Medication
What is the first-line treatment for C. diff? Antibiotics are the first-line treatment for a Clostridium difficile infection. Healthcare providers have only a limited arsenal of antibiotics they can use, starting with vancomycin or fidaxomicin. In some cases, however, the colon muscles stop working, and oral or rectal antibiotics become useless.
Procedures
Vancomycin and metronidazole are currently used as a standard therapy for CDI. Metronidazole is recommended as a first-line therapy for mild-to-moderate i … Clostridium difficile infection (CDI) represents one of the most serious nosocomial infections that have grown dramatically over the past decade.
Self-care
Antimicrobial treatment suggested for recurrent Clostridioides difficile infection (CDI) in the paediatric population. Abbreviations: IV, intravenous; PO, oral; PR, rectal; qid, 4 times daily; tid, 3 times daily. Adapted from McDonald et al. [ 19 ].
Nutrition
1.1.14 Refer people in the community with suspected or confirmed C. difficile infection to hospital if they are severely unwell, or their symptoms or signs worsen rapidly or significantly at any time. Refer urgently if the person has a life-threatening infection.
What is the first-line treatment for Clostridium diff?
Is metronidazole a first-line therapy for Clostridium difficile infection?
How is recurrent Clostridioides difficile infection (CDI) treated in the US?
When to refer a patient with Clostridium difficile to hospital?
What is the best treatment for Clostridium difficile?
Vancomycin and fidaxomicin are the most effective antibiotics against Clostridium difficile infections. They are both equally effective at wiping out an initial infection. However, patients treated with fidaxomicin have a lower rate of a recurrent C.
Which of the following are recommended first line options for C difficile infection?
Treatment Recommendations for Clostridioides difficile Infection in AdultsEpisodeTreatment regimenInitial infectionIf neither agent is available: metronidazole, 500 mg orally 3 times per day for 10 daysSevereVancomycin, 125 mg orally 4 times per day for 10 daysor19 more rows•Feb 1, 2020
What is the recommended treatment for Clostridium difficile colitis?
Antibiotic treatment is recommended for all except very mild cases actually triggered by antibiotic use; suitable treatments include metronidazole, vancomycin, and fidaxomicin. For mild/moderate disease, oral metronidazole (500 mg 3 times daily for 10 days) is recommended as the initial treatment.
What antibiotics treat Clostridium?
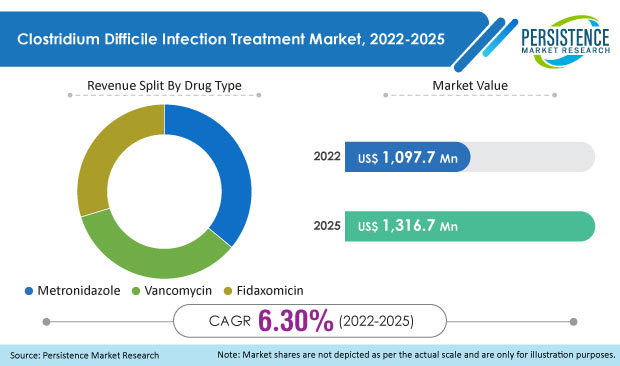
Three antibiotics are commonly used for the treatment of CDI: metronidazole (11), vancomycin (12), and fidaxomicin (13). Of these, fidaxomicin and its major active metabolite (OP-1118) have the narrowest reported spectrum of antibacterial activity (14).
Why is oral vancomycin given for C. diff and not IV?
Vancomycin, rifaximin, and fidaxomicin are useful in recurrent or persistent cases. The oral administration of these medications is the preferred route, because C difficile remains within the colonic lumen without invading the colonic mucosa.
Why is metronidazole not recommended for C. diff?
It is important to note that metronidazole is still recommended for the treatment of CDI in children according to the 2017 IDSA/SHEA guidelines. Keep in mind that prolonged or repeated courses of metronidazole increase the risk of neurotoxicity.
Can you take Flagyl and vancomycin together?
Interactions between your drugs No interactions were found between Flagyl and vancomycin. However, this does not necessarily mean no interactions exist. Always consult your healthcare provider.
Is fidaxomicin better than vancomycin?
According to the study, fidaxomicin was evaluated in almost 900 patients in six randomized controlled trials. In achieving a sustained cure, the researchers found that fidaxomicin was significantly better than vancomycin, metronidazole, bacitracin and tolevamer.
Why is vancomycin used for C diff?
C diff is a type of bacteria that causes severe diarrhea. Oral vancomycin is also used to treat enterocolitis caused by a certain bacteria (eg, Staphylococcus aureus). Vancomycin belongs to the family of medicines called antibiotics. It works by killing bacteria or preventing their growth.
What antibiotic is C. diff resistant to?
C. difficile is known to be resistant to multiple antibiotics, such as aminoglycosides, lincomycin, tetracyclines, erythromycin, clindamycin, penicillins, cephalosporins, and fluoroquinolones, which are commonly used in the treatment of bacterial infections in clinical settings (15, 16).
Does azithromycin treat C. diff?
Conclusions: It can be concluded from these data that, in Turkey, C. difficile is responsible for 20% of antibiotic-associated diarrheas. Lincomycin, Azithromycin and Ampicillin were most often associated with the development of antibiotic-associated diarrhea. Ornidazole and Vancomycin were effective agents for C.
Why is C. diff treated with antibiotics?
When you take antibiotics to treat an infection, these drugs tend to destroy some of the helpful bacteria in your body in addition to the bacteria causing the infection. Without enough helpful bacteria to keep it in check, C. difficile can quickly grow out of control.
What is the best treatment for C. difficile?
difficile is another antibiotic. These antibiotics keep C. difficile from growing, which in turn treats diarrhea and other complications. Your doctor may prescribe vancomycin ( Vancocin HCL, Firvanq) or fidaxomicin (Dificid).
What age can you take antibiotics for C difficile?
Are older than 65. Are taking other antibiotics for a different condition while being treated with antibiotics for C. difficile infection. Have a severe underlying medical disorder, such as chronic kidney failure, inflammatory bowel disease or chronic liver disease. Treatment for recurrent disease may include:
What test can detect C difficile toxin B?
Several main types of lab tests exist, and they include: Polymerase chain reaction. This sensitive molecular test can rapidly detect the C. difficile toxin B gene in a stool sample and is highly accurate. GDH/EIA. Some hospitals use a glutamate dehydrogenase (GDH) test in conjunction with an enzyme immunoassay (EIA) test.
What is the test for C difficile?
difficile infection and look for alternative causes of your symptoms, your doctor may examine the inside of your colon. This test (flexible sigmoidoscopy or colonoscopy) involves inserting a flexible tube with a small camera on one end into your colon to look for areas ...
How long does it take to get cytotoxicity test results?
This type of test is sensitive, but it is less widely available, is more cumbersome to do and requires 24 to 48 hours for test results. It's typically used in research settings.
What is the procedure to check for C. difficile?
If your doctor is concerned about possible complications of C. difficile, he or she may order an abdominal X-ray or a computerized tomography (CT) scan, which provides images of your colon. The scan can detect the presence of complications such as thickening of the colon wall, expansion of the bowel or, more rarely, a hole (perforation) in the lining of your colon.
Can probiotics help with C. difficile?
Research hasn't consistently shown that currently available products are helpful in preventing or treating infection with C. difficile. Advanced probiotics are currently being studied for their potential use in C. difficile treatment or prevention but aren't currently available.
Why is it important to have a pharmacist on CDI?
Because the recommendations in these guidelines differ notably from previous versions, pharmacists can play an important role in ensuring the optimal treatment approach for patients with CDI , particularly when it appears that a patient may be being treated for CDI according to outdated guidelines. References. 1.
Is metronidazole a first line drug?
For the first time in almost 3 decades, metronidazole is no longer recommended as first-line therapy in adults.
Can you use antimotility for CDAD?
In all patients with CDAD, inciting antibiotics should be discontinued, if possible, or changed to a regimen with a narrower spectrum. Antimotility agents should not be used, even in mild cases. Table 1. Guidelines for Treatment of Mild, Severe, and Complicated Clostridium difficile–associated Disease (CDAD) Criteria.
Is metronidazole a monotherapy?
The efficacy of IV metronidazole has not been definitively demonstrated, but at least one retrospective study examined its use as monotherapy in 10 patients with CDAD.17A majority of these patients experienced resolution, and none developed fulminant colitis or toxicity such as peripheral neuropathy.
Is metronidazole a first line treatment for C difficile?
difficileinfection. In mild-to-moderate cases, oral metronidazole remains adequate first-line therapy, but in the absence of a good clinical response, switching to vancomycin may be necessary.
How long does it take for Clostridium difficile to clear up?
A mild or moderate Clostridium difficile infection typically takes 10 to 14 days of antibiotic treatment to clear up. Depending on the antibiotic used to treat the initial infection, about 15% to 25% of patients will develop a second C. diff infection about two weeks after the first one clears up.
How long does it take for a C. difficile infection to progress?
In some cases, the infection can progress rapidly in a few hours or a couple of weeks after the initial symptoms into a life-threatening illness called fulminant CDI. The C. difficile poisons cause the colon to swell to massive proportions—a condition called toxic megacolon.
What is the toxins in Clostridium difficile?
Clostridium difficile produces two potent toxins that create many of the symptoms of Clostridium difficile colitis: toxin A and toxin B. Toxin A causes swelling of the intestinal tissues, and toxin B kills cells in the colon. A new, more deadly strain of C. difficile appeared in the United States and Canada in the 1990s.
How many C. difficile infections are community acquired?
difficile infections. About 3 out of 5 C. difficile infections happen in hospitals, long-term care facilities, or other healthcare facilities. However, 2 out of 5 C. difficile infections are community-acquired.
What is C diff?
Clostridium difficile (C. difficile, or C. diff) is a common and usually harmless bacterial infection of the large intestine. It often produces no symptoms or a little bit of watery diarrhea.
Why is C diff isolated?
In a hospital, patients with C. diff infections are usually isolated to prevent infecting others. For mild or moderate cases of Clostridium infection treated at home, infection control and contact precautions are paramount:
Where does Clostridium difficile live?
Clostridium difficile lives inside the large intestine. While it usually is a common and harmless bacteria, antibiotic use can jump-start a C. difficile infection that may rapidly progress to a severe and even life-threatening medical illness called pseudomembranous colitis.
Recommendations (Abridged)
I. In Patients With an Initial CDI episode, Should Fidaxomicin Be Used Rather Than Vancomycin?
Methodology
Clinical Practice Guidelines are statements that include recommendations intended to optimize patient care by assisting practitioners and patients in making shared decisions about appropriate healthcare for specific clinical circumstances.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
1.1 Managing suspected or confirmed Clostridioides difficile infection
1.1.1 For people with suspected or confirmed C. difficile infection, see Public Health England's guidance on diagnosis and reporting.
1.2 Choice of antibiotic
1.2.1 When prescribing antibiotics for suspected or confirmed C. difficile infection in adults, follow table 1.