrett's esophagus is most often attributed to long-standing GERD , which may include these signs and symptoms:Frequent heartburn and regurgitation of stomach contents.Difficulty swallowing food.Less commonly, chest pain.
How long does it take for Barrett's esophagus to become cancerous?
This cohort study showed that the incubation period from Barrett esophagus to invasive cancer is likely more than 30 years.
Are there stages of Barrett's esophagus?
DISEASE PROGRESSION AND COMPLICATIONS Barrett's esophagus can progress to more serious stages, potentially resulting in esophageal adenocarcinoma, a type of esophageal cancer. There are three stages of Barrett's esophagus, which range from intestinal metaplasia without dysplasia to high-grade dysplasia.
What can you eat after Halo surgery?
Eat a liquid diet for 24 hours after your procedure:Water, juice, and broth.Coffee and tea.Milk, ice cream, and yogurt (with no fruit in it)Gelatin, pudding, and custard (with no fruit in them)Soup with no meat, pasta, or vegetables in it (such as tomato soup)
Does ablation cure Barrett's esophagus?
How effective is radiofrequency ablation therapy? Overall, RFA completely removes Barrett's esophagus and dysplasia in a high proportion of patients, as shown in results from multiple clinical studies. The success rate is about 80 to 90 percent.
What happens after an ablation of the esophagus?
It is very common to experience significant chest pain which may last for a number of days. Sometimes the pain is severe enough that even drinking water may be very uncomfortable. For 48 hours after the procedure, you should consume a full liquid-only diet.
How long does it take for Barrett's esophagus to heal?
Studies show that when the Barrett’s tissue is removed, it is typically replaced by normal, healthy tissue within three to four weeks.
What is Halo ablation?
The HALO ablation procedure specifically targets only the layer of diseased tissue without harming the healthy structures underneath it. Combined with treatments to control acid production, this technique allows normal esophageal tissue to replace the intestinal metaplasia.
What is the term for the damage to the esophagus?
In patients with gastroesophageal reflux disease (GERD), stomach acid and enzymes can injure the esophageal lining. Over time, this damage can cause inflammation and genetic changes to esophageal cells, causing them to become intestinal tissue. This disorder is called “intestinal metaplasia” or Barrett’s esophagus.
What causes Barretts esophagus?
The exact causes of Barrett’s esophagus are not known. It is thought that damage to the lining of the esophagus from stomach acid and enzymes causes esophageal cells to change.
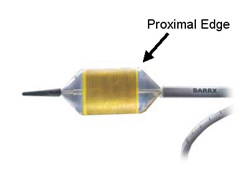
What is HALO Ablation?
Ablation therapy is performed during an upper endoscopy by the doctor using a HALO ablation catheter. Heat energy is delivered through the catheter in a precise manner to destroy the thin Barrett’s esophageal tissue until it is no longer viable or alive.
What are the complications of HALO ablation treatments?
Along with a very slight chance of adhesion (sticking together) of the esophageal tissue after ablation treatment, the risks and complications of HALO radiofrequency ablation are similar to those of an upper endoscopy with sedation.
What will I feel from ablation treatment?
During the upper endoscopy you will be sedated and feel nothing. Many people have no discomfort after the ablation. Some people have slight chest discomfort or difficulty swallowing for a few days after the treatment. The doctor will prescribe medicine (s) to manage this discomfort.
What is the treatment for Barrett's esophagus?
Gastroenterologists at Johns Hopkins developed the use of cryoablation therapy, an effective treatment for Barrett's esophagus. Ablation therapy may cause Barrett's esophagus to regress. Medications will be given to suppress your stomach acid. Then, during an endoscopy, thermal injury is administered to the abnormal mucous lining.
What is the name of the doctor who treats Barrett's esophagus?
Doctors at Johns Hopkins are at the forefront of diagnosing and treating Barrett's esophagus. In fact, gastroenterologists at Hopkins pioneered the use of cryoablation, a revolutionary new therapy, to treat Barrett's esophagus.
How often do you need an endoscopy for Barrett's?
Patients with low-grade dysplasia may need an endoscopy every three to six months. Patients with high-grade dysplasia may need to undergo an esophagectomy (removal of the esophagus) because of the increased risk of cancer.
What is the goal of surgery for reflux disease?
Some patients prefer a surgical approach as an alternative to a lifetime of taking medications. The goal of surgery for reflux disease is to strengthen the anti-reflux barrier.
What is endoscopic surveillance?
This means that you undergo periodic endoscopic examinations to evaluate whether the condition has evolved into cancer. Your doctor looks for increasing degrees of dysplasia, the abnormal growth of cells, and may perform a biopsy on the area to check for cancerous tissue.
What is the screening for Barrett's esophagus?
Screening for Barrett's esophagus. Barrett's esophagus has a distinct appearance when viewed during an endoscopy exam. During endoscopy, the doctor passes a flexible tube with a video camera at the tip (endoscope) down your throat and into the swallowing tube (your esophagus).
What is the best way to remove abnormal esophagus tissue?
Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue. Radiofrequency ablation may be recommended after endoscopic resection. Cryotherapy, which uses an endoscope to apply a cold liquid or gas to abnormal cells in the esophagus. The cells are allowed to warm up and then are frozen again.
What is the best treatment for esophageal cancer?
But, given the risk of esophageal cancer, treatment may be recommended if the diagnosis is confirmed. Preferred treatments include: Endoscopic resection , which uses an endoscope to remove damaged cells to aid in the detection of dysplasia and cancer. Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue.
What is the procedure to remove a hernia?
GERD surgery. GERD surgery. Laparoscopic anti-reflux surgery for GERD may involve a procedure to reinforce the lower esophageal sphincter, called Nissen fundoplication. In this procedure, the surgeon wraps the top of the stomach around the lower esophagus after reducing the hiatal hernia, if present.
How to treat GERD?
Treatment for GERD. Medication and lifestyle changes can ease your signs and symptoms. Surgery or endoscopy procedures to correct a hiatal hernia or to tighten the lower esophageal sphincter that controls the flow of stomach acid may be an option.
What is the tube that is passed down your throat?
A lighted tube with a camera at the end (endoscope) is passed down your throat to check for signs of changing esophagus tissue. Normal esophagus tissue appears pale and glossy. In Barrett's esophagus, the tissue appears red and velvety. Your doctor will remove tissue (biopsy) from your esophagus. The biopsied tissue can be examined to determine ...
Is Barrett's esophagus a low grade or high grade?
No dysplasia, if Barrett's esophagus is present but no precancerous changes are found in the cells. Low-grade dysplasia, if cells show small signs of precancerous changes. High-grade dysplasia, if cells show many changes. High-grade dysplasia is thought to be the final step before cells change into esophageal cancer.
What is the treatment for Barrett's esophagus?
If you have Barrett’s esophagus and gastroesophageal reflux disease (GERD), your doctor will treat you with acid-suppressing medicines called proton pump inhibitors (PPIs). These medicines can prevent further damage to your esophagus and, in some cases, heal existing damage.
How does Barrett's mucosal resection work?
In endoscopic mucosal resection, your doctor lifts the Barrett’s tissue, injects a solution underneath or applies suction to the tissue, and then cuts the tissue off. The doctor then removes the tissue with an endoscope. Gastroenterologists perform this procedure at certain hospitals and outpatient centers. You will receive local anesthesia to numb your throat and a sedative to help you relax and stay comfortable.
What is endoscopic ablative therapy?
Endoscopic ablative therapies use different techniques to destroy the dysplasia in your esophagus. After the therapies, your body should begin making normal esophageal cells. A doctor, usually a gastroenterologist or surgeon, performs these procedures at certain hospitals and outpatient centers.
What is the procedure to numb your throat?
You will receive local anesthesia to numb your throat and a sedative to help you relax and stay comfortable. Before performing an endoscopic mucosal resection for cancer, your doctor will do an endoscopic ultrasound. Complications can include bleeding or tearing of your esophagus.
How long does it take to recover from esophageal surgery?
The surgery is performed at a hospital. You’ll receive general anesthesia, and you’ll stay in the hospital for 7 to 14 days after the surgery to recover.
Can you have anti-reflux surgery for GERD?
Your doctor may consider anti-reflux surgery if you have GERD symptoms and don’t respond to medicines. However, research has not shown that medicines or surgery for GERD and Barrett’s esophagus lower your chances of developing dysplasia or esophageal adenocarcinoma. .