What is the maximum dosage for metoprolol?
metoprolol (see dosing suggestions to right). If HR > 120 after 15 mg IV metoprolol, consider an alternate agent such as diltiazem above. Oral dosing: If HR < 120 after 5 mg IV, consider oral dose of 25 mg PO BID. If HR < 120 after 10 mg IV, consider oral dose of 50 mg PO BID. If HR < 120 after 15 mg IV, consider oral dose of 75 mg PO BID.
How much diltiazem should I take for AFIB?
Usually instability with atrial fibrillation is caused by a rapid heart rate. Typically, you can apply some type of rate control medicaton like cardizem or metoprolol to bring the heart rate down. There are a lot of variables and a lot of options and cardioversion for unstable atrial fibrillation without an TEE would be the last option. Regards ...
How much dosage of metoprolol can be fatal?
0.005 mg/kg per min. Avoid in hypotension, heart failure, cardiomyopathy, acute and coronary syndromes. β-Adrenergic Blockers. Metoprolol. 2.5-5 mg over 2 min, up to 3 doses. Avoid in decompensated heart failure. Esmolol. 500 μg/kg IV over 1 min. 50–300 μg/kg per min.
What is the best medication for atrial fibrillation?
Amiodarone: There are a number of schemes to load but to obtain levels one uses 800 mg for 5 day, 600 mg for 5 days, and 400 mg maintenance for 3-6 months and the... Read More. 1.8k views Reviewed >2 years ago. Thank.
What to do after 15 mg of metoprolol?
If HR < 120 results, start oral metoprolol (see dosing suggestions to right). If HR > 120 after 15 mg IV metoprolol, consider an alternate agent such as diltiazem above.
How common is atrial fibrillation?
The cost of direct care of patients with AF in the U.S. is an estimated $6.65 billion annually, the majority of which is attributed to hospitalizations due to rapid ventricular response, heart failure, and stroke. There are 150 admissions to the over UMHS annually with principle the diagnosis of -onset new AF, and there are many more than that for recurrent or chronic atrial fibrillation.
Is loading propranolol necessary?
N/A Loading doses are not necessary due to rapid onset of action Propranolol Consider for use in thyrotoxicosis [Class I, LOE C]
What is the best medicine for decompensated systolic heart failure?
For patients with decompensated systolic heart failure: Consult cardiology, and consider digoxin or amiodarone for rate control.
Can you combine IV beta blockers?
Also, IV calcium channel blockers and IV beta blockers are not usually combined- if one is not effective, change to the other.
Is AFL asymptomatic or asymptomatic?
While AF may be asymptomatic and found incidentally, AFL is usually highly symptomatic.
Can AF/AFL be recurrence?
AF/AFL that occurs in the postoperative setting requires special consideration. Possible etiologies for postoperative AF/AFL should be considered based on the type of operation performed and potential perioperative events/complications. Many patients with postoperative AF/AFL will spontaneously convert back to sinus rhythm, and many of those patients will never have a recurrence of atrial fibrillation again. Therefore, postoperative AF/AFL is often treated with a rhythm control strategy. However, a subgroup of patients who suffer from postop AF/AFL will be found to have underlying heart disease, and go on to have recurrences. The optimal clinical approach to a patient with postoperative AF/AFL is not certain, but general recommendations will be provided in this section.
How long should you be anticoagulated for atrial fibrillation?
Patients who have been in atrial fibrillation for longer than 48 hours should be anticoagulated before being cardioverted to prevent clots from the atria from traveling through the bloodstream, where they may cause a heart attack, stroke, or pulmonary embolism.
What is the goal of atrial fibrillation treatment?
The goal of atrial fibrillation treatment is three-fold: to control the rate, to control the rhythm, and to prevent stroke.
What is it called when your heart beats 100 beats per minute?
When the heart rate is greater than 100 beats per minute, it is referred to as an uncontrolled ventricular response . Patients will often experience untoward symptoms at 150 beats per minute and higher, but some patients may experience symptoms at a lower rate.
Is ablation better than cardioversion?
Ablation is often more successful than cardioversion. (This article barely reviews the basics of AF and its causes and treatments. For a thorough study of AF and current treatment modalities, obtain a copy of the “2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS.”)
How to convert AF?
Besides medication, other measures can be taken to convert AF. One of these methods is synchronized cardioversion. By administering a shock, the hope is that the SA node will reassert itself and the patient will convert into a normal sinus rhythm. Patients will require sedation, as cardioversion is quite painful. Patients who have been in atrial fibrillation for longer than 48 hours should be anticoagulated before being cardioverted to prevent clots from the atria from traveling through the bloodstream, where they may cause a heart attack, stroke, or pulmonary embolism. Sometimes the effects of cardioversion are short-lived, in which case ablation may be an option.
How to maintain AF?
AF can be maintained by reentry and/or rapid focal ectopic firing. 8 The irregular atrial discharge typical of AF may result from an irregular atrial response to a rapidly discharging regularly firing driver (mechanism causing AF) resulting from either local ectopic firing or a single localized reentry circuit. 5
What happens to the blood vessels in the AV node?
At the AV node and beyond into the ventricles, the electrical impulse signals the ventricles to contract, and blood is pumped out of the ventricles to the body. In atrial fibrillation, the rapid and chaotic firing of multiple cells in the atria bombards the AV node with impulses, only some of which get through to signal the ventricles to contract.
When should I perform cardioversion of stable atrial fibrillation?
Cardioversion of stable atrial fibrillation should be performed with caution if the arrhythmia is more than 48 hours old and no anticoagulant therapy has been initiated due to the risk of emboli that can cause MI and stroke.
What is the best indicator of atrial fibrillation?
When the heart rate is extremely rapid, it may be difficult to determine if the rate is irregular, and the absence of p-waves will be the best indicator of atrial fibrillation.
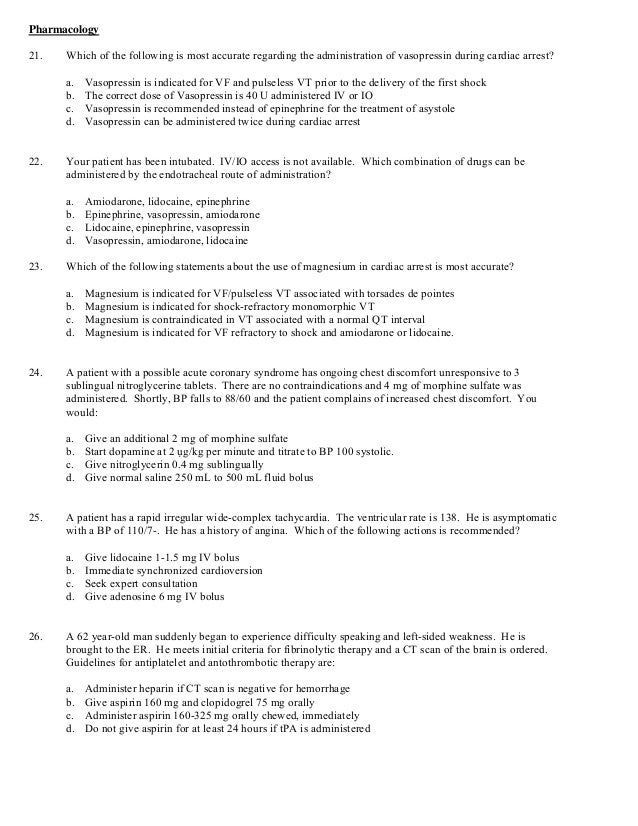
What voltage is needed for unstable tachycardia?
Drugs are not used to manage unstable tachycardia. The appropriate voltage for cardioverting unstable atrial fibrillation is 120-200 J.
What is the problem with atrial fibrillation?
For ACLS, atrial fibrillation becomes a problem when the fibrillation produces a rapid heart rate which reduces cardiac output and causes symptoms or an unstable condition.
What is the most common cardiac arrhythmia?
The most common cardiac arrhythmia, atrial fibrillation, occurs when the normal electrical impulses that are generated by the SA node are overwhelmed by disorganized electrical impulses in the atria. These disorganized impulses cause the muscles of the upper chambers of the heart to quiver (fibrillate) and this leads to the conduction ...
Can calcium channel blockers help with ventricular rate?
Q: To treat a patient with rapid atrial fibrillation (HR >180bpm), can calcium channel blockers be given to help control the rate? A: Yes, in some cases, calcium channel blockers are a good choice to help control atrial fibrillation with a rapid ventricular rate.
How many times a day can you give a titration?
Twice: But can be given 3 times a daily in specific circumstances. Titration should be done carefully with the help of a cardiologist experienced in using fl ... Read More
Is dilantin safe for atrial fibrillation?
Another medication to consider is dilantin. Dilantin is very safe, and is an effective anti-arrhythmic. See book by jack dreyfus.
Can you adjust metoprolol?
Adjust Metoprolol: Most antihypertensives may be used. However, my first choice is to adjust the dose of metoprolol. Rate control is more important than rhythm control... Read More
What is the most commonly used medication in the ACLS and PALS algorithms?
Adenosine. Adenosine is one of the most commonly used medications in the ACLS and PALS algorithms. It is an antiarrhythmic medication used to treat various forms of supraventricular tachycardia after vegal maneuvers have failed. The delivery of adenosine in ACLS and PALS causes a transient heart block in the atrioventricular (AV) node.
What is the best medication for cardiac arrhythmias?
Amiodarone is most commonly used to treat arrhythmias during emergency cardiac events. It is also commonly proscribed and used to prevent life-threatening cardiac arrhythmias in patients that have a chronic risk of developing such arrhythmias.
What causes a transient heart block in the atrioventricular node?
The delivery of adenosine in ACLS and PALS causes a transient heart block in the atrioventricular (AV) node. This is due to α 1 receptor inhibition of adenylyl cyclase. As a result there is a reduction of cAMP that leads to the hyperpolarization of the cells.
Is sotalol a beta blocker?
Sotalol is a non-selective beta blocker that also includes class III antiarrhythmic activity. It prolongs the refractory period and increases the action potential duration of the cardiac muscle. Sotalol is only recommended by the Food and Drug Administration (FDA) for serious life threatening arrhythmias because of its potential to develop a prolongation in the QT interval which increases the risk of torsades de point development.
What is the most common medication used during emergency treatment?
Epinephrine is one of the most common drugs used during emergency treatment when performing ACLS ( Advanced Cardiac Life Support) and PALS (Pediatric Advanced Life Support). It is used during ACLS and PALS because it has a wide range of indications.
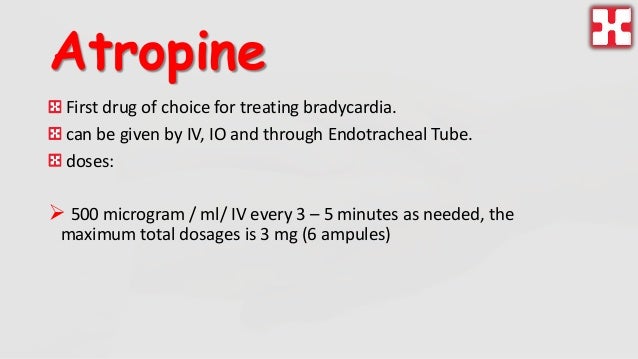
What is atropine used for?
Atropine is commonly used as a treatment for bradycardia (HR<60bpm). It was previously used in the ACLS algorithm for cardiac arrest, asystole, and PEA but had later been removed to treat these arrhythmias because of lack of evidence showing that it was effective in converting the rhythms. Atropine has proven effective in treating the arrhythmia second-degree heart block Mobitz type 1. It has also been effective against third-degree heart block but only in those with an AV-node escape rhythm. Atropine has also been known to treat a bradycardic response to intubation in children.
Is amiodarone used for ventricular fibrillation?
Cardiac Arrest: While the first line treatment for cardiac arrest resulting from ventricular fibrillation and ventricular tachycardia is defibrillation, amiodarone has been used as a second line drug therapy , after epinephrine, to treat shock-refractory ventricular fibrillation.