Treatment DSM-5 Criteria for Posttraumatic Stress Disorder (PTSD) Updated 2019 DSM 5 PTSD A.Exposure to actual or threatened death, serious injury, or sexual violence in one (or more) of the following ways: 1. Directly experiencing the traumatic event(s). 2. Witnessing, in person, the event(s) as it occurred to others. 3.
Full Answer
What are the DSM 5 criteria?
- Taking the substance in larger amounts or for longer than you're meant to.
- Wanting to cut down or stop using the substance but not managing to.
- Spending a lot of time getting, using, or recovering from use of the substance.
- Cravings and urges to use the substance.
- Not managing to do what you should at work, home, or school because of substance use.
What kind of doctor should I See for PTSD?
You must have experienced at least one of these things in the following ways:
- First-hand experience
- Witnessing the event
- Learning that a close friend or relative experienced it or was threatened
- You’re regularly exposed to other people’s trauma, maybe for your job
What is the DSM5 diagnosis of PTSD?
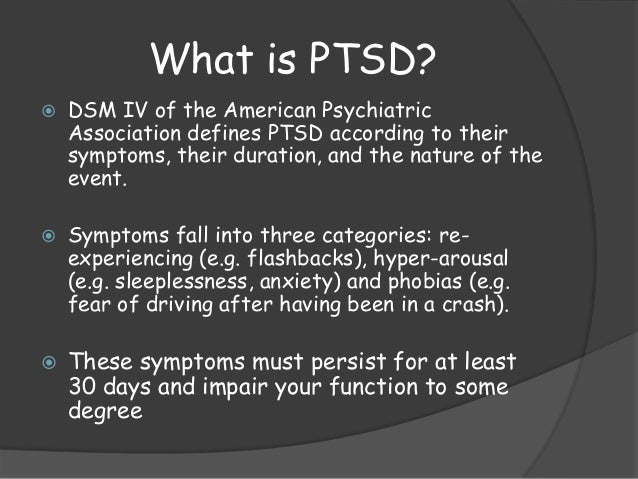
Under DSM-5, post-traumatic stress disorder (PTSD) is an anxiety disorder that develops in relation to an event which creates psychological trauma in response to actual or threatened death, serious injury, or sexual violation.
When was PTSD added to the DSM?
posttraumatic stress disorder first became the diagnosis we know today in 1980, when it was included in the anxiety disorders section of the dsm-iii psychiatric manual. [3], [7] before 1980, posttraumatic stress was described and diagnosed under a variety of different names in both medical literature, and the icd-6 (1948) and dsm-i (1952) …

What does the DSM say about PTSD?
What is the DSM-5 criteria for PTSD? The DSM-5 criteria for PTSD include, first, direct or indirect exposure to a traumatic event, followed by symptoms in four categories: intrusion, avoidance, negative changes in thoughts and mood, and changes in arousal and reactivity.
What are the DSM-5 specifiers for PTSD?
DSM-5 recognizes a “with dissociative symptom” specifier when the PTSD symptoms are accompanied by persistent or recurrent depersonalization or derealization. The specifier “with delayed expression” should be included if the full criteria for PTSD are not met for more than 6 months following the trauma.
What is the proper treatment for PTSD?
For PTSD, cognitive therapy often is used along with exposure therapy. Exposure therapy. This behavioral therapy helps you safely face both situations and memories that you find frightening so that you can learn to cope with them effectively. Exposure therapy can be particularly helpful for flashbacks and nightmares.
Is PTSD a DSM-5 diagnosis?
In 2013, the American Psychiatric Association revised the PTSD diagnostic criteria in the fifth edition of its Diagnostic and Statistical Manual of Mental Disorders (DSM-5; 1). PTSD is included in a new category in DSM-5, Trauma- and Stressor-Related Disorders.
What is the DSM-5 criteria?
The DSM-5 is a tool and reference guide for mental health clinicians to diagnose, classify, and identify mental health conditions. It now lists 157 mental disorders with symptoms, criteria, risk factors, culture and gender-related features, and other important diagnostic information.
Why is PTSD not in the DSM?
A DSM-IV/DSM-5 comparison study conducted by Kilpatrick and colleagues [20] using highly structured self-report inventories demonstrated that 60% of PTSD cases that met DSM-IV but not proposed DSM-5 PTSD criteria were excluded from the DSM-5 because the traumatic events involved only nonviolent deaths.
What are 3 treatments for PTSD?
What Are the Treatments for PTSD?Therapy.Cognitive Processing Therapy.Prolonged Exposure Therapy.Eye Movement Desensitization and Reprocessing.Stress Inoculation Training.Medications.
Is medication or therapy better for PTSD?
Most guidelines for the treatment of PTSD in adults recommend that trauma-focused psychotherapy be used as a first-line treatment and medications be used as a second-line treatment, Sonis said. In other words, they recommend that psychotherapy should be offered, preferentially, to adults with PTSD, over medication.
What is the best medication for complex PTSD?
What are the best medications to treat PTSD?Sertraline (Zoloft) is FDA-approved for treating PTSD, and it's one of the most common medications prescribed for this condition. ... Paroxetine (Paxil) is the only other FDA-approved medication for PTSD. ... Fluoxetine (Prozac) is used off-label for treating PTSD.More items...•
What are the ICD 11 PTSD diagnostic criteria?
The proposed ICD-11 template comprises, therefore, six disorder-defining criteria: dissociative flashbacks, nightmares, hypervigilance, exaggerated startle response, avoidance of external reminders, and avoidance of thoughts and feelings associated with the traumatic event.
What three criteria must be met to confirm the diagnosis of PTSD?
Persistent, distorted cognitions about the cause or consequences of the traumatic event(s) that lead the individual to blame himself/herself or others. Persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame). Markedly diminished interest or participation in significant activities.
Is PTSD an anxiety disorder DSM-5?
Posttraumatic stress disorder (PTSD) is now in a separate chapter in DSM-5 on Trauma- and Stressor-Related Disorders. This move from DSM-IV, which addressed PTSD as an anxiety disorder, is among several changes approved for this condition that is increasingly at the center of public as well as professional discussion.
What does PTSD stand for in the DSM?
What is PTSD? Before diving into the DSM criteria for PTSD, here are the basics of what PTSD is. PTSD stands for post-traumatic stress disorder. It is commonly associated with veterans. However, as you will learn in the remainder of this article, PTSD can be diagnosed in anyone that meets the criteria.
What is the DSM?
The DSM includes lists of symptoms and criteria that they can use in order to diagnose patients with mental disorders. This guidebook helps to make diagnosis and communication about mental illness more consistent.
What changes were made to the DSM-5?
As you can see, there were important changes made to the DSM-5 regarding mental health disorders in order to help treat patients more effectively. One of the changes made in the most recent edition was moving PTSD from the section on Anxiety Disorders to a new chapter on Trauma- and Stress- or- Related Disorders.
What does DSM mean?
DSM stands for Diagnostic and Statistical Manual of Mental Disorders. It's a book that is basically like an encyclopedia of mental health conditions. The book originally was published in 1952, but has been updated multiple times resulting in the current edition of the DSM-5.
Why was the DSM created?
The purpose of creating the DSM is to provide a handbook for mental health professionals and other healthcare workers.
How does exposure therapy work for PTSD?
Exposure Therapy works by exposing people with PTSD to the thing that caused their trauma.
What are the symptoms of a traumatic event?
Before someone can be diagnosed, they need to be re-experiencing the event on an on-going basis. This doesn't mean that they need to be living through the same thing over and over again, but experiencing it through one of the following: 1 Nightmares 2 Flashbacks 3 Involuntary memories 4 Emotional distress after being reminded of the trauma 5 A physical reaction after being reminded of the trauma
What is PTSD in DSM-5?
Under DSM-5, post-traumatic stress disorder (PTSD) is an anxiety disorder that develops in relation to an event which creates psychological trauma in response to actual or threatened death, serious injury, or sexual violation . The exposure must involve directly experiencing the event, witnessing the event in person, ...
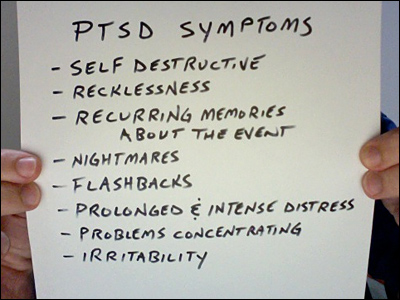
What are the symptoms of PTSD?
Under DSM-5, for those older than six years of age, PTSD includes four clusters of symptoms (APA, 2013): 1 Re-experiencing the event — Recurrent memories of the event, traumatic nightmares, dissociative reactions, prolonged psychological distress 2 Alterations in arousal — Aggressive, reckless or self-destructive behavior, sleep disturbances, hypervigilance 3 Avoidance — Distressing memories, thoughts, or reminders of the event. 4 Negative alterations in cognition and mood — Persistent negative beliefs, distorted blame, or trauma-related emotions; feelings of alienation and diminished interest in life
What are the two subtypes of PTSD?
In addition, the disturbance cannot be attributed to a substance or medical condition. DSM-5 has established two subtypes of PTSD: 1. PTSD Preschool subtype is used in the diagnosis of children younger than 6 years of age. The diagnostic thresholds are lowered for children and adolescents. 2.
What is the dissociative subtype of PTSD?
PTSD Dissociative Subtype is used when the person has prominent dissociative symptoms. These dissociative symptoms include depersonalization, in which the person feels like an outside observer or detached from oneself; and derealisation, in which the world seems unreal, distant or distorted.
What is the DSM 5?
DSM-5 has made a number of important changes to the criteria of post-traumatic stress disorder, the most significant being a more specific definition of the type and nature of the exposure to a threat. Under DSM-5, post-traumatic stress disorder (PTSD) is an anxiety disorder that develops in relation to an event which creates psychological trauma ...
How does post traumatic stress disorder affect daily life?
Post-traumatic stress disorder causes impairments in daily life through the persistent re-experiencing of the negative event via recollections such as intrusive negative thoughts and dreams, flashbacks, and dissociative states. Under DSM-5, emotional reactions to the traumatic event such as fear and helplessness are no longer part ...
Is PTSD a high risk profession?
PTSD is associated with “high-risk” professions such as the military, policing, firefighting and emergency medical work. PTSD has significantly limited daily functioning in those exposed to extreme and prolonged trauma such as war veterans. Depression is a common experience of war veterans with PTSD.
Prevalence of PTSD
Within the general US population, the DSM-5 estimates the projected lifetime risk for PTSD using DSM-4 criteria at age 75 years is 8.7%, though rates are higher for those in professions that increase their exposure to traumatic events, like veterans.
Suicide Risk and Comorbidities
Traumatic events increase a person’s suicide risk, and PTSD is strongly associated with suicidal ideation and suicidal attempts.
Resources and Assistance with VA Claims
Veterans have played an outsized role in spreading awareness of PTSD, especially following the recent wars in Afghanistan in Iraq.
What are the symptoms of PTSD?
1 The argument for inclusion was that many sufferers of trauma and chronic trauma do not experience the standard symptoms of PTSD but rather symptoms of depression, anxiety, or dissociation, or of borderline personality disorder. The authors of DSM-5 have handled this issue in a curious manner. 2 To begin with, they eliminated criterion A2, which included the words “. . . response involved intense fear, helplessness, or horror,” explaining that “Emotional reactions to the traumatic event (eg, fear, helplessness, horror) are no longer a part of criterion A. The clinical presentation of PTSD varies.” 3 The new criterion A does not, however, describe other possible reactions.
What is the DSM-5 coding change?
What about the diagnostic criteria? By way of difference, DSM-5 specifies that the criteria apply to adults and children over age 6 (and includes another set of criteria for children under 6); eliminates the immediate response to the trauma as involving fear, helplessness, or horror; and splits the avoidance symptoms into 2 clusters (ie, distressing memories and external reminders). In addition to these changes, virtually all the symptoms of each cluster are elaborated or written differently, and for each cluster extra symptoms are added. More about this later.
Does DSM-5 change PTSD?
Thus, as with complex PTSD, DSM-5 has not significantly changed the problems with PTSD that beset DSM-IV.
Does the DSM 5 have cultural variation?
While this subsection does recognize cultural variation, and while DSM-5 also has an entire section III dedicated to “cultural formulation,” these commentaries do not alter the core diagnostic criteria of PTSD, which continue to convey the sense of a universal response to trauma.
Does PTSD have anxiety?
The main rationale is that PTSD often manifests with non-anxiety symptoms such as dissociative experiences, anger outbursts, and self-destructive behavior. As discussed below, however, patients with “complex PTSD” usually experience anxiety along with other symptoms.
What is a traumatic dream?
2. Recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event(s). 3. Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring.
What is persistent avoidance of stimuli associated with the traumatic event(s)?
C.Persistent avoidance of stimuli associated with the traumatic event(s), beginning after the traumatic event(s) occurred, as evidenced by one or both of the following: 1. Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). 2.
What is the definition of traumatic event?
A.Exposure to actual or threatened death, serious injury, or sexual violence in one (or more) of the following ways: 1. Directly experiencing the traumatic event(s). 2. Witnessing, in person, the event(s) as it occurred to others. 3.
How to deal with PTSD?
Helping you think better about yourself, others and the world. Learning ways to cope if any symptoms arise again. Treating other problems often related to traumatic experiences, such as depression, anxiety, or misuse of alcohol or drugs. You don't have to try to handle the burden of PTSD on your own.
What is the best treatment for PTSD?
For PTSD, cognitive therapy often is used along with exposure therapy . Exposure therapy . This behavioral therapy helps you safely face both situations and memories that you find frightening so that you can learn to cope with them effectively. Exposure therapy can be particularly helpful for flashbacks and nightmares.
What is the best medication for PTSD?
They can also help improve sleep problems and concentration. The selective serotonin reuptake inhibitor (SSRI) medications sertraline (Zoloft) and paroxetine (Paxil) are approved by the Food and Drug Administration (FDA) for PTSD treatment.
What type of therapy is used for PTSD?
Some types of psychotherapy used in PTSD treatment include: Cognitive therapy . This type of talk therapy helps you recognize the ways of thinking (cognitive patterns) that are keeping you stuck — for example, negative beliefs about yourself and the risk of traumatic things happening again.
How to diagnose post traumatic stress disorder?
Diagnosis. To diagnose post-traumatic stress disorder, your doctor will likely: Perform a physical exam to check for medical problems that may be causing your symptoms. Do a psychological evaluation that includes a discussion of your signs and symptoms and the event or events that led up to them. Diagnosis of PTSD requires exposure to an event ...
What is the DSM-5?
Use the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. Diagnosis of PTSD requires exposure to an event that involved the actual or possible threat of death, violence or serious injury. Your exposure can happen in one or more of these ways:
How to prepare for a post traumatic stress disorder appointment?
Preparing for your appointment. If you think you may have post-traumatic stress disorder, make an appointment with your doctor or a mental health professional. Here's some information to help you prepare for your appointment, and what to expect. Take a trusted family member or friend along, if possible.
What are the treatment guidelines for PTSD?
A number of psychological treatments for PTSD exist, including trauma-focused interventions and non-trauma-focused interventions. Trauma-focused treatments directly address memories of the traumatic event or thoughts and feeling related to the traumatic event.
What is the APA for PTSD?
In 2017, the Veterans Health Administration and Department of Defense (VA/DoD) and the American Psychological Association (APA) each published treatment guidelines for PTSD, which are a set of recommendations for providers who treat individuals with PTSD.
What is PTSD in medical terms?
Posttraumatic stress disorder (PTSD) is a chronic, often debilitating mental health disorder that may develop after a traumatic life event, such as military combat, natural disaster, sexual assault, or unexpected loss of a loved one .
What is trauma focused CBT?
Trauma-focused CBT typically includes both behavioral techniques, such as exposure, and cognitive techniques, such as cognitive restructuring.
Is PTSD a traumatic stressor?
In the initial formulation of PTSD, a traumatic stressor was defined as an event outside the range of usual human experience.