Mayoclinic.org
Jun 14, 2021 · Now, primary treatments for gestational hypertension include medications and prenatal monitoring. Medications Drug therapy is an effective, proven way to moderate blood pressure during pregnancy, though care must be used in selecting and administering drugs.
Top10homeremedies.com
Background: Hydralazine, labetalol, and nifedipine are the recommended first-line treatments for severe hypertension in pregnancy. While all three are effective, there is a lack of sufficient evidence regarding their comparative safety and efficacy.
Medicalnewstoday.com
Drug treatment of hypertension in pregnancy According to NHBPEP methyldopa, labetalol, beta blockers (other than atenolol), slow release nifedipine, and a diuretic in pre-existing hypertension are considered as appropriate treatment [ 1 ].
What is the best first-line treatment for severe hypertension in pregnancy?
Apr 10, 2019 · oral labetalol is considered a first-line agent for non-severe hypertension in pregnancy 3 – 7, 9, 10 and is in fact the only first-line agent recommended by the british guidelines. 10 in a prospective observational study, approximately 75% of women responded to oral labetalol as monotherapy. 87 earlier randomized trials directly comparing it to …
What do you need to know about gestational hypertension?
Treatment for gestational hypertension may include: Bedrest, either at home or in the hospital, may be recommended; Hospitalization (as specialized personnel and equipment may be necessary) Magnesium sulfate (or other antihypertensive medications for gestational hypertension if blood pressure readings are in the severe range)
What is the role of antihypertensive drugs during pregnancy?
Gestational Hypertension also referred to as Pregnancy-Induced Hypertension (PIH) is a condition characterized by high blood pressure during pregnancy.. Gestational Hypertension can lead to a serious condition called Preeclampsia, also referred to as Toxemia.Hypertension during pregnancy affects about 6-8% of pregnant women.. The different types of hypertension during …
What is the first line treatment for preeclampsia?
Objectives: To quantify the mortality and morbidity effects from different first-line antihypertensive drug classes: thiazides (low-dose and high-dose), beta-blockers, calcium channel blockers, ACE inhibitors, angiotensin II receptor blockers (ARB), and alpha-blockers, compared to placebo or no treatment.Secondary objectives: when different antihypertensive drug classes …
What is the first line medication for gestational HTN?
Background: Hydralazine, labetalol, and nifedipine are the recommended first-line treatments for severe hypertension in pregnancy.
What is the treatment for gestational hypertension?
If you have mild hypertension and your baby is not fully developed, your doctor will probably recommend the following: Rest, lying on your left side to take the weight of the baby off your major blood vessels. Increase prenatal checkups. Consume less salt.
What is the drug of choice for hypertension in pregnancy?
Methyldopa is a drug of first choice for control of mild to moderate hypertension in pregnancy and is the most widely prescribed antihypertensive for this indication in several countries, including the US and the UK.
Why is hydralazine given during pregnancy?
Hydralazine is used to treat high blood pressure (hypertension). It is also used to control high blood pressure in a mother during pregnancy (pre-eclampsia or eclampsia) or in emergency situations when blood pressure is extremely high (hypertensive crisis).Feb 1, 2022
Why is magnesium sulfate given in pregnancy?
Magnesium sulfate is approved to prevent seizures in preeclampsia, a condition in which the pregnant woman develops high blood pressure and protein in the urine, and for control of seizures in eclampsia. Both preeclampsia and eclampsia are life-threatening complications that can occur during pregnancy.May 30, 2013
Is labetalol safe in first trimester?
Blood pressure control is more frequently achieved in hypertensive pregnancies with labetalol than with methyldopa as a first line treatment. Labetalol is safe to the fetus and newborn and might offer a better prevention of intrauterine death than methyldopa.
What is the best medication for hypertension during pregnancy?
Drug treatment of hypertension in pregnancy. According to NHBPEP methyldopa, labetalol, beta blockers (other than atenolol), slow release nifedipine, and a diuretic in pre-existing hypertension are considered as appropriate treatment [1].
What is the best way to measure BP?
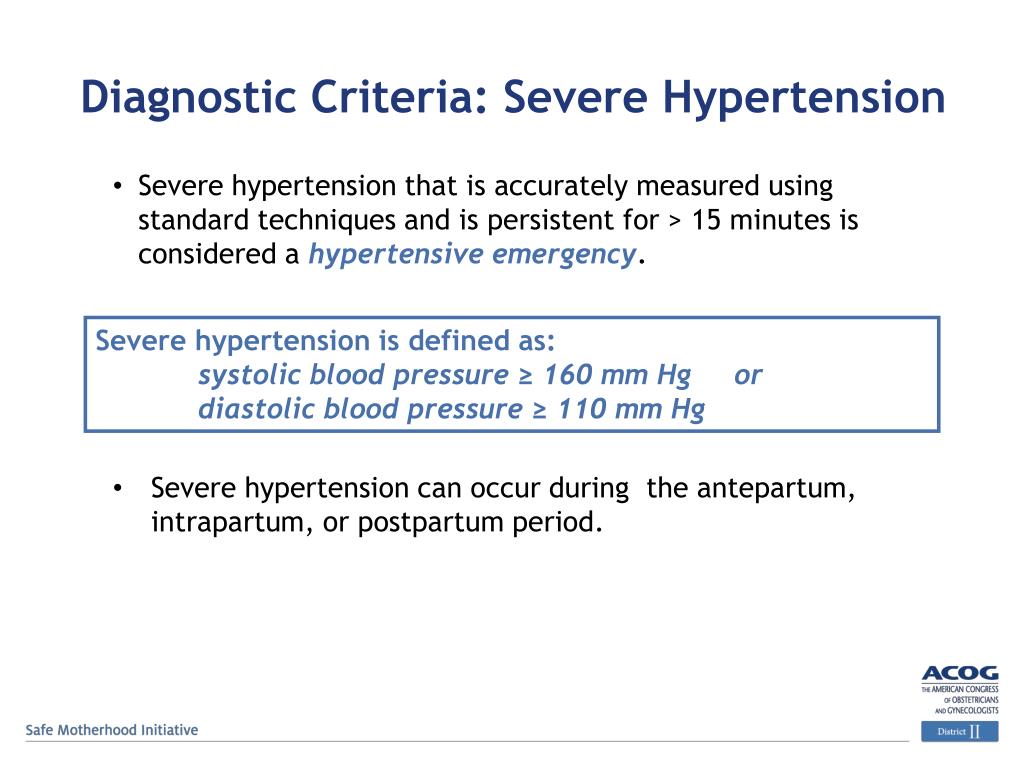
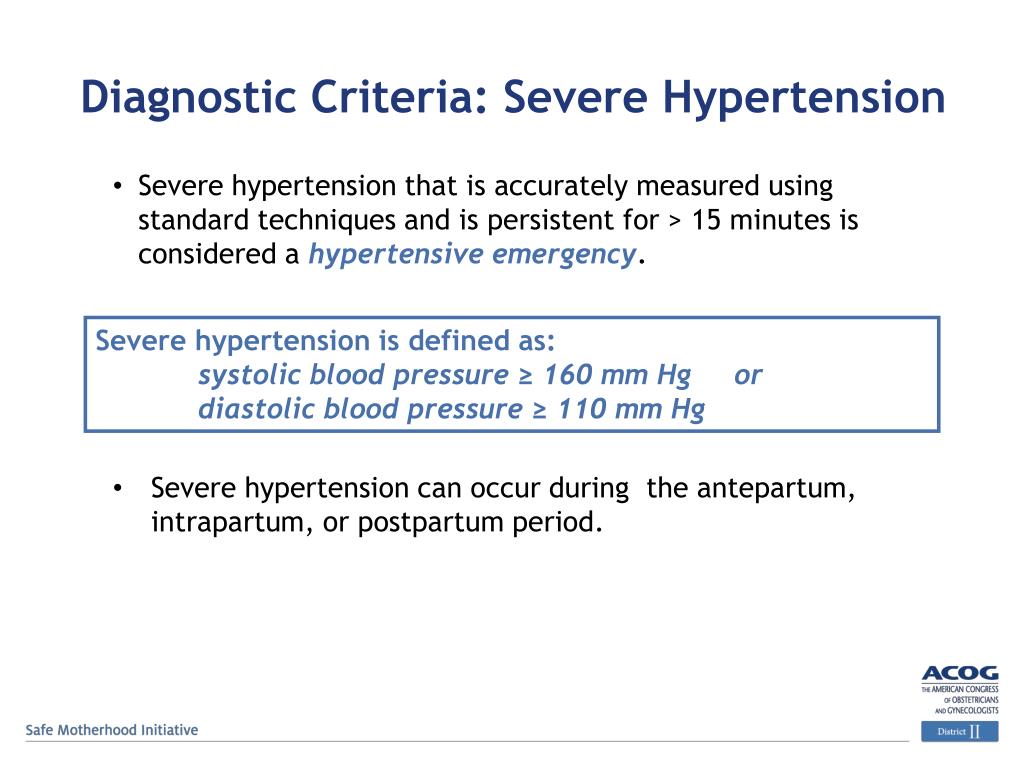
BP can be measured using a mercury sphygmomanometer, calibrated aneroid device, or an automated BP device (valida ted for use in preeclampsia). (II-2A) Automated BP machines may underestimate BP in women with preeclampsia, and comparison of readings using mercury sphygmomanometry or an aneroid device is recommended.
What is the most common medical condition during pregnancy?
Similar to the non-pregnant population, hypertension is the most common medical disorder encountered during pregnancy and is estimated to occur in about 6–8% of pregnancies [1]. A recent report highlighted hypertensive disorders as one of the major causes of pregnancy-related maternal deaths in the United States, ...
Is blood pressure higher during pregnancy?
Blood pressure levels requiring therapy in pregnancy, although somewhat different among various groups and professional societies, have been set, in general , at higher systolic and diastolic levels compared to the general population [12].
Can preeclampsia be superimposed?
Preeclampsia can also occur superimposed upon chronic hypertension. Gestational hypertension is defined as new onset BP ≥140 mmHg systolic or 90 mmHg diastolic on at least two occasions, at least 6 h apart, after 20 weeks gestation, in the absence of proteinuria.
Is methyldopa safe for pregnancy?
Methyldopa has a long history of use in pregnancy and does not appear teratogenic [27]. Methyldopa has a record of safety in pregnancy, as established by follow-up studies in the 1980’s of children exposed to the drug in utero [31].
Does magnesium sulphate reduce maternal mortality?
In a Cochrane review of treatment of women with preeclampsia, magnesium sulphate more than halves the risk of eclampsia, and probably reduces maternal death [48]. In women with eclampsia, magnesium sulphate reduces the risk ratio of maternal death and of recurrence of seizures, compared with diazepam.
Why is early detection of gestational hypertension important?
Early identification of women at risk for gestational hypertension may help prevent some complications of the disease. Education about the warning symptoms is also important because early recognition may help women receive treatment and prevent worsening of the disease.
What causes gestational hypertension?
Some conditions may increase the risk of developing the condition, including the following: Pre-existing hypertension (high blood pressure) Kidney disease. Diabetes. Hypertension with a previous pregnancy. Mother's age younger than 20 or older than 40.
What is the most common type of hypertension in pregnancy?
Gestational hypertension is a form of high blood pressure in pregnancy. It occurs in about 6 percent of all pregnancies. Another type of high blood pressure is chronic hypertension--high blood pressure that is present before pregnancy begins. Gestational hypertension can develop into preeclampsia. This condition occurs often in young women ...
How do you know if you have a swollen stomach?
Symptoms may include: Increased blood pressure. Absence or presence of protein in the urine (to diagnose gestational hypertension or preeclampsia) Edema (swelling) Sudden weight gain. Visual changes such as blurred or double vision. Nausea, vomiting. Right-sided upper abdominal pain or pain around the stomach.
When should a baby be delivered?
Because of these risks, it may be necessary for the baby to be delivered early, before 37 weeks gestation.
What is the difference between eclampsia and eclampsia?
Preeclampsia is diagnosed when a woman with gestational hypertension also has increased protein in her urine. Eclampsia is a severe form of preeclampsia. Women with eclampsia have seizures resulting from the condition. Eclampsia occurs in about one in 1,600 pregnancies and develops near the end of pregnancy, in most cases.
Can high blood pressure cause pregnancy?
The following are the most common symptoms of high blood pressure in pregnancy. However, each woman may experience symptoms differently, and a patient with gestational hypertension may be completely asymptomatic. Symptoms may include: Increased blood pressure.
How to prevent gestational hypertension?
Some ways you can help prevent gestational hypertension include the following: Use salt as needed for taste. Drink at least 8 glasses of water a day. Increase the amount of protein you take in, and decrease the number of fried foods and junk food you eat. Get enough rest.
What is a pregnancy induced hypertension?
Gestational Hypertension also referred to as Pregnancy-Induced Hypertension (PIH) is a condition characterized by high blood pressure during pregnancy. Gestational Hypertension can lead to a serious condition called Preeclampsia, also referred to as Toxemia.
How long does it take for blood pressure to rise during pregnancy?
Chronic Hypertension – Women who have high blood pressure (over 140/90) before pregnancy, early in pregnancy (before 20 weeks), or continue to have it after delivery. Gestational Hypertension– High blood pressure that develops after week 20 in pregnancy ...
Can hypertension cause low birth weight?
Hypertension can prevent the placenta from getting enough blood. If the placenta doesn’t get enough blood, your baby gets less oxygen and food. This can result in low birth weight. Most women still can deliver a healthy baby if hypertension is detected and treated early.
What percentage of pregnant women have gestational hypertension?
Gestational hypertension occurs in ≈6% of pregnancies and is hypertension developing in the latter half of pregnancy not associated with the systemic features of preeclampsia (eg, proteinuria).
What is the classification of antihypertensive drugs?
Most antihypertensive agents used in pregnancy are designated as “category C,” which states that human studies are lacking, animal studies are either positive for fetal risk or are lacking, and the drug should be given only if potential benefits justify potential risks to the fetus. 25 This category cannot be interpreted as no evidence of risk and is so broad to preclude usefulness in practice, leading some groups to suggest that the Food and Drug Administration classification be abandoned. 26,27 Information is, thus, based on clinical cases, small studies, and meta-analyses.
How long does it take for preeclampsia to manifest?
Preeclampsia-eclampsia is a syndrome that manifests clinically as new-onset hypertension in later pregnancy (any time after 20 weeks, but usually closer to term), with associated proteinuria: 1+ on dipstick and, officially, ≥300 mg per 24-hour urine collection.
Where is Tiina Podymow?
Tiina Podymow From the Division of Nephrology (T.P.), McGill University Health Center, Royal Victoria Hospital, Montreal, Quebec, Canada; and the Division of Nephrology and Hypertension (P.A.), Weill Medical College of Cornell University, New York, NY.
Is methyldopa safe for pregnancy?
Methyldopa remains one of the most widely used drugs for the treatment of hypertension in pregnancy. It is a centrally acting α 2 -adrenergic agonist prodrug, which is metabolized to α-methyl norepinephrine and then replaces norepinephrine in the neurosecretory vesicles of adrenergic nerve terminals. BP control is gradual, over 6 to 8 hours, because of the indirect mechanism of action. It is not thought to be teratogenic based on limited data and a 40-year history of use in pregnancy. It has been assessed in a number of prospective trials in pregnant women compared with placebo 28–30 or with alternative antihypertensive agents. 30–33 Treatment with methyldopa has been reported to prevent subsequent progression to severe hypertension in pregnancy 34 and does not seem to have adverse effects on uteroplacental or fetal hemodynamics 35 or on fetal well being. 29 One placebo-controlled trial (>200 women with diastolic BP >90 mm Hg at entry) noted fewer midpregnancy losses in patients randomly assigned to methyldopa, 28 but this observation was not confirmed in a more recent trial of a similar size. 29 Importantly, birth weight, neonatal complications, and development during the first year were similar in children exposed to methyldopa as in the placebo group. 36,37 In a follow-up study of offspring who were exposed to methyldopa in utero, at 7.5 years of age, the children exhibited intelligence and neurocognitive development similar to control subjects. 38
Can a blocker be used in pregnancy?
β-Blockers have been used extensively in pregnancy. Although several randomized trials comparing β-blockers with either placebo or other agents have been conducted, 31,32,42,43 there are still some unresolved issues regarding their use in pregnancy, largely a result of a few small studies that suggest an association with lower birth weight infants. None of the β-blockers have been associated with teratogenicity. In meta-analysis and Cochrane review, 44 individual agents were not distinguishable in their perinatal effects with the exception of atenolol, which in 1 small study was started at 12 to 24 weeks’ gestation and resulted in clinically significant fetal growth restriction and decreased placental weight compared with placebo. 45 This observation was supported in a subsequent retrospective review comparing atenolol with alternative therapies. 46 Given differences in β-blockers with respect to lipid solubility and receptor specificity, the potential for clinically relevant differences between agents exists but has not been investigated in pregnancy. Oral β-blockade had been associated with nonclinically significant neonatal bradycardia, 14,47 although in a systematic review of trials, labetalol does not (along with oral methyldopa, nifedipine, or hydralazine) seem to cause neonatal heart rate effects. 48 Parenteral therapy has been found to increase the risk of neonatal bradycardia, requiring intervention in 1 of 6 newborns. 14 Further reassurance is derived from a 1-year postpartum follow-up study, which showed normal development of infants exposed to atenolol in utero. 49 Maternal outcomes are improved with the use of β-blockers, with effective control of maternal BP, decreased incidence of severe hypertension, and decreased rate of preterm admission to hospital 14; they have been found in a recent Cochrane analysis to be more effective in lowering BP compared with methyldopa in 10 trials. 5
Can diuretics be used during pregnancy?
Diuretics are commonly prescribed in essential hypertension before conception and, given their apparent safety, the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy concluded that they may be continued through gestation (with an attempt made to lower the dose) or used in combination with other agents, especially for women deemed likely to have salt-sensitive hypertension. 1 Older anecdotal studies suggested that diuretics might prevent preeclampsia, a finding that was supported by a meta-analysis (published in 1985) of 9 randomized trials involving >7000 subjects. 74 Although volume contraction might be expected to limit fetal growth, outcome data have not supported these concerns. 74 However, mild volume contraction with diuretic therapy may lead to hyperuricemia and in so doing invalidate serum uric acid levels as a laboratory marker in the diagnosis of superimposed preeclampsia.
Can beta blockers be used for hypertension?
Current evidence does not support the use of beta blockers, particularly atenolol, as first-line treatment for hypertension. Although there is increasing evidence that ACE inhibitors and possibly CCBs may be equivalent to thiazide diuretics in reducing morbidity and mortality, the relative expense of these medications makes thiazide diuretics ...
Is thiazide a first line treatment?
The strongest body of evidence indicates that for most patients with hypertension, thiazide diuretics are the best proven first-line treatment in reducing morbidity and mortality. They are particularly effective in the secondary prevention of cardiovascular events in all patients with hypertension, and in the primary prevention ...
Is ACE inhibitor a low dose?
First-line high-dose thiazides and beta blockers are inferior to first-line low-dose thiazides. These summaries have been derived from Cochrane reviews published in the Cochrane Database of Systematic Reviews in the Cochrane Library.
Do beta blockers reduce mortality?
Beta blockers and CCBs were also no different from placebo in reducing mortality risk. Thiazide diuretics and ACE inhibitors reduced total mortality risk significantly, but this risk reduction was smaller than that of cardiovascular events and stroke. 1.
Is thiazide a beta blocker?
Current evidence does not support using beta blockers as first-line therapy for hypertension.
