A medical authorization form is a form from the patient to a third party, permitting them to access your protected medical records. The form can either be limited in scope or can be as broad as granting access to the third parties to anything in your medical records.
What is a patient’s authorization to use medical records?
With a patient’s authorization, you have permission to use and disclose their medical record according to the agreement. Without it, using and disclosing a patient’s medical record would violate HIPAA and could result in hefty fines or prosecution.
What information is included in a treatment record?
Each page in the treatment record contains the patient's name/identification number. Each record includes the patient's address, employer or school, home and work telephone numbers including emergency contacts, marital/legal status, appropriate consent forms and guardianship information, if relevant.
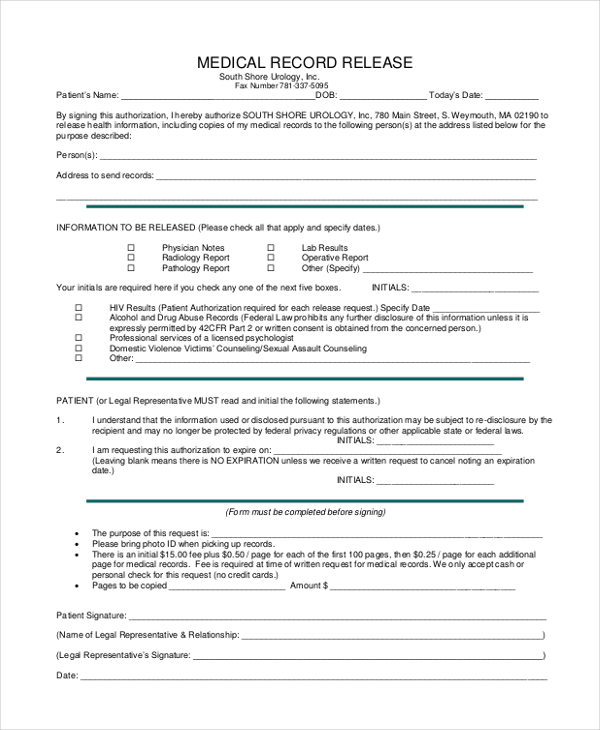
What is a medical record release authorization form under HIPAA?
Medical Records Release Authorization Form – HIPAA. The medical record information release (HIPAA), also known as the ‘Health Insurance Portability and Accountability Act’, is included in each person’s medical file. This document allows a patient to list the names of family members, friends, clergy, health care providers,...
How is the treatment authorization request processed?
Get information on how the Treatment Authorization Request are processed. Requirements are applied to specific procedures and services according to State and Federal law. Certain procedures and services are subject to authorization by Medi-Cal field offices before reimbursement can be approved. All inpatient hospital stays require authorization.
What is the purpose of an authorization form?
An authorization is a detailed document that gives covered entities permission to use protected health information for specified purposes, which are generally other than treatment, payment, or health care operations, or to disclose protected health information to a third party specified by the individual.
What is a patient authorization form?
A HIPAA patient authorization form is an agreement between a patient and healthcare provider. A signed form gives your organization permission to use the patient's health information or disclose it to another person or entity, depending on their wishes.
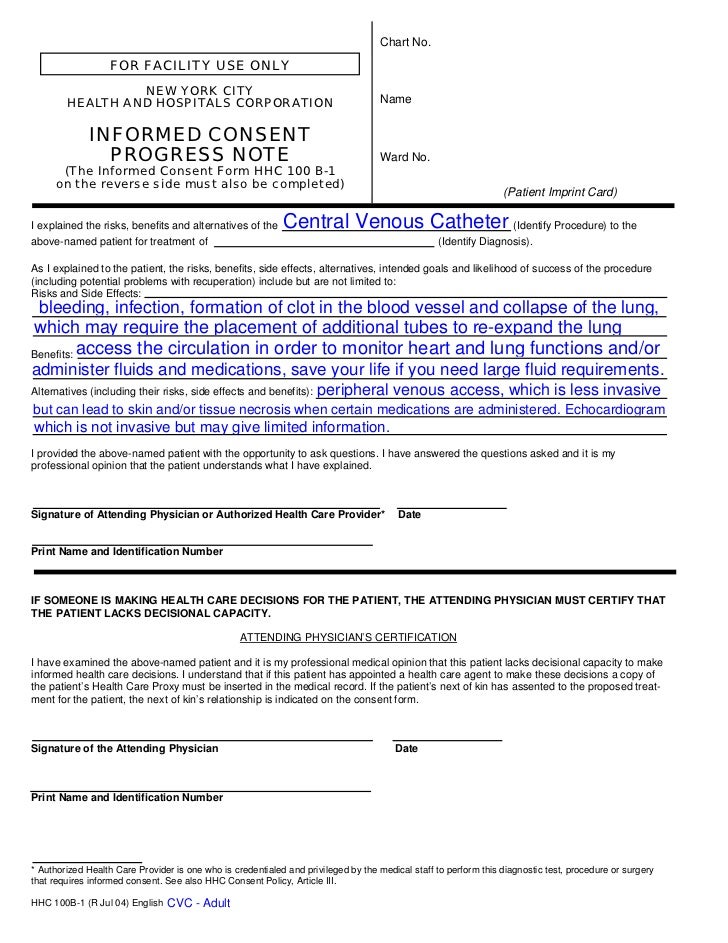
What is a document signed by a patient authorizing treatment?
A HIPAA authorization form is a document in that allows an appointed person or party to share specific health information with another person or group. Your appointed person can be a doctor, a hospital, or a health care provider, as well as certain other entities such as an attorney.
What is an authorization form?
An authorization form is a document that is duly endorsed by an individual or organisation which grants permission to another individual or organisation to proceed with certain actions. It is often used to grant permission to carry out a specific action for a fixed period of time.
What are the 8 requirements of a valid authorization to release information?
Valid HIPAA Authorizations: A ChecklistNo Compound Authorizations. The authorization may not be combined with any other document such as a consent for treatment. ... Core Elements. ... Required Statements. ... Marketing or Sale of PHI. ... Completed in Full. ... Written in Plain Language. ... Give the Patient a Copy. ... Retain the Authorization.
Is a patient authorization necessary to treat a patient?
Answer: No. The HIPAA Privacy Rule permits a health care provider to disclose protected health information about an individual, without the individual's authorization, to another health care provider for that provider's treatment of the individual.
What is the difference between authorization and consent?
A: “Consent” is a general term under the Privacy Rule, but “authorization” has much more specific requirements. The Privacy Rule permits, but does not require, a CE to obtain patient “consent” for uses and disclosures of PHI for treatment, payment, and healthcare operations.
What is the difference between consent and authorization to use patient specific health information?
Consent refers to an agreement by the patient to allow the health-care provider to use this information to carry out treatment, payment, and health-care operations. Authorization refers to the permission for the health-care provider to make specific disclosures not otherwise authorized by law.
What is signed authorization?
An Authorization is a document signed by a person to allow disclosure of their protected health information (PHI) to somebody outside the covered entity that stores the PHI.
How do I create an authorization form?
5 Steps to Create an Authorization FormStep 1: Include Parties. There are three parties involved in an Authorization transaction. ... Step 2: Add Name and Address. ... Step 3: Explain the Duties. ... Step 4: State the Reason. ... Step 5: Mention the Restrictions.
Which of these disclosures does require written authorization?
A covered entity must obtain the individual's written authorization for any use or disclosure of protected health information that is not for treatment, payment or health care operations or otherwise permitted or required by the Privacy Rule.
Why is it important to have patients sign a medical authorization form before any treatments or procedure?
It is important to have the patients sign a medical authorization form before any treatments or procedure to protect yourself from any litigation that may arise afterward. We hope that this guide has provided you with all the information that you need to get started on your medical authorization form.
Why do you need a medical authorization form?
The other reason why you may want to have used a medical authorization form is when you are sick and the medicine or procedure that the doctors are still in the trial phases. Since the doctors are not entirely sure of whether the medicine or procedure works 100%, they will have to seek your consent in order to proceed.
Can a hospital share medical records without consent?
If the doctors, hospital, or health care providers can not share the patient’s medical records without their consent, i.e., if sharing of such information is illegal. Suppose the patient requires emergency treatment. They must first sign a consent form before the doctors can proceed with the treatment.
What does each record mean in a prescription?
Each record indicates what psychotropic medications have been prescribed, dosages of each, and dates of prescription or refills . Each record indicates that psychotropic medication side effects have been explained. Each record indicates that results of laboratory tests, if ordered, have been documented and reviewed.
What is included in a medical record?
All entries in the record include the provider's name, signature, professional degree, and identification number (if applicable). All entries are legible. All entries are dated. Each record includes copies of appropriate release of information, consistent with State/Federal regulations. Informed consent for medication/treatment and ...
What is a substance abuse assessment?
A substance abuse assessment for patients 12 and older, which includes past and present use of cigarettes and alcohol, as well as illicit, prescribed and over-the-counter drugs, is documented .
What is the focus of treatment interventions?
The focus of treatment interventions is consistent with the treatment plan goals and objectives. Progress notes describe patient strengths and limitations in achieving treatment plan goals and objectives. Patient/family education and recommendations are documented.
Do providers have to keep treatment records?
Providers will maintain confidentiality of treatment records according to applicable state and federal regulations. Providers will limit access to treatment records. Providers will release treatment records only in accordance with a court order, subpoena or statute.
Do treatment records need to be secure?
Treatment record locations must be secure and accessed only by approved personnel. Any treatment records sent to storage must be secure and retrievable. The treatment record must be available at each appointment. Purging of treatment records must be done according to state statute.
What is HIPAA authorization form?
A HIPAA authorization form gives covered entities permission to use protected health information for purposes other than treatment, payment, or health care operations. Continue reading to find out what authorization to disclose health information is needed.
What is required before a HIPAA authorization form?
HIPAA Authorization forms are required before: The covered entity can use or disclose PHI whose use or disclosure is otherwise not permitted by the HIPAA Privacy Rule. The covered entity can use or disclosure of PHI for marketing purposes. If the marketing communication involves direct or indirect remuneration to the covered entity ...
What is the HIPAA Privacy Rule?
The HIPAA Privacy Rule requires that an individual provide signed authorization to a covered entity, before the entity may use or disclose certain protected health information (PHI). Under the Privacy Rule and in accordance with the minimum standards, doctors, nurses, hospitals, laboratory technicians, and other health care providers ...
When does the authorization have to state that remuneration is involved?
If the marketing communication involves direct or indirect remuneration to the covered entity from a third party, the authorization must state that such remuneration is involved. When the communication involves a promotional gift of nominal value.
Can an individual revoke an authorization in writing?
The individual‘s right to revoke the authorization in writing. The exceptions to the right to revoke (an individual may revoke an authorization in writing except when the covered entity has taken action in reliance on the authorization). The covered entity may not condition treatment, payment, enrollment or eligibility for benefits on whether ...
Can a covered entity condition treatment?
The covered entity may not condition treatment, payment, enrollment or eligibility for benefits on whether the individual signs the authorization, except that: A covered health care provider may condition the provision of research-related treatment on provision of an authorization for such research. A health plan may, to make eligibility ...
Do you need to provide a copy of a HIPAA authorization?
In addition, whenever a covered entity seeks a HIPAA authorization from an individual for a PHI use or disclosure, the covered entity must provide the individual with a copy of the signed authorization.
Who can access medical records of a deceased person?
If for any reason the medical records of the deceased are requested, the administrator appointed in the Last Will and Testament or a court-appointed authority may be able to obtain the records.
Who has the power to obtain medical records?
In addition, any person that has been appointed by a court to act as a caregiver or guardian, the judgment, order, or decree must be attached to the HIPAA release form.
What happens if a patient is not listed on HIPAA?
If anyone would ask for medical information regarding a specific patient and their name is not listed on the HIPAA form, they would not be privy, by law , to any of the patient’s information under any circumstances. The document also provides the ability for healthcare providers to share information with each other.
How long does it take to get medical records?
Accessing and obtaining your medical records is a requirement under 45 CFR 164.524 which requires that any request made to access or transfer medical records must be completed within 30 days or a letter must be sent to the requestor stating why the records are delayed.
What is the legal option for obtaining medical records for a minor?
Option 2 – Adult or Legal Guardian. An adult or legal guardian is legally authorized, under federal law, to obtain the medical records of a minor. If the medical records are for healthcare services that will be provided, the minor may be required to consent to such care based on State law.
Do you have to pay for a copy of medical records?
Yes but this depends on the medical office. Generally speaking, smaller offices tend to not require a fee for copying and transferring medical records to another office. If the medical office does charge a fee, it cannot be more than the maximum limit in the State (see table below).
Can a medical facility charge for sending a letter?
The medical facility may charge a fee for sending the records, although, they are prohibited from charging for processing the request.
What is a patient's authorization?
With a patient’s authorization, you have permission to use and disclose their medical record according to the agreement. Without it, using and disclosing a patient’s medical record would violate HIPAA and could result in hefty fines or prosecution. So, you must know how to get an authorization correctly.
What is a HIPAA authorization form?
A: A HIPAA authorization form represents an agreement between a patient and a HIPAA-covered organization. A signed form gives your organization permission to use the patient’s PHI or disclose it to another person or entity. You need a signed form to:
Do you need authorization to use PHI?
A: In some cases, you don’t need patient authorization to use and disclose their protected health information (PHI). For instance, you can use and disclose PHI for treatment, payment, and healthcare operations (TPO). Other special circumstances include:
Do you put expiration date on a research database?
However, if you’re creating a research database/repository, the expiration date would be “none.”. The patient’s date and signature. If a representative is signing for the patient, they must describe their authority to do so.
Do you need to notarize a HIPAA authorization?
A: No. The HIPAA Privacy Rule does not require you to notari ze authorization forms or have a witness. Download an authorization form from HHS. Though taking the time to fill out an authorization form and get a patient’s signature is an extra step, it’s an important one that you can’t afford to overlook.
