Consent to treatment is rooted in case law. Consent to research, in contrast, has its basis in ethical codes, statutes, and administrative regulations, with the courts playing a lesser role.
What are some problems with informed consent?
- Source documents must reflect that consent was obtained before the start of study treatment and procedures
- A copy of the signed consent form must be kept at the site
- All versions of approved consent forms must be kept in the site study file; only the current Institutional Review Board (IRB) approved version may be used to consent new patients.[14]
What are the required elements of informed consent?
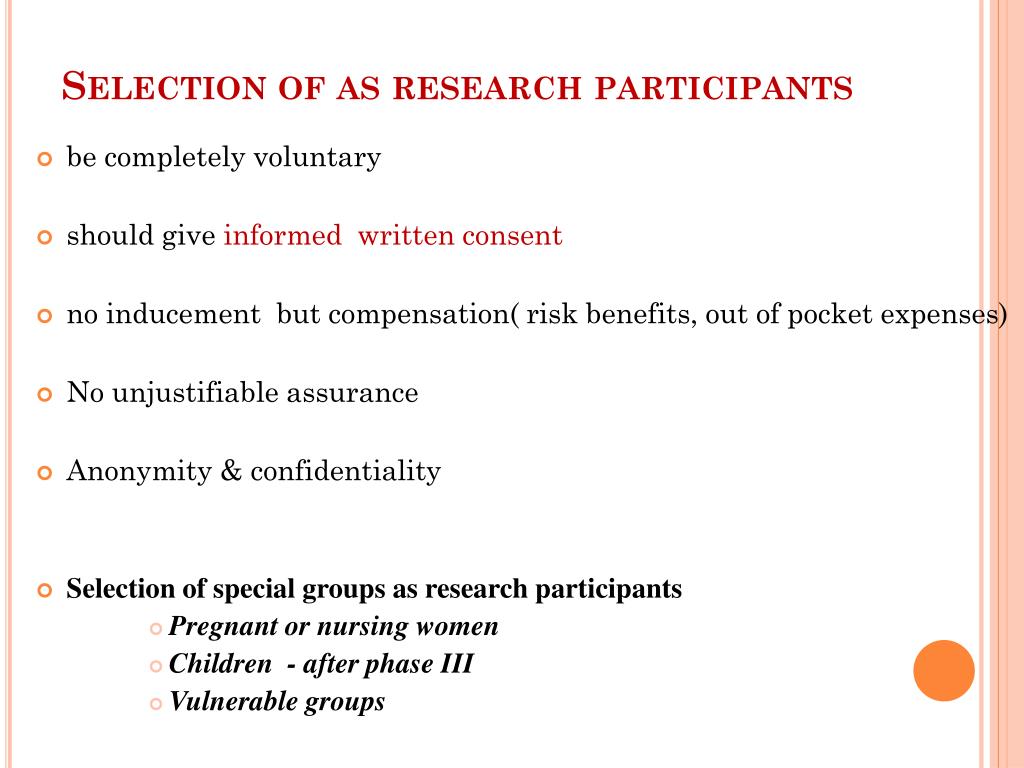
Valid informed consent for research must include three major elements: (1) disclosure of information, (2) competency of the patient (or surrogate) to make a decision, and (3) voluntary nature of the decision. US federal regulations require a full, detailed explanation of the study and its potential risks.
What is informed consent in clinical research?
- The human subjects are in a life-threatening situation that necessitates urgent intervention;
- Available treatments are unproven or unsatisfactory;
- Collection of valid scientific evidence is necessary to determine the safety and effectiveness of the intervention;
What do you need to know about informed consent?
What do I need to know about Informed Consent, Parental Consent and Child Assent forms?
- Obtaining Consent for EXEMPT Research. The consent process and its related documents can be simpler than those required for review mechanisms.
- Obtaining Consent for EXPEDITED and FULL Review projects. ...
- Research Involving Children/Minors. ...
- Child Assent Process. ...
- Approval for Consent Waiver or Permission to Alter the Consent Process. ...

What are the 3 requirements of consent?
Valid informed consent for research must include three major elements: (1) disclosure of information, (2) competency of the patient (or surrogate) to make a decision, and (3) voluntary nature of the decision. US federal regulations require a full, detailed explanation of the study and its potential risks.
What are the 5 elements that should be part of consent?
B. Basic Elements of Informed ConsentDescription of Clinical Investigation. ... Risks and Discomforts. ... Benefits. ... Alternative Procedures or Treatments. ... Confidentiality. ... Compensation and Medical Treatment in Event of Injury. ... Contacts. ... Voluntary Participation.
What are the 4 types of medical consent?
There are 4 components of informed consent including decision capacity, documentation of consent, disclosure, and competency. Doctors will give you information about a particular treatment or test in order for you to decide whether or not you wish to undergo a treatment or test.
What type of consent is required for research?
informed consentThe HHS regulations require that an investigator obtain legally effective informed consent from subjects or a legally authorized representative before the subjects may be involved in research (45 CFR 46.116), unless this requirement has been waived by an IRB.
What is research consent?
Informed consent is an ongoing communication process between research participants and the investigator to ensure participants' comfort. Informed consent allows potential research participants to volunteer their participation freely, without threat or undue coaching.
What is healthcare consent?
Consent to treatment means a person must give permission before they receive any type of medical treatment, test or examination. This must be done on the basis of an explanation by a clinician.
What are the two types of consent for medical treatment?
There are two types of consent that a patient may give to their medical provider: express consent and implied consent. Express consent is typically done in writing, while implied consent is typically conveyed through a patient's actions or conduct.
What are the main types of consent?
There are three different types of consent an organization may obtain:Explicit Consent.Implicit Consent.Opt-out Consent.
How do you ensure informed consent in research?
Getting informed consentare prepared and not surprised by the research activities they will be involved in - make sure you give them the sheet before the research session.know how you will be recording the sessions and any data you want to collect.do not feel pressured to agree to things they're not comfortable with.
What are some examples of informed consent?
I understand that my participation is voluntary and that I am free to withdraw at any time, without giving a reason and without cost. I understand that I will be given a copy of this consent form. I voluntarily agree to take part in this study.
What is informed consent?
The practice of informed consent has historical roots in various disciplines, including medicine, moral philosophy, and the law. It is closely tied to philosophical notions of respect for persons and respect for individual autonomy. Consent to treatment is rooted in case law.
Is consent to treatment a case law?
Consent to treatment is rooted in case law. Consent to research, in contrast, has its basis in ethical codes, statutes, and administrative regulations, with the courts playing a lesser role.
What is consent to treatment?
Consent to treatment is the agreement that an individual makes to receive medical treatment, care, or services, including tests and examinations. Anyone who can independently decide whether they want treatment must provide consent.
What is written consent?
Written consent involves completing and signing a consent form, which is a legal document that gives the doctor permission to proceed with the treatment. Consent forms ensure that doctors provide the appropriate information related to the medical condition and treatment options and that the individual selects their preferred option.
What is the obligation of healthcare professionals?
Healthcare professionals have an ethical and legal obligation to disclose information related to various treatment options to help people make an informed choice. This includes the risks, possible outcomes, and alternative options, if they are available. Healthcare providers can provide information verbally or in writing. They may also provide audio or video materials.
What does it mean when you don't have the mental capacity to comprehend treatment choices?
In these cases, the healthcare team must make the decisions that best serve the interests of the individual.
What is informed consent?
Informed consent requires the healthcare professional to provide information that outlines what the treatment entails, the benefits and risks, and other potential treatment options. They must also explain to the person the possible outcomes of refusing the recommended treatment.
What is nonverbal consent?
Nonverbal consent, sometimes called implied or implicit consent, includes gestures such as nodding the head, extending the arm for a blood test, or opening the mouth during a dental exam. Doctors may refer to verbal consent as explicit consent.
How old do you have to be to get treatment?
In most cases, young people aged 16 or 17 have the capacity to consent to treatment without acquiring consent from a person with parental responsibility.
How to meet the legal requirements for informed consent?
The best way to meet the legal requirements of informed consent is to develop a consistent practice of involving patients in decisions, even if that involvement may occasionally be limited (Box 2).1,6,45,58–61As with any aspect of medical practice, a systematic approach is important. Clinicians can develop a system to ensure that the discussion is not limited to the disclosure of risks, but also includes relevant details about the expected benefits, possible alternatives, and what to anticipate before and after the procedure. Furthermore, clinicians can ensure that the patient or surrogate has the capacity to make decisions, and that the choice is being made voluntarily without undue influence.
Why is informed consent important?
Informed consent has become the primary paradigm for protecting the legal rights of patients and guiding the ethical practice of medicine. It may be used for different purposes in different contexts: legal, ethical or administrative (Figure 1). Although these purposes overlap, they are not identical, thus leading to different standards and criteria for what constitutes “adequate” informed consent.
How long does it take to get informed consent?
A rigorous informed consent process is difficult and takes time from busy clinical schedules. Such time commitments are rarely recognized or rewarded by health care administrators. A recent study measured the time required for providers to obtain informed consent for elective surgery when using an electronic form.45In that study, the mean time taken by the provider was 10.9 minutes, with a large standard deviation (22 min).45Studies involving orthopedic and vascular surgeons showed similar results — the average time needed to obtain consent for orthopedic procedures was 16.1 (range 3–76) minutes;46the average was 12.1 (range 5–20)47minutes for a carotid endarterectomy. These measurements very likely underestimate the true time commitment involved, because they only included the time spent discussing the form. Additional time required for any discussions that the patient may have had with his or her primary care provider before the surgical referral, or with the nurses, midlevel providers or the surgeon in the surgical outpatient area before completing the formal documentation, was not included.
What are the elements of informed consent?
Although legal and ethical debate persists, most stakeholders in the informed consent process agree on at least four basic elements for discussions of informed consent: the decision-maker (i.e., the patient or a surrogate) should have the capacity to make decisions; the physician should disclose sufficient details for the decision-maker to make an informed choice; the decision-maker should show his or her understanding of the disclosed information; and the decision-maker should freely authorize the treatment plan.
When was informed consent first used?
Although the concept of consent is rooted in ancient legal and philosophical precepts, the modern legal precedent for “simple” consent was written in 1914, establishing a patient’s “right to determine what shall be done with his body.”2The further obligation for physicians to disclose details about treatment in a process of informed consent did not emerge until the 1950s,3when courts first required physicians to disclose information customarily disclosed by experienced clinicians (e.g., the reasonable physician standard). It was not until 1975 that American courts articulated the reasonable person standard, which required that physicians disclose the information that a “reasonable person” would want to know in a similar situation.4Regardless of the standard used, informed consent is further predicated on the patient’s or surrogate’s capacity to make decisions — not only should the decision-maker understand the relevant information, he or she should also be able to appreciate the information’s importance and use it to weigh treatment options in light of their values.5
What is explicit care?
Explicitly establish the goals of care, and prioritize them in the context of the patient’s other life goals.
What is shared decision making?
To address this concern, there is a growing focus on a shared process of decision-making — a process that emphasizes the critical importance of patient input while recognizing that it should be tailored to each patient’s ability for and interest in participation, and that the physician’s contribution to the decision is important and deserving of its own respect.55To the extent that medical treatment is a partnership between patient and clinician, the moral responsibility for decisions is carried by both partners. Neither partner should dominate the decision, nor should either partner be disenfranchised from their prerogative and privilege to participate as a moral agent in the decision. Support for this paradigm shift was recently articulated by an international consensus panel in the “Salzburg statement on shared decision making” (Appendix 1, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.112120/-/DC1.), which calls on clinicians, patients and policy-makers to change their practices, expectations and laws to more thoroughly share the responsibility for decision-making between clinician and patient.56
How far in advance of research participation can consent be obtained?
The HHS regulations at 45 CFR part 46 do not specify how far in advance of study entry a subject can provide consent. The amount of time required by a subject to make a decision would presumably depend on the nature of the study, taking into account, among other factors, the degree of risk, potential benefits, alternatives, and desire to consult with family members or others. However, if a prolonged period of time elapses from the date of consent to the date of entry into the study even if there have been no changes in the study design or no new significant findings affecting the study it might be prudent to review the information contained in the consent form with the subject prior to initiating any research procedures with the subject.
What is informed consent and when, why, and how must it be obtained?
When informed consent is required, it must be sought prospectively, and documented to the extent required under HHS regulations at 45 CFR 46.117. [Food and Drug Administration (FDA) regulations at 21 CFR part 50 may also apply if the research involves a clinical investigation regulated by FDA.]
What are the basic elements of informed consent?
The basic required elements of informed consent can be found in the HHS regulations at 45 CFR 46.116 (a). Also see OHRP Informed Consent Tips.
What constitutes coercion or undue influence when students are involved in research in a college or university setting?
The regulations require that the investigator seek consent only under circumstances that minimize the possibility of coercion or undue influence ( 45 CFR 46.116 ). The Office for Human Research Protections (OHRP) recommends that institutions have policies in place that clarify for students and faculty that any participation of students in research must be voluntary. Reasonable levels of extra credit or rewards may be offered for participating in research. If extra credit or rewards are offered for participation, students must be provided with and informed of non-research alternatives involving comparable time and effort to obtain the extra credit in order for the possibility of undue influence to be minimized. However, if participation in research is a course requirement, students must be informed of non-research alternatives involving comparable time and effort to fulfill those requirements in order for the possibility of undue influence to be minimized. Moreover, students must not be penalized for refusing to participate in research ( 45 CFR 46.116 (a) (8) ).
What constitutes coercion or undue influence when employees are the subjects of research?
The issues involving employees as research subjects are essentially identical to those involving students as research subjects: that is, investigators and IRBs must be cautious about the potential for coercion or undue influence and the need to protect confidentiality.
Should the initial consent or parental permission procedure ever be repeated or supplemented?
Likewise, for research involving children, permission of the potential subjects' parents or guardians must be obtained ( 45 CFR46.408 (c) ), unless an IRB has waived this requirement. Ensuring an adequate consent or parental permission process may require repeating or supplementing the initial consent procedure. The regulations also stipulate that “An investigator shall seek such consent only under circumstances that provide the prospective subject or the representative sufficient opportunity to consider whether or not to participate and that minimizes the possibility of coercion or undue influence” ( 45 CFR 46.116 ). This requirement also might necessitate repeating or supplementing the initial consent procedure.
Can records or databases be reviewed to identify potential subjects without obtaining informed consent or parental permission?
Yes, under certain circumstances. Although the HHS regulations do not specifically reference this type of activity, sometimes referred to as “preparatory to research,” such an activity must be reviewed and approved by an IRB in accordance with HHS regulations at 45 CFR 46.109 (a) when:
Why is informed consent important?
Informed consent is an essential safeguard in research. The obligation to obtain informed consent arises out of respect for persons and a desire to respect the autonomy of the individual deciding whether to volunteer to participate in biomedical or health research. For these reasons, no person may be used as a subject in research against his ...
What is the nature of an experimental drug?
The nature of the experimental drug (s), device (s), or procedure (s) to be used in the research. Any conflicts of interest relating to the research, in keeping with ethics guidance. Any known risks or foreseeable hazards, including pain or discomfort that the participant might experience.
Can informed consent be waived?
In certain situations, with special safeguards in keeping with ethics guidance, the obligation to obtain informed consent may be waived in research on emergency interventions.
What are the different types of consent?
There are three main types of consent for medical treatment: verbal, written, and implied consent. Each type is applicable in various cases, and each one requires different procedures and considerations.
What is the third type of consent?
The third type of consent for medical treatment is based on a person’s ability to understand and give consent. This is considered voluntary consent. The person is expected to make his or her own decisions regarding the medical treatments, and the doctor or the physician is allowed to make his or her own decisions concerning any procedure or any part of the medical procedure.
What is a court order for incapacity?
In the case of an incapacitated individual, a court order allows the person to give the necessary consent for medical treatment. It also authorizes the medical practitioner to carry out the procedure for a specified period or to a definite hospital, depending on the condition and type of incapacity of the individual. The consent needs to be given at the time of the medical examination or a later date when the patient is in a stable state.
What does it mean when a doctor says he is not competent?
A person is not competent if he or she does not want to undergo any medical treatment. In such a case, the doctors have to take certain actions to help the patient to agree to the procedure. If the doctor determines that the patient is in a stable condition, the doctors can go ahead with the procedure. If the patient is unconscious, then the doctors must notify the court about the refusal of consent.
Why is it difficult for an incapacitated person to give consent?
Under certain circumstances, it may be difficult for an incapacitated person to consent because of his or her physical condition or other health issues. In such cases, it is recommended that his or her parents or guardians or any other adult close to the incapacitated individual can be asked by the doctor to be present at the medical examination so that they could give consent on behalf of their minor wards.
Can an adult consent to medical care in Maryland?
The general rule, according to Maryland law, is that an adult can legally consent to medical care for him or herself only if it is determined that he or she can do so. This capacity depends on several factors: the individual’s age, the maturity of capacity to understand the nature and consequences of the procedure. It is also determined by the patient’s status as a dependent of another person.
Can a person give consent to a surrogate in Maryland?
A person can give consent for his or her own self, but he or she has no legal responsibility or accountability to provide for the treatment. If the individual is not capable of giving informed consent due to unconsciousness or lack of mental capacity, Maryland law gives for surrogate decision-making and for a guardian to be appointed by court order. Also, in certain cases where a parent is unable to take care of his or her child or children due to health or disability, the court appoints a guardian for them.
What is consent in research?
The term consent implies that a research subject is not a minor and is capable of fully understanding the implications of the research in which s/he will participate. The subject understands all the benefits and risks as well as the purpose of the study and can therefore give truly informed consent.
What is the difference between informed consent and assent?
However, consent is legally binding. Informed consent means that the subject is able to understand what the study or treatment is all about , why it is being done, how it is expected to benefit him/her , and any existing risks or side effects because he/she has been informed by the researcher and has given permission. Informed consent is required by law for all research participants and ensures the autonomy of these subjects.
What should be made by the investigating researcher to ensure that the child understands what being a subject in the research project?
Every effort should be made by the investigating researcher to ensure that the child understands what being a subject in the research project will entail. Educational materials, like videos, pictures, or other learning aids that are age-appropriate for the child, can be used to help increase understanding.
What is the code of ethics for medical research?
The American Medical Association (AMA) has a code of medical ethics that outlines the elements necessary to establish informed consent. These elements must be applied in health care, as in the signing of treatment consent forms and in research projects as well. In addition to this, legislation known as the Common Rule, or Federal Policy for the Protection of Human Subjects regulations, was published in 1991, outlining the requirements for informed consent for subjects of research. Some of the most important of these elements and requirements include:
What is full disclosure in research?
Full Disclosure - The researcher must disclose all aspects of participation in the research project to the subject, including any pain, suffering, or hazards that may occur during the research. The researcher must also make it clear that there are alternative treatments available or that taking no treatment or not participating at all is also an option. The likelihood that participating in the research will benefit the subject is an issue that should also be discussed.
Can a minor give consent to a research study?
A minor may not give informed consent and must have a parent or legal guardian do so for him/her. However, efforts should be made to help the child understand what participating in the research will entail.
Do you have to be a Study.com member to unlock this lesson?
To unlock this lesson you must be a Study.com Member.
Who put strict rules on clinical studies?
Strict rules for clinical studies have been put in place by National Institutes of Health and the FDA. Some studies involve promising new treatments that may directly benefit participants. Others do not directly benefit participants, but may help scientists learn better ways to help people.
Why is confidentiality important in clinical research?
Confidentiality is an important part of clinical research and ensures that personal information is seen only by those authorized to have access. It also means that the personal identity and all medical information of clinical trial participants is known only to the individual patient and researchers.
Who should consider clinical trials and why?
Some people participate in clinical trials because none of the standard (approved) treatment options have worked, or they are unable to tolerate certain side effects. Clinical trials provide another option when standard therapy has failed. Others participate in trials because they want to contribute to the advancement of medical knowledge.
Where are clinical trials conducted?
The sponsor determines the location (s) of the trials, which are usually conducted at universities, medical centers, clinics, hospitals, and other Federal ly or industry-funded research sites.
What should I think about before joining a clinical trial?
Before joining a clinical trial, it is important to learn as much as possible. Discuss your questions and concerns with members of the health care team conducting the trial. Also, discuss the trial with your health care provider to determine whether or not the trial is a good option based on your current treatment. Be sure you understand:
Where can I find clinical trials?
One good way to find out if there are any clinical trials that might help you is to ask your doctor. Other sources of information include:
What is a placebo and how is it related to clinical trials?
A placebo is a pill, liquid , or powder that has no treatment value. It is often called a sugar pill. In clinical trials, experimental drugs are often compared with placebos to evaluate the treatment’s effectiveness.
