What percentage of gastric emptying is normal 4 hours after gastric bypass?
At 4 hours: 0-10%. (More than 10% at 4 hours is considered delayed gastric emptying). You should note that these numbers are different according to the hospital or center performing the test.
How should I prepare for a gastric emptying study (get)?
How should I prepare for a Gastric Emptying Study (GET)? You should be not eat or drink anything after midnight the day before the test, and until after the test is completed. How long does the test take? This test takes four and half hours to complete in one visit.
What are the results of the gastric emptying study?
Gastric emptying study results explained: 1- Normal values.. At one hour after the meal: 37-90% of the meal is still inside your stomach. At 2 hours: 30-60%. 3- Borderline delayed gastric emptying.. Borderline delayed gastric emptying results are gastric retention values around... 4- Abnormal ...
How is delayed gastric emptying classified in gastroparesis?
Further classification of the severity of the gastroparesis (delayed gastric emptying) is obtained at the 4 hours measurement. According to the percentage of meal retained at 4 hours, delayed gastric emptying is classified into: Mild: 10-15% of the meal is still retained.
What should I do after gastric emptying study?
You may be able to leave the exam room during this time period but will need to sit quietly. You should not smoke or eat while you wait. Your provider will let you know when you need to return for imaging. The amount of the substance found in your breath samples can help show how fast the stomach has emptied.
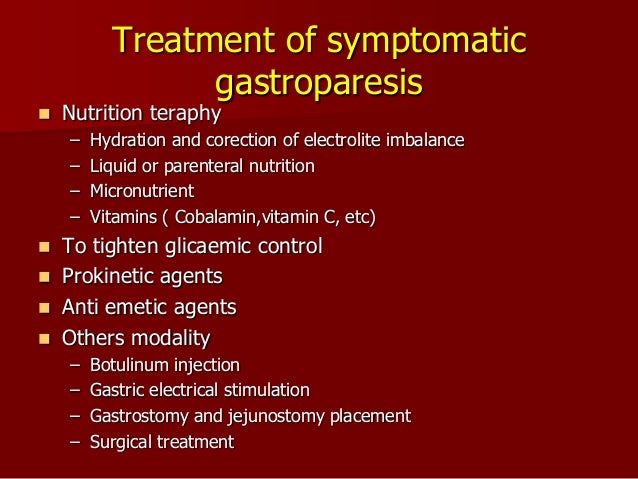
How do you fix delayed gastric emptying?
How do doctors treat gastroparesis?eat foods low in fat and fiber.eat five or six small, nutritious meals a day instead of two or three large meals.chew your food thoroughly.eat soft, well-cooked foods.avoid carbonated, or fizzy, beverages.avoid alcohol.More items...
How long does gastroparesis take to heal?
Gastroparesis then is a complex, multifactor, chronic, digestive disease state with possible genetic, physiological, immune, psychological, social and environmental interplays. Gastroparesis has been documented to occur as a sequel to viral gastroenteritis, slowly resolving over one to two years.
Can delayed gastric emptying be reversed?
There's no cure for gastroparesis. It's a chronic, long-term condition that can't be reversed.
How do you increase GI motility?
If your transit time is a concern, there are some steps you can take to speed things up.Exercise for 30 minutes a day. Food and digested material is moved through the body by a series of muscle contractions. ... Eat more fiber. ... Eat yogurt. ... Eat less meat. ... Drink more water.
What is the best medication for gastroparesis?
Medications to treat gastroparesis may include:Medications to stimulate the stomach muscles. These medications include metoclopramide (Reglan) and erythromycin. ... Medications to control nausea and vomiting. Drugs that help ease nausea and vomiting include diphenhydramine (Benadryl, others) and ondansetron (Zofran).
What medications make gastroparesis worse?
Medicines that may delay gastric emptying or make symptoms worse include the following: narcotic pain medicines, such as codeine link , hydrocodone link , morphine link , oxycodone link , and tapentadol link. some antidepressants link , such as amitriptyline link , nortriptyline link , and venlafaxine link.
Can gastroparesis be resolved?
Although there is no cure for gastroparesis, changes to the diet, along with medication, can offer some relief. Certain medications, such as some antidepressants, opioid pain relievers, and high blood pressure and allergy medications, can lead to slow gastric emptying and cause similar symptoms.
Do you have normal bowel movements with gastroparesis?
The delayed stomach emptying and reduced digestive motility associated with gastroparesis can have a significant impact on bowel function. Just as changes in bowel motility can lead to things like diarrhea and constipation, so also changes in stomach motility can cause a number of symptoms: nausea. vomiting.
Can gastroparesis go into remission?
Can Gastroparesis Be Reversed? While there is no cure, it is possible to go into remission for years, so following a treatment plan can significantly improve your quality of life.
Do probiotics help gastroparesis?
Bacterial overgrowth (SIBO) may accompany gastroparesis. The main symptom is bloating. Judicious use of antibiotics and probiotics may be helpful in the management of these symptoms. It is difficult for patients with nausea and vomiting to tolerate oral medications.
What foods should you avoid with gastroparesis?
Foods to avoid if you have gastroparesiscarbonated beverages.alcohol.beans and legumes.corn.seeds and nuts.broccoli and cauliflower.cheese.heavy cream.More items...
Lucretia Updated Friday at 07:05 PM
My allergic reaction to either a blood pressure medication or the surgical tape!!
Weight Loss Journey Updated February 9
I am going to try and upload pictures weekly if not monthly to see the progress. I had a RYGB Limb Lenghtening- January 19 2022
Before Surgery Updated September 24, 2021
All of these photos were from before September 21, 2021 (my RNY date) - I started at 255 lb in April of 2021 at my first...
What is the most common method of gastric emptying?
The most simple, cost-effective, and widely available technique is the “ Scintigraphic gastric emptying ” study. During the study, You typically ingest a small meal containing a radioactive substance. The meal can be: Solid (Typically egg white): the most common.
How long after a meal is the gastric emptying rate?
Normal values of the gastric emptying study (for the solid meal) are: At one hour after the meal: 37-90% of the meal is still inside your stomach. At 2 hours: 30-60%. (more than 60% is considered delayed gastric emptying). At 4 hours: 0-10%. (More than 10% at 4 hours is considered delayed gastric emptying).
What does a gastric emptying study diagnose?
The gastric emptying study assesses how fast your stomach empties. The emptying study can detect either delayed gastric emptying (gastroparesis) or rapid gastric emptying (gastric dumping).
What is gastric dumping?
Gastric dumping is defined as RAPID gastric emptying. As a result, sugar rapidly moves from the stomach to the intestine producing symptoms Such as:
How do you know if you have gastroparesis?
Symptoms of Gastroparesis include: Nausea (93%) Vomiting (Up to 84 %) Abdominal pain or discomfort (Up to 90%). Early satiety (Up to 86%) Fullness after meals, bloating. Weight loss in severe cases. Learn more about gastroparesis.
Why does food stay in your stomach longer?
With gastroparesis, your stomach is unable to effectively process the food inside. As a result, food stays longer inside your stomach. Diabetes Mellitus: The most recognized cause of gastroparesis. Viral infections: Some studies show that gastroparesis can occur due to some viral infections.
How much of the meal is retained?
Mild: 10-15% of the meal is still retained.
What is a Gastric Emptying Study (GET)?
A Gastric Emptying Study is a test to determine the time is takes a meal to move through a person’s stomach. It is typically ordered by physicians for patients with frequent vomiting, gastroparesis, abdominal pain, early satiety and pre-operative evaluation.
How should I prepare for a Gastric Emptying Study (GET)?
You should be not eat or drink anything after midnight the day before the test, and until after the test is completed.
How long does the test take?
This test takes four and half hours to complete in one visit. When you arrive to the Nuclear Medicine Department a technologist will take you to a room and give you a meal to eat. The normal meal is 4 oz. of egg beaters scrambled; 2 pieces of toast with jam; and 6 oz. of water. In the scrambled eggs will be a radioactive isotope.
How soon will the scan results be available?
A radiologist will interpret the images, write a report, and deliver the results to your doctor via the internal computer system.
What is the best pre and post op pictorial aid for you to visualize how you will appear after losing?
As the old adage goes, “A picture can say more than a thousand words.” Gastric sleeve before and after female pictures are the best pre and post op pictorial aid for you to visualize how you will appear after losing your excess body weight.
How long does it take to lose weight after a gastrectomy?
Most women are able to lose about 60 to 70 percent of their excess weight within the first one to two years after a (VSG) vertical sleeve gastrectomy in Mexico.
Why did Christina get the gastric sleeve?
Christina was inspired to seek out gastric sleeve surgery after being inspired by many patients success stories noting that others who have gone through this process understand the feelings you go through in choosing to have weight loss surgery. “I looked in the mirror one day and I could see the real me in there,” she recalls. “I made the decision to get the gastric sleeve and it was so very worth it!”
What is gastric sleeve surgery?
Gastric sleeve surgery in Mexico is a bariatric procedure that will limit the size of your stomach so that you will naturally consume less food and achieve your desired weight loss. Gastric sleeve before and after pictures tell a compelling tale of how you can achieve a dramatic body transformation with the VSG surgery.
Why did Christy Biddle eat so much before bariatric surgery?
From running to the fridge to running marathons! Christy Biddle admits that her habits before bariatric procedure included impulse eating due to boredom or stress and she would often eat larger than necessary portions. The turning point for Christy in seeking out gastric sleeve surgery with Jet Medical Tourism was when the scales tipped 300 pounds. “I was diagnosed with health issues like high blood pressure and high cholesterol by this point.” Christy recalls.
How much weight did Kendall M. lose?
Stepping on the scale, Kendall M. found herself staring down 200 pounds total weight and a mounting social anxiety at the thought of being around people. She felt so uncomfortable in her own skin and hoped that bariatric surgery would help her lose excess weight and get down to her ideal weight of 135 pounds.
What type of sleeve is before and after female?
Type: Gastric S leeve Before and After Female Picture
How to treat gastroparesis?
Some complementary and alternative therapies have been used to treat gastroparesis, including acupuncture. Acupuncture involves the insertion of extremely thin needles through your skin at strategic points on your body. During electroacupuncture, a small electrical current is passed through the needles. Studies have shown these treatments may ease gastroparesis symptoms more than a sham treatment.
How to monitor the rate of food leaving your stomach?
A scanner that detects the movement of the radioactive material is placed over your abdomen to monitor the rate at which food leaves your stomach. You'll need to stop taking any medications that could slow gastric emptying. Ask your doctor if any of your medications might slow your digestion. Breath tests.
What is gastric electrical stimulation?
In gastric electrical stimulation, a surgically implanted device provides electrical stimulation to the stomach muscles to move food more efficiently. Study results have been mixed. However, the device seems to be most helpful for people with diabetic gastroparesis.
What test is used to test for gastroparesis?
Gastric emptying tests. To see how fast your stomach empties its contents, one or more of these tests may be recommended: Scintigraphy. This is the most important test used in making a diagnosis of gastroparesis. It involves eating a light meal, such as eggs and toast, that contains a small amount of radioactive material.
What is the procedure used to examine the digestive system?
Upper gastrointestinal (GI) endoscopy. This procedure is used to visually examine your upper digestive system — your esophagus, stomach and beginning of the small intestine (duodenum). It uses a tiny camera on the end of a long, flexible tube.
Where do feeding tubes go?
Feeding tubes can be passed through your nose or mouth or directly into your small intestine through your skin . The tube is usually temporary and is only used when gastroparesis is severe or when blood sugar levels can't be controlled by any other method.
Where do you put a feeding tube?
In these situations, doctors may recommend a feeding tube (jejunostomy tube) be placed in the small intestine. Or doctors may recommend a gastric venting tube to help relieve pressure from gastric contents. Feeding tubes can be passed through your nose or mouth or directly into your small intestine through your skin.
What is delayed gastric emptying?
Delayed gastric emptying: whom to test, how to test, and what to do. Gastroparesis, or delayed gastric emptying, is a common cause of chronic nausea and vomiting as seen in a gastroenterology practice. Diabetic, postsurgical, and idiopathic causes remain the three most common forms of gastroparesis. In addition to nausea and vomiting, symptoms of ...
How long does it take for a gastric emptying test to be performed?
Extension of the gastric emptying test to 4 hours improves the accuracy of the test, but unfortunately, this is not commonly performed at many centers. Emptying of liquids remains normal until the late stages of gastroparesis and is less useful.
What are the symptoms of gastroparesis?
In addition to nausea and vomiting, symptoms of gastroparesis may include early satiety, postprandial fullness, and abdominal pain.
What should patients be advised to eat?
Patients should be advised to eat small meals and to limit their intake of fat and fiber. Additional dietary recommendations may include increasing caloric intake in the form of liquids.
What is the treatment for a patient who fails all medical therapy?
In patients for whom all medical therapy fails, other options that are tried at experienced centers include the injection of botulinum toxin into the pylorus, placement of a feeding jejunostomy, and/or placement of a gastric electrical stimulator.
What is the treatment for gastroparesis?
Other nonmedical therapies which are sometimes offered to patients include gastric outlet stenting (placing a stent in the pylorus and holding it open for food to pass through), gastric outlet my otomy (cutting the muscle of the pylorus to enable food to pass through) and in some rare cases, total gastrectomy (surgical removal of the stomach). In these difficult cases where standard medical therapies do not help, Johns Hopkins physicians work together in teams to create new and innovative therapies.
What to do if dietary changes do not improve symptoms?
If dietary changes and medication did not improve your symptoms, your doctor may perform an endoscopic procedure.
What is the membrane lining of the stomach called?
You undergo a small operation to place electrodes on the surface of the stomach called the gastric serosa, the membrane lining of the stomach.
What is the purpose of a jejunostomy tube?
Jejunostomy: If the gastrostomy tube is not effective, a jejunostomy tube will be left in place to ensure you remain properly hydrated and nourished. During a jejunostomy, a feeding tube is inserted through your abdomen and into your small intestine. This way, your small intestine receives the nutrients directly, bypassing the stomach.
Does Johns Hopkins offer gastric pacing?
Doctors at Johns Hopkins are at the forefront of novel therapies for patients with gastroparesis. In fact, we are the only health care center in Maryland to offer gastric pacing, a new approach to treating gastroparesis .
Can eating fat cause gastric emptying?
Eating foods that are lower in fiber and fat; both fiber and fat can cause a delay in gastric emptying
Does gastric pacing help with nausea?
Gastric pacing has been shown to decrease nausea in some patients ; however, data is still emerging and not all patients benefit. Talk to your Johns Hopkins gastroenterologist to see if gastric pacing is right for you.
How to prevent gastroparesis?
If you have diabetes, you can prevent or delay nerve damage that can cause gastroparesis by keeping your blood glucose levels within the target range that your doctor thinks is best for you. Meal planning, physical activity, and medicines, if needed, can help you keep your blood glucose levels within your target range.
How do doctors treat gastroparesis?
How doctors treat gastroparesis depends on the cause, how severe your symptoms and complications are, and how well you respond to different treatments. Sometimes, treating the cause may stop gastroparesis. If diabetes is causing your gastroparesis, your health care professional will work with you to help control your blood glucose levels. When the cause of your gastroparesis is not known, your doctor will provide treatments to help relieve your symptoms and treat complications.
How does gastric stimulation work?
Gastric electrical stimulation (GES) uses a small, battery-powered device to send mild electrical pulses to the nerves and muscles in the lower stomach. A surgeon puts the device under the skin in your lower abdomen and attaches wires from the device to the muscles in the wall of your stomach. GES can help decrease long-term nausea and vomiting.
What is the National Institute of Diabetes and Digestive and Kidney Diseases?
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. The NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by the NIDDK is carefully reviewed by NIDDK scientists and other experts.
What is a venting gastrostomy?
Venting gastrostomy. Your doctor may recommend a venting gastrostomy to relieve pressure inside your stomach. A doctor creates an opening, called a gastrostomy, in your abdominal wall and into your stomach. The doctor then places a tube through the gastrostomy into your stomach.
Where is the feeding tube placed?
Jejunostomy tube feeding is a way to feed you through a tube placed into part of your small intestine called the jejunum. To place the tube into the jejunum, a doctor creates an opening, called a jejunostomy, in your abdominal wall that goes into your jejunum. The feeding tube bypasses your stomach and delivers a liquid food directly into your jejunum.
Can you take IV nutrition for gastroparesis?
Parenteral nutrition. Your doctor may recommend parenteral, or intravenous (IV), nutrition if your gastroparesis is so severe that other treatments are not helping. Parenteral nutrition delivers liquid nutrients directly into your bloodstream. Parenteral nutrition may be short term, until you can eat again.