Tackling Type 1 Diabetes at a Cellular Level In individuals with type 1 diabetes, the body mistakenly attacks insulin-producing cells and destroys them. This leaves the body unable to regulate the amount of sugar in the blood or shift the sugar into cells that convert it into energy.
Full Answer
What is the molecular mechanism of Type 1 diabetes?
Keywords: type 1 diabetes, HLA molecules, molecular mechanisms. Type 1 diabetes is a multifactorial autoimmune disease, which is characterised by T cell mediated destruction of the insulin secreting β cells of the islets of Langerhans in the pancreas.
What is the best treatment for Type 1 diabetes mellitus?
For type 1 diabetes mellitus, resulting from selective destruction of insulin producing cells by exaggerated immune reaction, the only effective therapy remains exogenous insulin administration.
What is type 1 diabetes mellitus?
Diabetes mellitus is characterized by long standing hyperglycemia leading to numerous life-threatening complications. For type 1 diabetes mellitus, resulting from selective destruction of insulin producing cells by exaggerated immune reaction, the only effective therapy remains exogenous insulin administration.
Is it time to bring dendritic cell therapy to type 1 diabetes?
It's time to bring dendritic cell therapy to type 1 diabetes. Diabetes (2014) 63 :20–30. 10.2337/db13-0886 [ PMC free article] [ PubMed] [ CrossRef] [ Google Scholar] [ Ref list]

How does type 1 diabetes affect the body at a cellular level?
With type 1 diabetes, beta cells produce little or no insulin. Without enough insulin, glucose builds up in the bloodstream instead of going into the cells. This buildup of glucose in the blood is called hyperglycemia. The body is unable to use the glucose for energy.
What is the molecular basis of type 1 diabetes?
Susceptibility to type 1 diabetes is associated with two combinations of DQA1 and DQB1 alleles, namely: DQA1*0501. DQB1*0201 and DQA1*0301. DQB1*0302, which encode the HLA-DQ2 and HLA-DQ8 molecules, respectively.
How does type 1 diabetes treatment work?
If you have type 1 diabetes, you'll need to use insulin to treat your diabetes. You take the insulin by injection or by using a pump. If you have Type 2 diabetes, you may have to use insulin or tablets, though you might initially be able to treat your diabetes by eating well and moving more.
How does insulin work on a cellular and molecular level?
A Molecular Messenger Insulin is made in the pancreas and added to the blood after meals when sugar levels are high. This signal then spreads throughout the body, binding to insulin receptors on the surface of liver, muscle and fat cells.
What is diabetes on a cellular level?
In individuals with type 1 diabetes, the body mistakenly attacks insulin-producing cells and destroys them. This leaves the body unable to regulate the amount of sugar in the blood or shift the sugar into cells that convert it into energy.
What molecules are affected by diabetes?
The majority of the diabetic population is affected by type 2 diabetes. Currently, hyperglycemia is treated by a broad range of molecules such as biguanides, sulfonylurea, insulin, thiazolidinediones, incretin mimetics, and DPP-4 inhibitors exerting different mechanisms.
How is type 1 diabetes permanently treated?
Currently, there is no cure for type 1 diabetes. Insulin injection is the only medication; however, it accompanies serious medical complications. Current strategies to cure type 1 diabetes include immunotherapy, replacement therapy, and combination therapy.
What treatment do you need for type 1 diabetes?
Anyone who has type 1 diabetes needs lifelong insulin therapy. Types of insulin are many and include: Short-acting (regular) insulin. Rapid-acting insulin.
What happens to a type 1 diabetes without insulin?
Without insulin, your body will break down its own fat and muscle, resulting in weight loss. This can lead to a serious short-term condition called diabetic ketoacidosis. This is when the bloodstream becomes acidic, you develop dangerous levels of ketones in your blood stream and become severely dehydrated.
How does type 1 diabetes affect insulin and blood glucose levels?
If you have type 1 diabetes, your pancreas doesn't secrete insulin — which causes a buildup of glucose in your bloodstream. Without insulin, the glucose can't get into your cells. If you have type 2 diabetes, your pancreas secretes less insulin than your body requires because your body is resistant to its effect.
What effect does insulin have on blood glucose level?
Insulin helps keep the glucose in your blood within a normal range. It does this by taking glucose out of your bloodstream and moving it into cells throughout your body. The cells then use the glucose for energy and store the excess in your liver, muscles, and fat tissue.
How does insulin work for diabetics?
Insulin helps blood sugar enter the body's cells so it can be used for energy. Insulin also signals the liver to store blood sugar for later use. Blood sugar enters cells, and levels in the bloodstream decrease, signaling insulin to decrease too.
What is the pathophysiology of diabetes mellitus?
Type 1 diabetes mellitus (T1DM) is a disease where destruction of the insulin producing pancreatic beta-cells leads to increased blood sugar levels. Both genetic and environmental factors play a part in the development of T1DM.
What are the factors that contribute to T1DM?
Both genetic and environmental factors play a part in the development of T1DM. Currently, numerous loci are specified to be the responsible genetic fac …. Type 1 diabetes mellitus (T1DM) is a disease where destruction of the insulin producing pancreatic beta-cells leads to increased blood sugar levels. Both genetic and environmental factors play ...
What happens when you have type 1 diabetes?
In individuals with type 1 diabetes, the body mistakenly attacks insulin-producing cells and destroys them. This leaves the body unable to regulate the amount of sugar in the blood or shift the sugar into cells that convert it into energy. Uncontrolled blood sugar can take a toll on the body damaging the kidneys and heart ...
How much does the Diabetes Research Connection give?
The Diabetes Research Connection supports early career scientists with up to $50,000 in funding for research on type 1 diabetes.
Can diabetes cause kidney damage?
Uncontrolled blood sugar can take a toll on the body damaging the kidneys and heart and leading to other complications. Individuals with type 1 diabetes must take care to monitor their own blood sugar and administer the correct amount of insulin to make up for the work that would normally be done by the pancreatic cells.
Can pluripotent stem cells be used as pancreatic islet cells?
The researchers want to use the body’s own pluri potent stem cells and turn them into pancreatic islet cells . To do this, they must determine exactly how to manipulate the cells to get them to transform into the islet cells needed by the body.
What are the mechanisms of the susceptible genes in type 1 diabetes?
The mechanisms of the susceptible genes in type 1 diabetes may relate to their respective roles in antigen presentation, beta cell autoimmunity, immune tolerance, and autoreactive T cell response. Environmental susceptibility factors also contribute to the risk of developing type 1 diabetes.
What is autoimmune type 1 diabetes?
Autoimmune type 1 diabetes is characterized by selective destruction of insulin-secreting beta cells in the pancreas of genetically susceptible individuals. The mechanisms underlying the development of type 1 diabetes are not fully understood. However, a widely accepted point is that type 1 diabetes is caused by a combination ...
Is type 1 diabetes genetically susceptible?
However, a widely accepted point is that type 1 diabetes …. Autoimmune type 1 diabetes is characterized by selective destruction of insulin-secreting beta cells in the pancreas of genetically susceptible individuals. The mechanisms underlying the development of type 1 diabetes are not fully understood. However, a widely accepted point is that type ...
What are the factors that affect the development of type 1 diabetes?
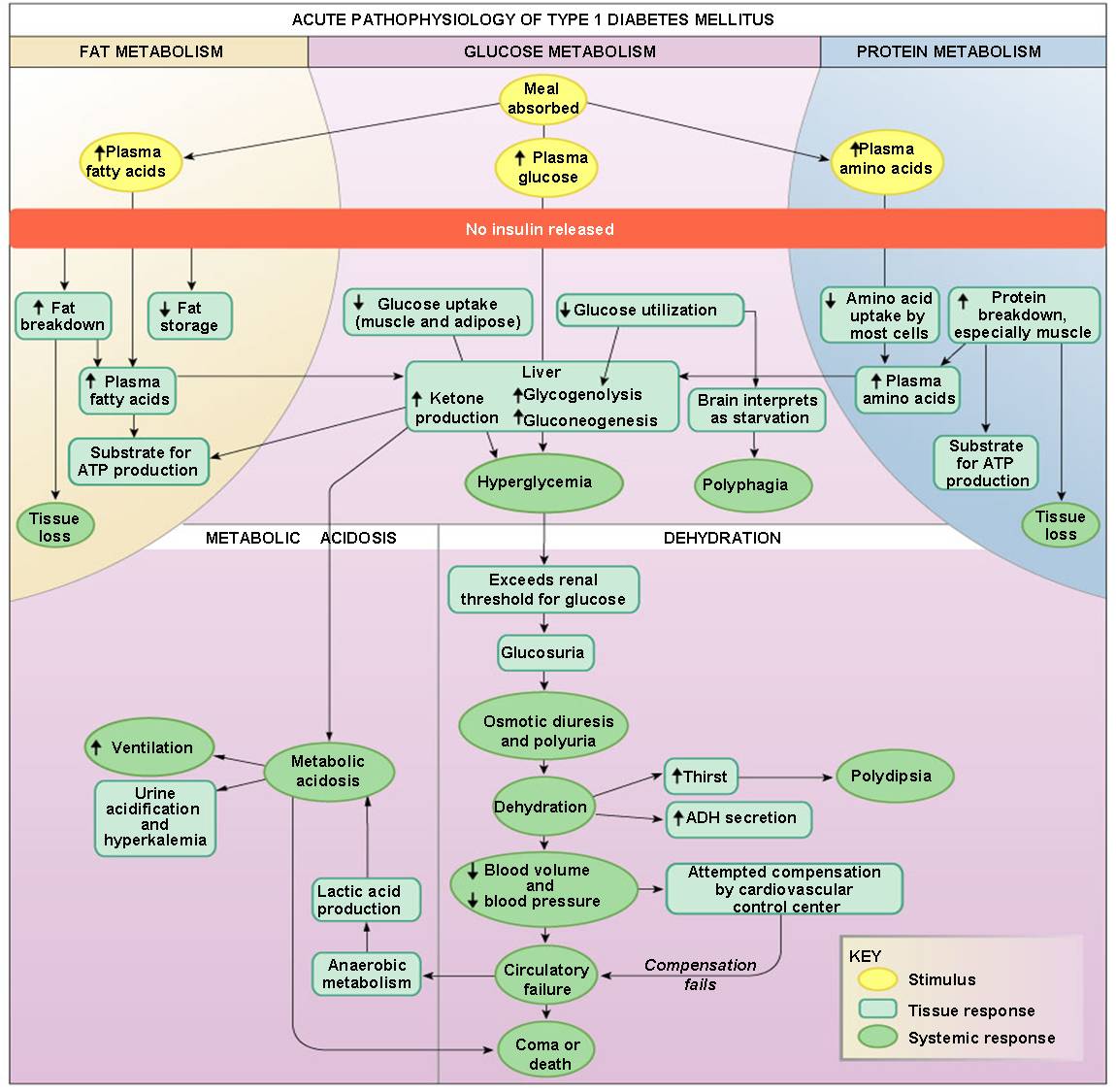
Go to: Abstract Type 1 diabetes is a T cell mediated autoimmune disease, characterised by the selective destruction of pancreatic β cells, and susceptibility is determined by a combination of genetic and environmental factors . The environmental agents implicated include viruses and dietary factors, although none has yet been shown to be directly responsible for triggering β cell autoimmunity. The genetic factors that influence disease risk have been subjected to more intensive study and two gene regions of major importance have been identified: the human leucocyte antigen locus and the insulin gene. This review will focus on the mechanisms by which these genes might influence the risk of developing type 1 diabetes. Keywords: type 1 diabetes, HLA molecules, molecular mechanisms Type 1 diabetes is a multifactorial autoimmune disease, which is characterised by T cell mediated destruction of the insulin secreting β cells of the islets of Langerhans in the pancreas. The destructive process leads to severe insulin depletion, which results in hyperglycaemia, because of hepatic overproduction of glucose by glycogenolysis and gluconeogenesis and decreased cellular uptake of glucose from the circulation. In the absence of insulin, there is also an increase in fat breakdown and fatty acid oxidation, resulting in the excessive production of ketones. If left untreated, these metabolic disturbances lead progressively to central nervous system depression, coma, and death. Therefore, the disease requires life long treatment with exogenous insulin for survival. The rate of β cell destruction varies from patient to patient, but tends to be more aggressive in infants and young children.1 Hence, type 1 diabetes usually presents during childhood or adolescence, although it may develop m Continue reading >>
What are the causes of type 1 diabetes?
Type 1 diabetes causes Type 1 diabetes is believed to be due to an autoimmune process, in which the body's immune system mistakenly targets its own tissues (islet cells in the pancreas). In people with type 1 diabetes, the beta cells of the pancreas that are responsible for insulin production are attacked by the misdirected immune system. This tendency for the immune system to destroy the beta cells of the pancreas is likely to be, at least in part, genetically inherited, although the exact reasons that this process happens are not fully understood. Exposure to certain viral infections (mumps and Coxsackie viruses) or other environmental toxins have been suggested as possible reasons why the abnormal antibody responses develop that cause damage to the pancreas cells. The primary problem in type 2 diabetes is the inability of the body's cells to use insulin properly and efficiently, leading to hyperglycemia (high blood sugar) and diabetes. This problem affects mostly the cells of muscle and fat tissues, and results in a condition known as insulin resistance. In type 2 diabetes, there also is a steady decline of beta cells that worsens the process of elevated blood sugars. At the beginning, if someone is resistant to insulin, the body can at least partially increase production of insulin enough to overcome the level of resistance. Over time, if production decreases and enough insulin cannot be released, blood sugar levels rise. In many cases this actually means the pancreas produces larger than normal quantities of insulin, but the body is not able to use it effectively. A major feature of type 2 diabetes is a lack of sensitivity to insulin by the ce Continue reading >>
What is the historical model of diabetes?
As a result of this work, the majority of current conventional wisdom portrays type 1 diabetes as a T cell–mediated autoimmune disease involving the specific destruction of insulin-producing pancreatic β-cells. In this model, persons destined to develop type 1 diabetes are assumed to begin life with a full cadre of β-cells. However, a “triggering” insult, likely environmental, initiates a process involving the recruitment of antigen-presenting cells. Antigen-presenting cells sequester self-antigens released by injured β-cells, followed by their transport to pancreatic lymph nodes where they are subsequently presented to autoreactive T cells. These T cells, rogue constituents brought to life due to genetically driven failures of thymic deletion (i.e., central tolerance) combined with defects in mechanisms designed to induce peripheral immune tolerance, come into play (3). This toxic duo, imparting lack-of-tolerance formation, again in the context of genetic susceptibility, allows for migration of self-reactive T cells to islets, mediating β-cell killing and promoting further inflammation (4). When 85–90% of pancreatic β-cells meet their demise, symptoms of the disease occur. In the final stage of the model, the autoimmune process ends with the complete elimination of β-cells. While this concept still forms the prevailing intellectual dogma for the majority of individuals associated with Continue reading >>
What causes diabetes in the pancreas?
The root cause of Type 1 Diabetes is the autoimmune action of cytotoxic T cells on the beta cells of pancreatic islets , which the T cells incorrectly recognize as foreign and thus carry out their destruction (4). These cells are vital to the body’s production of the peptide hormone insulin, which is the major modulator of the uptake of glucose in cells. Without adequate ability to produce insulin, the body suffers from the effects of an imbalanced glycemia, thus bringing forth the signs, symptoms, and effects attributed to Type 1 Diabetes (5). A complex formed by a genetically affected form of the Major Histocompatibility Complex Class II protein (MHCII) and a posttranslationally modified Glutamate Dehydrogenase 65 (GAD65) acts as the autoantigen recognized by the T-cell receptor as foreign, thus triggering the cytotoxic response and destruction of pancreatic beta cells (6) (7). On a biochemical and molecular level, the gene responsible for the coding and expression of MHCII is referred to as the HLA gene, and it is the allelic haplotype forms of this gene HLA-DQ and HLA-DR that have a strong correlation with Type 1 Diabetes (8), and individuals that harbor these HLA haplotypes are considered to be at high risk of developing the disease (9). Also included in this site are summaries of two recent studies in the field of Type 1 Diabetes research, one that explores the quality of register binding that triggers the autoimmune attack by T-cells on pancreatic beta cells (23) and another that explores an alternate high genetic risk factor for Type 1 Diabetes (25), outlining current research focuses and methods pertaining to the disease. Also, a summary of some experimental methods common to Type 1 Diabetes medical research has been included as well. Continue reading >>
Insulin Dependent Diabetes Mellitus (type I Diabetes)
The root cause of Type 1 Diabetes is the autoimmune action of cytotoxic T cells on the beta cells of pancreatic islets, which the T cells incorrectly recognize as foreign and thus carry out their destruction (4).
Diabetes: Mechanism, Pathophysiology And Management-a Review
Anees A Siddiqui1*, Shadab A Siddiqui2, Suhail Ahmad, Seemi Siddiqui3, Iftikhar Ahsan1, Kapendra Sahu1 Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Jamia Hamdard (Hamdard University), Hamdard Nagar, New Delhi (INDIA)-110062. School of Pharmacy, KIET, Ghaziabad U.P.
On Type 1 Diabetes Mellitus Pathogenesis
Division of Endocrinology, Metabolism and Diabetes, First Department of Pediatrics, Aghia Sophia Childrens Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece Correspondence should be addressed to C Kanaka-Gantenbein: chriskan {at}med.uoa.gr Type 1 diabetes mellitus (T1DM) results from the autoimmune destruction of cells of the endocrine pancreas.
The Pathogenesis And Natural History Of Type 1 Diabetes
Abstract The purpose of this article is to provide an overview that summarizes much in the way of our current state of knowledge regarding the pathogenesis and natural history of type 1 diabetes in humans.
Molecular Mechanism Of Insulin Resistance In Type 2 Diabetes Mellitus: Role Of The Insulin Receptor Variant Forms
Molecular mechanism of insulin resistance in type 2 diabetes mellitus: role of the insulin receptor variant forms University of CatanzaroMagna, Graecia, Italy c/o Dipartimento di Medicina Interna, Universit di Roma Tor Vergata, Via Tor Vergata 135, 00133 Rome, Italy.
Molecular Mechanisms In Autoimmune Type 1 Diabetes: A Critical Review
1. Clin Rev Allergy Immunol. 2014 Oct;47 (2):174-92. doi: 10.1007/s12016-014-8422-2. Molecular mechanisms in autoimmune type 1 diabetes: a critical review.
Molecular Mechanism Of A Diabetes Vaccine Revealed
Follow all of ScienceDaily's latest research news and top science headlines ! Molecular Mechanism Of A Diabetes Vaccine Revealed A team of researchers led by Prof. Irun Cohen of the Weizmann Institute of Science Immunology Department has revealed the molecular mechanism of a vaccine for Type 1 diabetes.
Why does fasting hyperglycemia occur in type 2 diabetics?
The fasting hyperglycemia in patients with type 2 diabetes is the clinical correlate of the increased glucose production by the liver because of insulin resistance. This is the result of the lack of inhibition of the two key gluconeogenic enzymes, PEPCK and the glucose-6-phosphatase (G6Pase) catalytic subunit.
What is the main pathophysiological event contributing to the development of type 2 DM?
Besides β cell failure, the major pathophysiological event contributing to the development of type 2 DM is the resistance of target tissues to insulin, which is usually associated with abnormal insulin secretion.
What are the mutations in IRS-1?
MUTATIONS IN IRS PROTEINS. In humans, rare mutations of the IRS-1 protein are associated with insulin resistance[15]. Disruption of the IRS-1gene in mice results in insulin resistance, mainly of muscle and fat[16]. Interesting results are obtained by studying IRs in knockout mice.
What is the role of free fatty acids in diabetes?
Free fatty acids are known to play a key role in promoting loss of insulin sensitivity in type 2 diabetes mellitus but the underlying mechanism is still unclear. It has been postulated that an increase in the intracellular concentration of fatty acid metabolites activates a serine kinase cascade, which leads to defects in insulin signaling ...
What is the role of leptin in the body?
The role of leptin in regulating food intake and energy expenditure is well established. Humans with leptin deficiency or leptin receptor mutations are severely obese[83,84]. In addition, it has direct effects on insulin sensitivity and may also reverse insulin resistance in mice with congenital lipodystrophy[85].
What are the substrates of PDKs?
Known substrates of the PDKs are the protein kinase B (PKB) and also atypical forms of the protein kinase C (PKC)[8]. PKB. Downstream from PI3-kinase, the serine/threonine kinase Akt (also called PKB), triggers insulin effects on the liver, such as glycogen synthesis and the suppression of hepatic glucose production.
What is the IR in insulin?
NORMAL INSULIN SIGNALING. The insulin receptor (IR) is a heterotetramer consisting of two α subunits and two β subunits that are linked by disulphide bonds. Insulin binds to the α subunit of the insulin receptor and activates the tyrosine kinase in the β subunit.