How do you know if you have MRSA in your urine?
You may notice a range of symptoms before a doctor finds MRSA in urine or on your skin. If you see any of these symptoms occur in yourself or a loved one, contact a doctor immediately. MRSA infections may cause you to experience a fever. For skin infections, MRSA symptoms first appear as swollen or painful red bumps.
How to treat a MRSA infection naturally?
How to Treat a MRSA Infection Naturally
- Warm Compresses. To treat the swollen, red, painful bumps on the skin caused by a CA-MRSA infection, it is important to apply a warm compress on the affected area.
- Turmeric. A natural spice, turmeric is an effective home treatment for a CA-MRSA infection. ...
- Aloe Vera. ...
- Garlic. ...
- Manuka Honey. ...
- Oil of Oregano. ...
- Colloidal Silver. ...
- Tea Tree Oil. ...
- Indian Lilac. ...
Does clindamycin cover MRSA?
Clindamycin is widely used in children for community-acquired MRSA skin and soft-tissue infections, and is anecdotally reported to be effective.
What antibiotic is used for MRSA?
Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterial infection that has become resistant to most of the antibiotics used to treat regular staph infections. Duke University computer ...
How long do you take antibiotics for MRSA?
Typically, you can expect treatment to last for 7 to 14 days, although you may notice it clear up before you finish your antibiotic treatment. It's critical to complete your entire course of prescribed antibiotics.
How long is MRSA suppression treatment usually given for?
The treatment is a combination of two separate treatments to be used over a 5 day period. It is important that you complete the 5 day course to reduce the possibility of developing a MRSA infection. Both treatments should be started on the same day.
How many days does the MRSA Decolonisation treatment consist of?
Decolonisation is when topical treatments are used to try and get rid of methicillin resistant staphylococcus aureus (MRSA). It involves the use of an antiseptic body wash and nasal ointment for 5 days. Decolonisation treatment can reduce the risk of recurrent MRSA infections or spreading MRSA to others.
How long is a course of antibiotics for staph infection?
Practice guidelines recommend at least 14 days of antibiotic therapy for uncomplicated Staphylococcus aureus bacteremia (SAB).
What is the best antibiotic for MRSA?
Vancomycin is generally considered the drug of choice for severe CA-MRSA infections. Although MRSA is usually sensitive to vancomycin, strains with intermediate susceptibility, or, more rarely, resistant strains have been reported.
How often should MRSA positive patients be screened?
Patients who have prolonged admissions (e.g. for several weeks or longer) but who are MRSA negative on admission are at higher risk of acquisition of MRSA and must therefore be screened on a weekly basis. During topical eradication regimen and for 2 days after.
How long do you need to leave to MRSA screen the patient after they have completed MRSA suppression therapy?
Begin at least 48 hrs after end of antiseptic and antibiotic therapy. If decolonisation fails, seek advice from the Infection Control Team. What do I do if a patient is discharged from hospital MRSA positive?
How do you clear colonization of MRSA?
Because MRSA carriage is most common in the nares and on the skin (particularly in sites such as the axilla and groin), MRSA decolonization therapy typically includes intranasal application of an antibiotic or antiseptic, such as mupirocin or povidone-iodine, and topical application of an antiseptic, such as ...
Do patients with MRSA need to be isolated?
Since MRSA and/or VRE patients require isolation and can only be paired with patients of like infection, this is a perfect environment for testing. Starting in May 2016, the hospital discontinued contact precautions for patients with endemic MRSA and VRE colonization, coupled with an education initiative.
Is 7 days of antibiotics enough for staph infection?
Background. Staphylococcus aureus bacteremia (SAB) is frequently encountered in the hospital setting, and current guidelines recommend at least 14 days of antibiotic treatment for SAB in order to minimize risks of secondary deep infections and relapse.
How long does doxycycline take to work for Staph?
Response and effectiveness. Doxycycline is almost completely absorbed after oral administration. Peak concentrations are reached within two to three hours after dosing; however, it may take up to 48 hours before infection-related symptoms start to abate.
What is the first line treatment for MRSA?
Vancomycin remains the initial antibiotic of choice for the treatment of patients with MRSA bacteremia and endocarditis due to isolates with vancomycin MIC≤2 μg/mL.
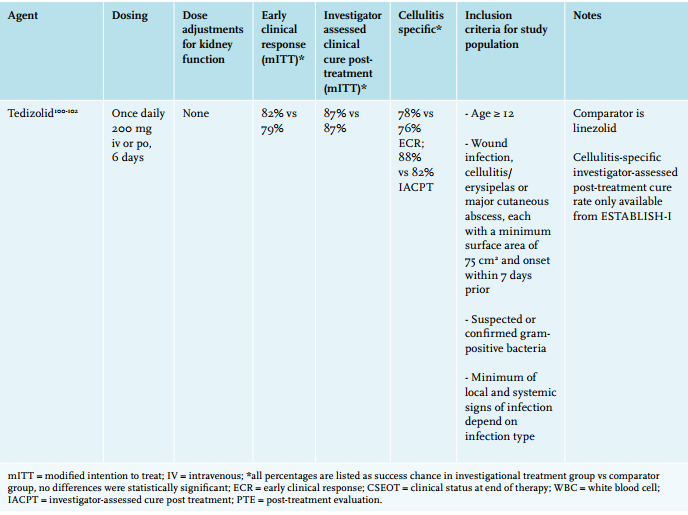
Linezolid (Brand Names: Zyvox, Zyvoxid Or Zyvoxam)
Approved for use in the year 2000, Linezolid is FDA approved for treating soft tissue and skin infections, including those caused by MRSA. It is of...
Mupirocin (Brand Name: Bactroban)
Commonly used as a topical cream for minor skin infections and skin lesions for Staph aureus, MRSA and Streptococcus infections. Mupirocin ointment...
Trimethoprim-Sulfamethoxazole (Brand Name: Septra Or Bactrim)
It is not FDA-approved for the treatment of Staphylococcal infections (including MRSA). However, laboratory tests have shown most CA-MRSA strains a...
Tetracyclines (Doxycycline and Minocycline)
Data suggests these drugs are effective in treatment of soft tissue and skin infections, but not for deeper or more severe infections. 1. Side Effe...
Intravenous (IV) Vancomycin
Vancomycin is often called an antibiotic of last resort for MRSA, though resistance against it has been growing. Vancomycin requires IV administrat...
Intravenous (IV) Daptomycin
Daptomycin is FDA approved for adults with Staph aureus bacteremia, some forms of endocarditis and some skin and soft tissue infections. The safety...
How to diagnose MRSA?
Doctors diagnose MRSA by checking a tissue sample or nasal secretions for signs of drug-resistant bacteria. The sample is sent to a lab where it's placed in a dish of nutrients that encourage bacterial growth. But because it takes about 48 hours for the bacteria to grow, newer tests that can detect staph DNA in a matter ...
What to expect from a doctor for a physical exam?
What to expect from your doctor. During your physical exam, your doctor will closely examine any skin cuts you may have. He or she might take a sample of tissue or liquid from the cuts for testing. By Mayo Clinic Staff.
What to write in a doctor's appointment?
Before your appointment, you might want to write a list that includes: 1 Detailed descriptions of your symptoms 2 Information about medical problems you've had 3 Information about the medical problems of your parents or siblings 4 All the medications and dietary supplements you take 5 Questions you want to ask the doctor
Can antibiotics help with MRSA?
Treatment. Both health care-associated and community-associated strains of MRSA still respond to certain antibiotics. Doctors may need to perform emergency surgery to drain large boils (abscesses), in addition to giving antibiotics. In some cases, antibiotics may not be necessary.
Do antibiotics help with boils?
In some cases, antibiotics may not be necessary. For example, doctors may drain a small, shallow boil (abscess) caused by MRSA rather than treat the infection with drugs.
What is the AUC of vancomycin?
The pharmacokinetic driver of efficacy of vancomycin in bacteremia due to S. aureusis area under the plasma concentration time curve (AUC) values and an AUC0-24hto MIC ratio of ≥400μg·h/mL has been suggested as the target value. The measured trough concentration of 15-20 mg/L alone as been used as a surrogate as it was thought to be predictive of AUC/MIC; recent evidence suggests this may be incorrect. Modeling studies have demonstrated that unadjusted extrapolation of AUC from serum trough concentrations underestimate AUC by up to 25% and that AUCs varied between patients with similar trough results by up to 30-fold [3]. The increased accuracy of AUC estimations from serum vancomycin concentrations by the addition of Bayesian analysis may allow more precise individualized dosing, especially for targeting treatment of infections due to MRSA with an MIC = 2 μg/mL.
What is the best treatment for MRSA?
Vancomycin or daptomycin are the agents of choice for treatment of invasive MRSA infections [1]. Alternative agents that may be used for second-line or salvage therapy include telavancin, ceftaroline, and linezolid. Recent studies of treatment of MRSA bacteremia are reviewed. Vancomycin.
What is the fifth generation of cephalosporin?
Ceftaroline. Ceftaroline is a fifth-generation cephalosporin with bactericidal activity against MRSA and VISA as well as Gram-negative pathogens [14]. Ceftaroline fosamil, the pro-drug of ceftaroline, received approval by the US Food and Drug Administration (FDA) in 2010.
How long does telavancin last?
It is bactericidal against MRSA, vancomycin-intermediate S. aureus(VISA), and vancomycin-resistant S. aureus(VRSA). It has a half-life of seven to nine hours, permitting once daily dosing. Telavancin should be avoided in patients at risk for nephrotoxicity.
When was telavancin approved?
Telavancin was approved in November 2009 in the United States for the treatment of acute bacterial skin and skin structure infections (ABSSSI), and in June 2013 in US for hospital-acquired pneumonia (HAP) caused by gram-positive pathogens including MRSA where alternative treatments are not suitable.
What is the purpose of tigecycline?
Tigecycline’s distinctive feature is that it confers broad antibiotic coverage of drug-resistant Gram-positive bacteria and certain, but not all, species of multidrug-resistant Gram-negative bacteria, although it is a bacteriostatic agent.
Is teicoplanin a vancomycin?
Teicoplanin is a glycopeptides with slow bactericidal activity and a spectrum of activity and efficacy camparable to vancomycin. Some use it as the drug of choice for initial therapy of MRSA bacteremia, although good evidence to support this practice is lacking, while others favor its use for patients with intolerance to vancomycin [5]. Much debate has surrounded this antibiotic, however due to data showing inferior efficacy compared with vancomycin. These results can be explained by inadequate dosing of teicoplanin secondary to greater protein binding compared with vancomycin. Recent data and meta-analysis suggest that teicoplanin may not be inferior to vancomycin [6]. One meta-analysis noted a lower risk of nephrotoxicity with teicoplanin than with vancomycin [5].
What are the symptoms of MRSA?
Symptoms include a cough, sore throat, head ache, shortness of breath, fever and chills. In the retrospective study, researchers evaluated the medical charts of 115 patients hospitalized with MRSA pneumonia. Patients received either vancomycin or linezolid, ...
How long does it take to cure MRSA?
The national practice guideline for treating MRSA-related pneumonia is seven to 21 days. A Henry Ford Hospital study found that effective treatment can be done in half the time. Researchers found that 40 percent of patients were treated for eight to 13 days on a therapy of the antibiotics vancomycin or linezolid, and had the highest survival rate.
What was the Henry Ford study?
The Henry Ford study is believed to be the first to evaluate the length of treatment for MRSA-related pneumonia. The study was presented last week at the IDWeek meeting in San Diego.
What are common side effects of MRSA medication?
Stomach upset, nausea, and diarrhea can occur when taking antibiotics, especially when they are taken on an empty stomach. Some antibiotics used for MRSA treatment can have side effects such as itching, headache, rash, joint pain, and a metallic taste in the mouth. These side effects are not as common but can still occur. If you notice any serious side effects you should contact your doctor immediately. These are not all of the possible side effects of MRSA medications.
What are the best home remedies for MRSA?
The use of antibiotics coupled with different at-home treatments may help you recover more quickly from MRSA. You can also use this section to help to prevent MRSA or reduce the chance of sharing it with someone else.
What to do if you have an abscess?
If you have an abscess (a swollen area containing pus), draining the pus and taking oral antibiotics may be the first line of treatment—especially if the infected area is small and the condition appears mild. If you have a serious infection, or if MRSA gets into your bloodstream, then you may need intravenous antibiotics. "The approach to treatment is entirely dependent on the location of the infection and its severity," explains Dr. Adalja. "For example, a skin infection may require just a short course of oral antibiotics while a bloodstream infection may require weeks of intravenous antibiotics.”
What is the best treatment for MRSA?
Antibiotics. Depending on your specific antibiotic resistance with a MRSA infection, you may be given one or more antibiotic treatments to try. Antibiotics are the most commonly used and accepted form of treatment for MRSA patients because the condition is caused by bacteria.
What are the symptoms of MRSA?
You may notice a skin infection that resembles a spider bite, large pimple, or a red and painful bump.
What is the most common type of bacteria that is resistant to antibiotics?
Methicillin-resistant Staphylococcus aureus is a specific type of bacteria, also called staph, which can cause infection and has become resistant to common antibiotic treatments, such as methicillin. CDC.gov estimates that 5% of patients in United States hospitals are carriers for MRSA via their skin or nose.
How does MRSA spread?
The spread of MRSA in the general community is typically through the sharing of personal items such as razors, washcloths, towels, or other items that may have come into contact with the infected skin.
How long does it take for MRSA to develop?
It is important to discuss a follow-up plan with your patients in case they develop systemic symptoms or worsening local symptoms, or if symptoms do not improve within 48 hours.
What is the purpose of obtaining specimens for culture and susceptibility testing?
Obtaining specimens for culture and susceptibility testing is useful to guide therapy , particularly for those with more severe infections and those who fail to respond adequately to initial management.
Is incision and drainage the primary treatment for MRSA?
In the community, incision and drainage remains the primary therapy for these purulent skin infections. Empiric antibiotic coverage for MRSA may be warranted in addition to incision and drainage based on clinical assessment (e.g., presence of systemic symptoms, severe local symptoms, immune suppression, extremes of patient age, infections in a difficult to drain area, or lack of response to incision and drainage alone).
Is a spider bite a S. aureus infection?
A patient’s presenting complaint of “spider bite” should raise suspicion of an S. aureus infection. Recent data suggest that MRSA as a cause of skin infections in the general community remains at high probability.