What are the long-term risks of GBS?
The symptoms of GBS often progress quickly and thus require hospitalization for urgent treatment. There are two treatments that may help speed up recovery from GBS: Intravenous immunoglobulin therapy (IVIG) : This is an infusion of antibodies (the proteins that your body uses to fight foreign invaders) that has been collected from tens of thousands of other people.
Does Guillain Barre go away?
· How is Guillain-Barré treated? There is no known cure for Guillain-Barré syndrome. However, some therapies can lessen the severity of the illness and shorten recovery time. There are also several ways to treat the complications of the disease.
How long does Guillain Barre syndrome last?
· Antibiotics are effective treatment for group B strep infection in adults. The choice of antibiotic depends on the location and extent of the infection and your specific circumstances. If you're pregnant and you develop complications due to group B strep, you'll be given oral antibiotics, usually penicillin, amoxicillin (Amoxil, Larotid) or cephalexin (Keflex).
Can Guillain Barre be cured?
GBS is the most common peripheral neuropathy causing respiratory paralysis. Despite advances in respiratory management and immunotherapy, mortality from GBS is as high as 20% for ventilated patients. Mechanical ventilation is usually required by one third of the patients. [ 59]

What causes GBS?
GBS most commonly causes bacteremia, sepsis, pneumonia, and meningitis in newborns. It is very uncommon for GBS to cause meningitis in adults.
What is the best treatment for GBS?
The most commonly used treatment for Guillain-Barré syndrome is intravenous immunoglobulin (IVIG). When you have Guillain-Barré syndrome, the immune system (the body's natural defences) produces harmful antibodies that attack the nerves. IVIG is a treatment made from donated blood that contains healthy antibodies.
Is GBS can be cured?
There is no known cure for GBS. But treatments can help improve symptoms of GBS and shorten its duration. Given the autoimmune nature of the disease, its acute phase is typically treated with immunotherapy, such as plasma exchange to remove antibodies from the blood or intravenous immunoglobulin.
How long does GBS take to recover?
Guillain-Barre syndrome (GBS) may last between 14 and 30 days and you may slowly recuperate from it. Usually, recovery takes 6 to 12 months, but for some people, it could take up to 3 years.
Can GBS cause death?
Guillain-Barré syndrome (GBS) is a life-threatening polyradiculoneuropathy with a reported mortality rate of 3% to 13%. 1–6 The most frequently described causes of death in GBS are respiratory failure, pneumonia, cardiac arrest, and autonomic dysfunction.
Does GBS cause weight loss?
Patients with GBS are at high risk for inadequate nutrition throughout the course of their illness. Gastrointestinal symptoms produce dehydration and weight loss even prior to hospital admission.
Who is at risk for GBS?
Risk for serious GBS disease increases as people get older. Adults 65 years or older are at increased risk compared to adults younger than 65 years old.
How long does Guillain-Barre last?
GBS usually lasts between 14 and 30 days. If your symptoms continue longer, you may be suffering from a chronic form of GBS called chronic inflammatory demyelinating polyneuropathy and will need more aggressive treatment.
Does GBS shorten life expectancy?
Less than 1% of people with Guillain-Barre syndrome experience complications, and even fewer die. Once Guillain-Barre syndrome goes into remission, life-expectancy doesn't seem to be affected.
Can Covid trigger Guillain-Barré syndrome?
In two-thirds of cases, Guillain-Barre syndrome (GBS) is an autoimmune inflammatory disease affecting the nerve roots and peripheral nerves, preceded by a recent infection [2]. There have been many reported cases of GBS following COVID-19 infection, showing a possible association between the two entities.
Is GBS painful?
Conclusions: Pain is a common and often severe symptom in the whole spectrum of GBS (including MFS, mildly affected, and pure motor patients). As it frequently occurs as the first symptom, but may even last for at least 1 year, pain in GBS requires full attention.
What are the first signs of the onset of Guillain-Barré syndrome?
What are the symptoms of GBS?Difficulty with eye muscles and vision.Difficulty swallowing, speaking, or chewing.Pricking or pins and needles sensations in the hands and feet.Pain that can be severe, particularly at night.Coordination problems and unsteadiness.Abnormal heart beat/rate or blood pressure.More items...
What is the best treatment for GBS?
Doctors usually treat GBS disease with a type of antibiotic called beta-lactams, which includes penicillin and ampicillin. Sometimes people with soft tissue and bone infections may need additional treatment, such as surgery. Treatment will depend on the kind of infection caused by GBS bacteria.
What to do if you suspect someone has GBS?
Diagnosis. If doctors suspect someone has GBS disease, they will take samples of sterile body fluids. Examples of sterile body fluids are blood and spinal fluid. Doctors look to see if GBS bacteria grow from the samples (culture).
How many babies die from GBS?
However, 2 to 3 in every 50 babies (4% to 6%) who develop GBS disease will die. GBS bacteria may also cause some miscarriages, stillbirths, and preterm deliveries. However, many different factors can lead to stillbirth, pre-term delivery, or miscarriage. Most of the time, the cause for these events is not known.
Can a chest x-ray show a GBS infection?
Doctors may also order a chest x-ray to help determine if someone has GBS disease. Sometimes GBS bacteria can cause urinary tract infections (UTIs or bladder infections). Doctors use a sample of urine to diagnose urinary tract infections.
Can a baby die from GBS?
Babies may have long-term problems, such as deafness and developmental disabilities, due to having GBS disease. Babies who had meningitis are especially at risk for having long-term problems. Care for sick babies has improved a lot in the United States. However, 2 to 3 in every 50 babies (4% to 6%) who develop GBS disease will die.
How to treat GBS?
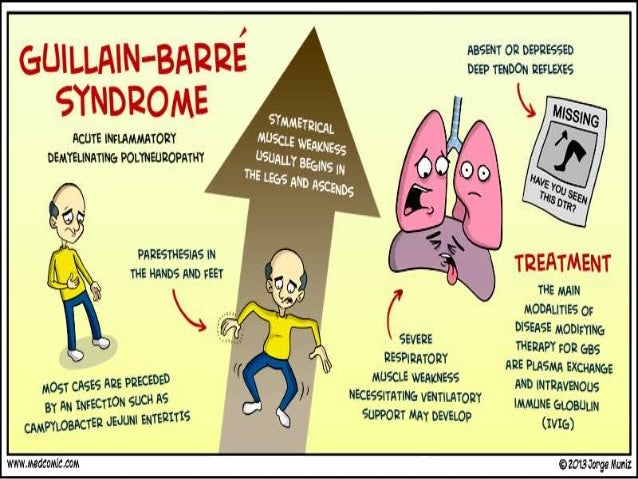
The symptoms of GBS often progress quickly and thus require hospitalization for urgent treatment. There are two treatments that may help speed up recovery from GBS: 1 Intravenous immunoglobulin therapy (IVIG): This is an infusion of antibodies (the proteins that your body uses to fight foreign invaders) that has been collected from tens of thousands of other people. This infusion helps calm down your body’s immune system attack on your nerves. 2 Plasma exchange (plasmapheresis): This is a procedure that involves filtering the liquid part of your blood (known as plasma). During this filtering process, your body’s antibodies which are attacking the nerves are removed and the “cleaned” plasma is returned back to your body. This helps stop the body’s immune system from continuing to attack your nerves.
What is the diagnosis of GBS?
Like many diseases, the diagnosis of GBS is largely based on a patient’s symptoms as well as their neurologic examination. A healthcare provider may also need to order tests to rule out other diseases that may present with similar symptoms as GBS.
What is the purpose of cerebrospinal fluid analysis?
The main goal of the analysis is to look for signs of other diseases which could appear similar to GBS (such as an infection of the nervous system) as well particular findings which support a diagnosis of GBS.
What is spinal tap?
Spinal tap (this is also known as a lumbar puncture): A spinal tap is a procedure that allows for the sampling of the cerebrospinal fluid (i.e. the fluid which surrounds your spinal cord and brain). During this procedure, a small needle is inserted into the back. A small amount of cerebrospinal fluid is then removed and sent for analysis. The main goal of the analysis is to look for signs of other diseases which could appear similar to GBS (such as an infection of the nervous system) as well particular findings which support a diagnosis of GBS.
Is GBS inherited or contagious?
GBS isn't contagious and it's not passed down through families (it isn' t an inherited disease).
What causes GBS?
GBS is usually triggered by a viral or bacterial infection. Rarely, viral or bacterial components (proteins) can appear to look similar to your body’s proteins. When this happens, your immune system becomes confused and starts to attack your body. When the nerves are attacked by your immune system, this can result in GBS.
Can older people get GBS?
While anyone can potentially get GBS, the syndrome is more commonly found in older people.
What is the best treatment for group B strep?
Antibiotics are effective treatment for group B strep infection in adults. The choice of antibiotic depends on the location and extent of the infection and your specific circumstances.
What tests are done to determine if a baby has B strep?
If your baby appears ill, he or she might be given other tests, including: Urine culture. Lumbar puncture. Chest X-ray.
What is a GBS?
Guillain–Barré syndrome (GBS) is an acute onset, usually monophasic immune-mediated disorder of the peripheral nervous system. The term GBS is often considered to be synonymous with acute inflammatory demyelinating polyradiculoneuropathy (AIDP), but with the increasing recognition of variants over the past few decades, the number of diseases that fall under the rubric GBS have grown to include axonal variants and more restricted variants, such as Miller Fisher syndrome (MFS) [Table 1].[1]
How to manage GBS?
Patients with GBS who are symptomatic but are able to walk unaided for more than 5 m and who are stable can be managed conservatively at peripheral centers. However, they should be observed for progression of the disease, especially if they are still within the first week of the onset of the disease. Blood pressure and heart rate fluctuations, clinical signs of respiratory failure should be carefully and meticulously monitored. Clinical signs of ileus should be watched. If any of these signs are detected they should be immediately shifted to specialized centers for further management. In the acute phase in bed-bound adult patients require both supportive therapy and immunotherapy can be used taking into consideration the cost factors and the clinical status (staging, complications, and other comorbid conditions) of individual patients.
What is the common electrolyte abnormality in GBS?
Hyponatremiais the common electrolyte abnormality in GBS and is due to SIADH (in majority of the cases) and natriuresis. The treatment is different for both. Both require replenishment of sodium but SIADH need fluid restriction and in case of natriuresis requires intravascular volume expansion. The best way to differentiate these two conditions is by measuring central venous pressure.
What is the most common cause of death in GBS patients?
Acute dysautonomia is a significant cause of death in patients with GBS. Cardiac and hemodynamic disturbance manifesting as hypertension, postural hypotension, and tachycardia occur in a majority of GBS patients.[69] This is due to excessive sympathetic over activity and parasympathetic under activity. Severe dysautonomia occurs usually in severe cases at the peak of the deficit.[69] Tachycardia is most common, usually in the range of 100–120/min, which does not require treatment. Approach to inserting a pacemaker for serious bradycardia or sinus arrest has varied widely because of the uncertainty that exists in anticipating such events at the bed side by different ways. However, the presence of tachycardia, increased daily variation in systolic blood pressure, reduced normal respiratory-induced heart rate variation, and first episode of severe bradyarrhythmia reduce the threshold for insertion of pacemaker.[70,71] Endotrachial suction may provoke bradycardia or systole, and this can be reduced by hyperoxygenation. Hypertension is seen in one third of patients with GBS and can be labile or be followed by hypotension.[63–65] If hypertension is severe (mean pressure greater than approximately 125 mmHg) and sustained, specific therapy may be necessary. Antihypertensives with short half-lives (labetolol, esmolol, or nitroprusside infusions) should be considered.[65] Beta-adrenergic or calcium channel blockers should be used with caution, especially if episodes of hypertension alternate with hypotension. Hypotension can be managed by maintaining intravascular volume and avoid using diuretics. Patients with a risk of hypotension should not be left unattended in a sitting or upright position. Pronounced and persistent hypotension should warrant search for other causes, such as sepsis myocardial infarction and pulmonary thromboembolism or use of narcotics or positive pressure ventilation. Gastrointestinal motility disorders occur in 15% of severely affected GBS patients. Ileus is associated with other features of dysautonomia (tachycardia and hypertension). Dysmotility can be effectively managed by suspension of enteral feeds, nasogastric suctioning, and erythromycin or neostigmine.[59,69]
How common is GBS?
The reported incidence rates for GBS are 1–2 per 100,000 population .[2–4] The lifetime likelihood of any individual acquiring GBS is 1:1000.[5] The subtypes of GBS have different incidence rates in different parts of the world. In Europe and North America AIDP is dominant contributing to 90% of the cases. In contrast in China and Japan AMAN being the most common subtype.[6,7] The picture is intermediate when we look at other population. In Indian series the incidence of AIDP and AMAN are virtually equal although AMAN is more common in younger patients.[8] There seems to be a slight preponderance of AIDP in studies by Gupta et al[9] and by Meena et al (unpublished data from NIMS, Hyderabad). Available Indian literature indicates a peak incidence between June–July and Sept–October.[10] In western countries, GBS is common in the 5thdecade,[11] but in India it occurs more commonly at a younger age.[10,12] GBS is equally common in men and women and can occur at any age. There is a male preponderance among the hospitalized population.[10,12]
What is the most recognizable variant of GBS?
MFS: The more recognizable and distinct regional variant of GBS is MFS. [1,45,46] Like GBS, the onset of MFS often follows an infection, for example C. jejuni.[47] MFS patients classically present with external ophthalmoparesis, areflexia, and ataxia,[2] although MFS patients often present with fewer components of the classical clinical triad[1,46,48,49] or with additional clinical features (facial weakness, oropharyngeal weakness, internal ophthalmoparesis, central nervous system involvement). Bickerstaffs brainstem encephalitis (BBE) is a related syndrome in which alteration of consciousness or conticospinal tract signs are seen in addition to ophthalmoparesis and ataxia. Many patients with MFS or BBE also have “overlapping GBS” with flaccid quadriparesis.[46,50] Anti-GQ1b antibodies are present in 95% of patients with acute MFS [51] and in approximately two-thirds of patients with BBE. The recognition of various clinical presentations and the high sensitivity and specificity of anti-GQ1b antibody testing suggest rubric name of “anti-GQ1b antibody syndrome.”
What is EDX in GBS?
Electrodiagnostic (EDX) testing is performed to support the clinical impression. EDX testing of GBS patients often demonstrates features of demyelination, such as temporal dispersion, significantly slow conduction velocities, and prolonged distal and F-wave latencies.[24] Electrodiagnostic testing features of acquired demyelination (eg, conduction block, temporal dispersion, nonuniform slowing of conduction velocities) are particularly helpful because these findings are characteristic of immune-mediated demyelinating neuropathies. In early GBS, prolonged distal compound muscle action potential (CMAP) latencies and temporal dispersion are more commonly demonstrated than are slow motor conduction velocities and conduction block.[27] Another electrodiagnostic testing hallmark of GBS is the “sural sparing” pattern; that is, the finding of a normal sural sensory nerve response in the setting of abnormal upper extremity sensory nerve results.[27] This pattern is very unusual for neuropathies other than GBS. Sural sparing, a marker of demyelinating neuropathy, is more commonly seen in later than in early stages of AIDP. Other electrodiagnostic testing abnormalities are frequently encountered in early GBS but they are less specific to GBS. These include absent H-reflexes, low motor nerve CMAP amplitudes on distal stimulation, and prolonged F-wave responses.[25–27] It is reported that the H-reflex was absent in 97% of GBS patients within the first week of symptom onset. It should also be pointed out that motor electrodiagnostic testing findings are more often abnormal than sensory nerve results in early GBS. Blink reflex studies are often abnormal when there is facial nerve involvement.[26] Phrenic nerve conduction studies can be used to predict respiratory failure and the need for ventilation.[28] Reduced CMAP amplitudes of 0%–20% of the lower limit of normal carry a poor prognosis.[29]
How to recover from GBS?
In some cases, in order to speed recovery, the doctor will take blood from your body, “clean” it, and then return it to you. This process is called plasmapheresis. Your doctor may give you immunoglobulin, or antibodies.
How long does GBS last?
A small number of people also have permanent nerve damage. GBS usually lasts between 14 and 30 days. If your symptoms continue longer, you may be suffering from a chronic form of GBS called chronic inflammatory demyelinating polyneuropathyand will need more aggressive treatment. WebMD Medical Reference .
How long do you stay in hospital for GBS?
Some people with GBS need to be hospitalized for a few days. Others stay for several weeks.
How long does it take for a GBS to show up?
It usually shows up a few days or weeks after a cold, stomach virus, or the flu. In rare cases, surgery or vaccinations can trigger it. You may hear your doctor mention “campylobacter.” That’s a type of bacteria associated with GBS.
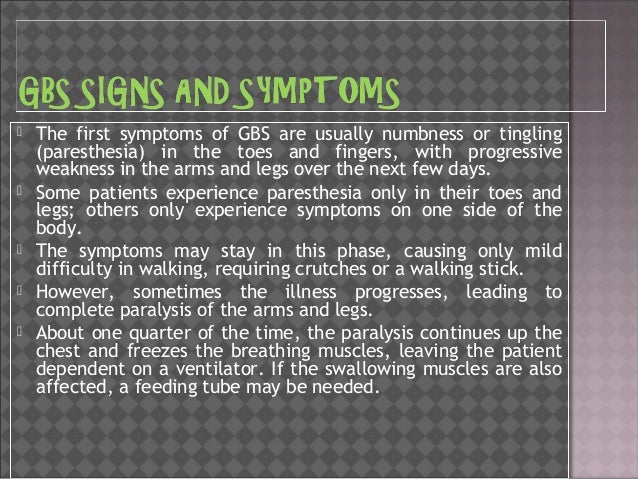
How do you know if you have Guillain Barre syndrome?
You usually feel it first in your arms and legs. You may notice muscle weakness or a “pins and needles” tingling in your hands and feet, which later moves toward your midsection. You may also feel unusually tired. Your reflexes may slow.
Can a virus cause GBS?
No one’s sure if a germ or virus, like the Zika virus, causes GBS . It could be that some illnesses alter your nerve cells, so your immune system starts to view them as threats. Others think your immune system forgets which cells it shouldn’t attack.
How to diagnose GBS?
To diagnose GBS, you may have the following tests: Spinal tap (lumbar puncture). A special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. The pressure in the spinal canal and brain can then be measured.
Why do some people get GBS?
It’s not clear why some people get GBS. What is known is that the body's immune system begins to attack the body itself.
What is the blood product that helps to decrease the immune system's attack on the nervous system?
Immunoglobulin is a blood product that helps to decrease the immune system’s attack on the nervous system.
What is the procedure that removes the plasma and replaces it with other fluids?
Plasmapheresis is a procedure that removes the plasma (liquid part of the blood) and replaces it with other fluids. Antibodies are also removed with the plasma, which is thought to help reduce the symptoms of the disease.
Is GBS a life threatening condition?
GBS is a medical emergency and needs to be treated promptly. Although symptoms can become life-threatening, partial recovery is possible from even the most severe cases of GBS.
Can GBS cause weakness?
The first symptom includes weakness or tingling sensations in the legs. This sometimes spreads to the arms and upper body. A neurological exam usually reveals a loss of all deep tendon reflexes. The symptoms may get worse. In some cases, you may not be able to use your muscles at all. You become paralyzed, and breathing is hard. Your blood pressure and heart function are affected. GBS is a medical emergency and needs to be treated promptly.
What causes GBS?
GBS can occur after a viral infection, surgery, injury, or a reaction to an immunization.
How to prevent group B strep?
The two best ways to prevent group B strep (GBS) disease during the first week of a newborn’s life are: 1 Testing pregnant women for GBS bacteria 2 Giving antibiotics, during labor, to women at increased risk
Do babies born to women who tested positive for GBS need antibiotics?
Most babies born to women who tested positive for GBS bacteria do not need treatment if their mother received antibiotics during labor.
Can antibiotics help with GBS?
Antibiotics are very effective at preventing GBS disease in newborns. Consider the following examples:
Can you test positive for GBS during pregnancy?
GBS bacteria come and go naturally in people’s bodies. A woman may test positive for the bacteria at some times and not others. That is why doctors test women late in their pregnancy, close to the time of delivery.
Does Emma have a chance of developing GBS?
Tested positive for GBS bacteria. Did not get antibiotics during labor. Her baby has a 1 in 200 chance of developing GBS disease. Emma’s baby is 20 times more likely to get GBS disease compared to Tanya’s baby.
What is the diagnosis of GBS?
The diagnosis of GBS is based on the prodromal infections, symptoms, and signs combined with laboratory workups including electrophysiological studies and CSF/serum tests. Pharmacological treatments should be applied immediately in progressive GBS patients who cannot walk without aid. Decision-making as to ICU admission should be based on EGRIS, respiratory function, and extent of dysautonomia/dysphagia. The ICU monitoring of physiological parameters facilitates the recognition of GBS progression and the decision-making process for neurointensivists. *EGRIS is calculated viaintegrating MRC scores, facial/bulbar weakness, and duration from the onset to admission. **IVIg at 2g/kg BW can even be completed within 2 or 1 day in heathy cohorts, especially for young patients with normal cardiac and renal functions. Abbreviations: ANA, antinuclear antibody; BW, body weight; CK, creatine kinase; CSF, cerebrospinal fluid; EGRIS, Erasmus GBS respiratory insufficiency score; GBS, Guillain–Barré syndrome; ICU, intensive care unit; IVIg, intravenous immunoglobulin; LDH, lactate dehydrogenase; MRC, Medical Research Council; PE, plasma exchange.
Why are GBS patients more susceptible to pressure palsies?
Patients with severe GBS are particularly susceptible to pressure palsies for two reasons: (a) loss of functional position in GBS patients leads to an imbalance between flexor and extensor muscles and (b) inflamed nerves are susceptible to pressure injury (Chalela, 2001).
Does IVIG inhibit Fc-mediated activation?
IVIg has pleiotropic immunomodulatory effects, which include inhibiting Fc-mediated activation of macrophages, preventing the binding of antibodies to neural targets, and preventing complement activation which would otherwise trigger further nerve damage (Verboon et al., 2017).
How long does aor 1 g/kg BW last?
aOr 1 g/kg BW for 2 days or 2 g/kg BW for 1 day
Is GBS a heterogeneous disease?
As the incidence of GBS is low and the disease is clinically heterogeneous, most of the documented investigations have a relatively small sample size. In contrast with immunotherapies, care and treatment of GBS in the ICU setting are largely empirical. As a consequence, observational data are occasionally used to guide clinical practice.
Do GBS patients need MV?
Up to 30% of GBS patients require MV as well as ICU admission (Yuki and Hartung, 2012; Van Den Berg et al., 2018). Whenever feasible, rapidly progressing patients who are unable to walk without aid, are bedbound, or have labile blood pressure, cardiac arrhythmia, or respiratory distress should be treated immediately, preferably in an ICU (Harms, 2011; Verboon et al., 2017). Failure to refer severely affected patients to a specialized neurological ICU may lead to higher mortality rates, implicating the importance of earlier referral of severe cases and providing neurocritical care (Taylor et al., 2017). A multidisciplinary team is encouraged to provide supportive care for severe GBS cases in the ICU to avoid multiple comorbidities.
Is GBS a reflex?
Hypoactive or absent deep tendon reflexes are a common clinical feature of GBS, although increased or normal tendon reflexes can be seen in about 10% of patients during the early phase of the disease (Yuki, 2012; Leonhard et al., 2019).