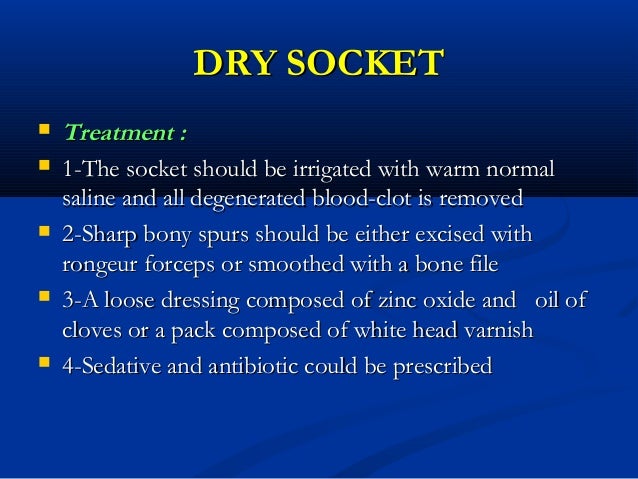
- Flushing out the socket. Flushing out the socket can remove any food particles or other debris that may contribute to pain or possible infection.
- Medicated dressings. Your dentist or oral surgeon may pack the socket with medicated gel or paste and medicated dressings. ...
- Pain medication. ...
- Self-care.
Medication
- Switch to a nicotine patch.
- Wait at least 48 hours after your surgery before smoking.
- Ask your dentist for stitches on your surgery site.
- Keep gauze in place over your socket while smoking.
Procedures
I n most cases, dry socket will heal on its own, but as the site heals patients will likely continue to experience discomfort. If you do choose to treat dry socket at home, you need to clean the wound with cool water, irrigate the socket with saline, and keep gauze over the socket.
Self-care
How to get fast relief from dry socket
- Clove oil. A person may experience dry socket a few days after a tooth extraction. ...
- Salt water. Rinsing the mouth with warm salt water can help reduce bacteria and swelling. ...
- Hot and cold compresses. ...
- Honey. ...
- NSAIDs. ...
- Turmeric. ...
- Green and black teas. ...
- Aloe vera. ...
- Avoid making it worse. ...
- When to see a doctor. ...
Nutrition
Peppermint
- Soak a cotton swab into the water
- Dip it in peppermint oil
- Rub the cotton swab against the site of dry socket
- Leave it on for 10 minutes and wash your mouth with water
- Perform the treatment twice on a daily basis up to 3 days
How long does it take for dry socket to heal?
Can a dry socket heal on its own?
How to heal a dry socket quickly?
What is the best antibiotic for dry socket?
How to treat a dry socket?
What to do if you have a socket that hurts?
How to get rid of a swollen socket?
What to do if you have pain after a tooth extraction?
Can a tooth extraction cause dry socket?
See more
About this website
How does a dentist treat dry socket?
If you have dry socket, your dentist will clean the socket to make sure it's free of food and other particles. This may alleviate any pain and can help prevent infection. Your dentist may also pack the socket with a medicated dressing or paste to help numb the pain.
Can a dry socket heal on its own?
Will a dry socket heal on its own? Yes, in most cases a dry socket will heal on its own. However, because most people experience moderate to severe dry socket pain, seeing your dentist for prompt treatment can help ease discomfort sooner.
How do you treat a dry socket at home?
The Mayo Clinic recommends dissolving ½ teaspoon of salt into 8 ounces of warm water. Swish this around in your mouth for a minute, or use it to flush out the dry socket with a syringe your surgeon gives you. Do this at least three times per day or after meals.
How serious is a dry socket?
Painful, dry socket rarely results in infection or serious complications. However, potential complications may include delayed healing of or infection in the socket or progression to chronic bone infection (osteomyelitis).
Why is the blood clot needed for the healing process?
The clot serves as a protective barrier against bacteria and other types of irritants that may lead to infection. It also plays a crucial role in t...
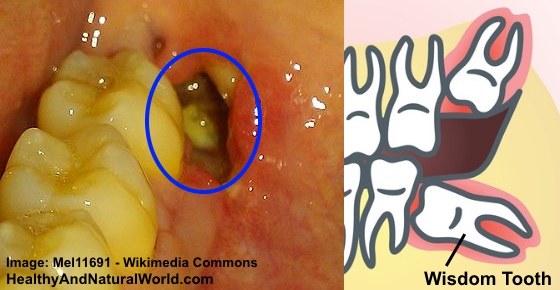
What does a dry socket look like?
If you can see inside the socket, you'll notice that there is no dark, red blood clot. Instead, the tissue inside looks dry and the white bone may...
How long does dry socket take to heal?
Dry socket normally occurs within 3 to 5 days following the extraction. The usual dry socket healing time is 7 days, of which the first 3 days are...
How long should dry socket packing stay in?
If your dentist uses a gel or foam packing which is designed to dissolve by itself, it will stay in for three to five days before starting to lique...
What complications can develop from dry socket?
The most common complication of dry socket is delayed healing. Infections may also occur; however, these might not be strictly associated with alve...
26 Impressive Home Remedies for Dry Socket
Dry socket is one of the most painful dental problems during adulthood. In this article, Authority Remedies will present to you top 26 natural home remedies for dry socket. Overview. You might think that getting a tooth pulled is not an enjoyable experience and you hope not to suffer from some discomfort afterward.
What causes a dry socket?
Dentists do not know what causes dry socket. Risk factors associated with it include: 1 A difficult tooth extraction (removal) 2 Poor oral hygiene 3 Not following mouth care instructions after the tooth is removed 4 Using tobacco products 5 Taking oral contraceptives ( birth control) 6 Drinking through a straw after the tooth is removed
Why is my dry socket so painful?
Dry socket can be painful and make it hard for the area to heal. It happens more often in the lower teeth than those in the top of the mouth. Research shows women are slightly more likely than men to develop dry socket, likely due to estrogen.
How long does it take for a tooth to dry out after a tooth extraction?
Dentists typically suspect dry socket when a person experiences severe pain three days after having a tooth removed. They can confirm the diagnosis simply by looking at the spot where the tooth used to be.
How long does it take for a dry socket to heal?
With proper care, including keeping the socket clean, a dry socket usually heals in seven to 10 days. In that time, new tissue grows and covers the exposed socket. Regular brushing and flossing during this time helps keep the mouth healthy and reduces the risk of infection.
Can dry sockets hurt?
Pain is the most common side effect of dry socket. This pain can be severe enough to interfere with normal activities. In rare cases, a dry socket can become infected. Your dentist will prescribe medicines called antibiotics to destroy the infection.
How to treat dry socket pain?
Dry socket treatment usually involves the following steps: Flush out the socket: Your dentist will start by flushing out the socket to get rid of food particles, dead tissue, or anything else that has made its way into the socket. This helps provide dry socket pain relief and allows the tissue to heal better.
What is dry socket?
Dry socket, or alveolar osteitis, occurs when the blood clot present at the site of a tooth extraction dissolves or becomes dislodged. This blood clot is usually responsible for protecting the nerves and bone tissue present at the extraction site during the entire healing process.
Why does it take longer for a dry socket tooth to heal?
It will also take longer for the dry socket tooth to heal if you don't get it treated .
How do you know if you have a dry socket?
Some other dry socket symptoms include: Bad breath. An unpleasant taste in the mouth. Pain in the ears, eyes, jaw or neck. A headache. If you are experiencing any of these signs of dry socket, especially if you can see that there is no blood clot, you should contact your dentist for advice.
What does it feel like to have a dry socket after tooth removal?
However, a common dry socket symptom is a persistent throbbing or stabbing pain that begins or worsens a few days following tooth removal. The pain normally radiates to surrounding areas of the face. Drinking cold beverages, eating, or merely breathing may cause extreme pain and discomfort in the mouth.
What to do if your mouth is dry after a dry socket?
The dentist may apply a medicated dressing during dry socket treatment. Your dentist can take several steps to help your mouth properly heal following the surgery in order to prevent dry socket. This usually includes using certain medications such as: Antibacterial gels or mouthwashes both before and after surgery.
What happens if you have a dry socket?
The most common complication of dry socket is delayed healing. Infections may also occur; however, these might not be strictly associated with alveolar osteitis. If you develop any sign of infection, contact the dentist immediately. The most common symptoms include:
What is dry socket?
Dry socket, also termed fibrinolytic osteitis or alveolar osteitis, is a complication of tooth exodontia. A dry socket lesion is a post-extraction socket that exhibits exposed bone that is not covered by a blood clot or healing epithelium and exists inside or around the perimeter of the socket or alveolus for days after the extraction procedure. This article describes dry socket lesions; reviews the basic clinical techniques of treating different manifestations of dry socket lesions; and shows how microscope level loupe magnification of 6× to 8× or greater, combined with co-axial illumination or a dental operating microscope, facilitate more precise treatment of dry socket lesions. The author examines the scientific validity of the proposed causes of dry socket lesions (such as bacteria, inflammation, fibrinolysis, or traumatic extractions) and the scientific validity of different terminologies used to describe dry socket lesions. This article also presents an alternative model of what causes dry socket lesions, based on evidence from dental literature. Although the clinical techniques for treating dry socket lesions seem empirically correct, more evidence is required to determine the causes of dry socket lesions.
What is a dry socket lesion?
A dry socket lesion where the socket perimeter is fully covered with healing epithelium, but a septum of exposed bone is visible inside the socket. The occlusal aspect of the septum bone is inferior to the projected plane of the occlusal aspect of the socket when the socket fully heals.
How long does it take for a dry socket to appear?
In addition, the model can also demonstrate that there can be a 24- to 96-hour delay after an extraction before dry socket lesions appear2,5; that traumatic extractions, where heavy luxation or forceps forces are required to extract teeth particles, increase the incidence of dry socket lesions19; that plasmin-induced fibrinolysis activity seems higher in dry socket lesions compared to non-dry-socket post-extraction sockets2,6,9; and that bacteria do not seem to initiate dry socket lesions11,12,13. Such a model should explain whether or not inflammation causes dry socket lesions.
What causes dry sockets?
There is uncertainty in the dental literature about what causes dry socket lesions. Although some factors, such as smoking, oral contraceptive use, and presence of fibrinolytic activity in post-extraction sockets correlate with an increased incidence of dry socket, a definitive mechanism for explaining dry socket pathogenesis remains elusive1,2.
How does the necrotic bone in a socket heal?
Instead, clinical observation seems to show that the socket heals by a mechanism where vital epithelium, initially present at the outer perimeter of the socket, grows gradually from the outer perimeter of the socket inferiorly into the socket down to the apex of the socket. As the vital epithelium gradually covers the surface area of the socket intaglio surface, the epithelium brings blood vessels, immune system cells, and their complements in direct contact with the necrotic bone cells of the socket to begin resorbing the necrotic bone cells. This process of epithelium growth may take several days; during this time, the uncovered bone is painful to the touch and is vulnerable to painful contact with bacterial biofilm or food impaction.
What happens if you eat food in a dry socket?
Food particles that collect inside the socket may dislodge a blood clot. Bacterial biofilm and food particles inside a socket may also hinder the reformation of a dislodged blood clot by obstructing contact of a reforming blood clot with the exposed bone. Food particles and bacterial biofilm may hinder contact of the healing epithelium with the exposed bone, which may prolong the healing time of the dry socket lesion. Food particles that collect inside a dry socket can also ferment due to bacteria. This fermentation may result in the formation of toxins or antigens that may irritate the exposed bone, produce an unpleasant taste or halitosis, and cause pain throughout the jaw. However, evidence suggests that bacteria is not the main cause of dry socket lesions1,2.
What magnification is needed for a dry socket?
Microscope-level magnification of 6× to 8× or greater, combined with head-mounted or co-axial illumination, facilitates the observation of dry socket lesion anatomy such as exposed bone, either inside the socket or around the socket occlusal perimeter, areas of vital healing epithelium (which shows tensile strength when lightly probed), food particles or clumps of bacterial biofilm material within the socket, or inflamed gingival tissue, which may be sensitive to touch, but is not as sensitive as exposed bone.
How to treat dry sockets?
To care for the dry socket at home, your dentist may recommend that you rinse with salt water or a special mouthwash every day.
What does it mean when your tooth is dry socket?
You can endure it when you need to. But if the pain becomes intense and perhaps even worsen after a few days, it may be a symptom of a condition called dry socket, or alveolar osteitis. Only a very small percentage -- about 2% to 5% of people -- develop dry socket after a tooth extraction.
How long does it take for a clot to dissolve after tooth extraction?
Sometimes that clot can become dislodged or dissolve a couple of days after the extraction. That leaves the bone and nerve exposed to air, food, fluid, and anything else that enters the mouth. This can lead to infection and severe pain that can last for 5 or 6 days.
What can I take to help with pain?
You can take a nonsteroidal anti-inflammatory drug (NSAID), such as aspirin or ibuprofen, to ease the discomfort. Sometimes these over-the-counter medications aren't enough to relieve the pain. When that's the case, your doctor may prescribe a stronger drug or will anesthetize the area.
Can you drink after a tooth extraction?
After surgery, avoid drinking through a straw and spitting for the first few days. Also don't rinse your mouth more than your dentist recommends. If you do rinse, do so gently. Be sure to visit your dentist for all scheduled follow-up visits.
Can you smoke after a dry socket?
Because smoking is a big risk factor for dry socket, avoid cigarettes, cigars, and any other tobacco products for a day or so after your surgery. If you take birth control pills, ask your dentist about performing the extraction on a day when you are getting the lowest dose of estrogen.
Can you get dry socket after teeth are pulled?
have a history of dry socket after having teeth pulled. Rinsing and spitting a lot or drinking through a straw after having a tooth extracted also can raise your risk of getting dry socket.
How to help dry socket pain?
Test each and see what works best for you. Always use warm instead of hot, and place it against the cheek where you’re feeling pain.
How to flush out dry sockets?
The Mayo Clinic recommends dissolving ½ teaspoon of salt into 8 ounces of warm water. Swish this around in your mouth for a minute, or use it to flush out the dry socket with a syringe your surgeon gives you. Do this at least three times per day or after meals.
How to get rid of a swollen ear?
To use this remedy, immerse a tea bag in a cup of boiling water for five minutes. Remove it and squeeze the excess water out after it’s cooled.
What causes a dry socket?
The exact causes of dry socket still need more research. The most common causes are: 1 bacterial infection 2 difficult or complicated extractions, such as an impacted wisdom tooth 3 trauma at the surgical site
How do you know if you have a dry socket?
Symptoms of dry socket include: severe pain, which may radiate from the socket to your ear, eye, temple, or neck. seeing an empty socket. visible bone in the socket. bad breath or an unpleasant taste in your mouth.
What is the best medicine for swelling?
Over-the-counter NSAIDs. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can be effective at reducing both pain and swelling. They won’t be much help at treating or preventing an infection, but they can relieve pain until you can get to your doctor.
Can a dentist prescribe dry socket?
There are different treatments available for dry socket that your dentist or oral surgeon can prescribe to you. When you have to wait to get into see them, however, these home treatments can help alleviate symptoms.
What happens if you have a dry socket?
A dry socket can leave the nerves and bones in your gums exposed, so it’s important to seek dental care. If left untreated, this can lead to infection and other complications. Read on to learn how to recognize dry socket, how to help prevent this from occurring, and when you should call your dentist or oral surgeon for help.
How to tell if tooth extraction is dry socket?
If you’re able to look into your open mouth in a mirror and see bone where your tooth used to be, you’re probably experiencing dry socket. Another tell-tale sign of dry socket is an unexplained throbbing pain in your jaw. This pain may spread from the extraction site up to your ear, eye, temple, or neck.
What to do if you have pain after a tooth extraction?
If you experience extreme pain after having your tooth removed, it’s important to contact your dentist or surgeon right away. Your dentist will want to see you to look at the empty socket and to discuss next steps. In some cases, your dentist may suggest X-rays to rule out other conditions.
Why do teeth get dry sockets?
When a tooth is removed from the bone and gums, a blood clot is supposed to form to protect the hole in your gums as it heals. If the blood clot doesn’t form properly or becomes dislodged from your gums, it can create a dry socket. A dry socket can leave the nerves and bones in your gums exposed, so it’s important to seek dental care.
What to do after removing a dressing?
After removing your dressing, you’ll need to clean the socket again. Your dentist will likely recommend a salt water or prescription rinse.
Why do dentists clean sockets?
If you have a dry socket, your dentist will clean the socket to make sure it’s free of food and other particles. This may alleviate any pain and can help prevent infection from forming.
How long does it take for pain to go away after a syringe?
If you’re still dealing with pain or swelling after about five days , you should see your dentist.
What to do for dry socket after surgery?
These steps may include recommending one or more of these medications, which may help prevent dry socket: Antibacterial mouthwashes or gels immediately before and after surgery. Oral antibiotics, particularly if you have a compromised immune system. Antiseptic solutions applied to the wound.
How do you know if you have a dry socket?
Signs and symptoms of dry socket may include: Severe pain within a few days after a tooth extraction. Partial or total loss of the blood clot at the tooth extraction site, which you may notice as an empty-looking (dry) socket. Visible bone in the socket.
What does it mean when you have a dry socket after a tooth extraction?
Partial or total loss of the blood clot at the tooth extraction site, which you may notice as an empty-looking (dry) socket. Pain that radiates from the socket to your ear, eye, temple or neck on the same side of your face as the extraction.
What is the purpose of a blood clot in a tooth extraction?
This blood clot serves as a protective layer over the underlying bone and nerve endings in the empty tooth socket. The clot also provides the foundation for the growth of new bone and for the development of soft tissue over the clot. Exposure of the underlying bone ...
What to do if you have pain after a tooth extraction?
If you develop new or worsening pain in the days after your tooth extraction, contact your dentist or oral surgeon immediately.
How long does it take for a tooth to dry out after extraction?
If you develop dry socket, the pain usually begins one to three days after your tooth is removed. Dry socket is the most common complication following tooth extractions, such as the removal of third molars (wisdom teeth). Over-the-counter medications alone won't be enough to treat dry socket pain.
How to get rid of a blood clot in your socket?
Drink lots of water after the surgery. Avoid alcoholic, caffeinated, carbonated or hot beverages for as long as your dentist or oral surgeon recommends. Don't drink with a straw for at least a week because the sucking action may dislodge the blood clot in the socket.
What is the best treatment for dry socket?
Turmeric. People can use turmeric to help treat dry socket. The curcumin in turmeric has strong anti-inflammatory properties that may reduce pain and aid wound healing. , a dressing of turmeric and mustard oil reduced pain, discomfort, and inflammation in people with dry socket.
What to do if you have a dry socket?
The dentist may also recommend that people use either a rinse, saline solution, or saltwater mix daily as the dry socket heals.
What to do after a tooth extraction?
A dentist will usually advise people to rinse their mouth with a saline solution, or salt water, following a tooth extraction, as this helps the healing process. It is very important to rinse gently as blood clots can easily become dislodged.
What happens if a tooth is dry socketed?
Here’s our process. Dry socket happens when a blood clot either does not form properly or falls out after a tooth extraction. The lack of a protective blood clot exposes both the nerves and bone. Dry socket can be very painful, but it usually heals quickly with treatment. Symptoms of dry socket include:
How long does it take for a tooth to dry out after extraction?
People may experience dry socket up to a few days after a tooth extraction. It is best to see a dentist for dry socket, but some home remedies can help ease the pain while a person waits for treatment.
How to diagnose dry socket?
A dentist can diagnose dry socket by carrying out a visual examination. They may also use an X-ray to check that another condition, such as an infection of the bone, is not causing the symptoms.
How to get rid of a swollen socket?
Rinsing the mouth with warm salt water can help reduce bacteria and swelling. It can also flush out any food particles from the socket. Keeping this area clean can reduce pain and lower the risk of infection.
How to treat a dry socket?
Drink plenty of clear liquids to remain hydrated and to prevent nausea that may be associated with some pain medications. Rinse your mouth gently with warm salt water several times a day. Brush your teeth gently around the dry socket area.
What to do if you have a socket that hurts?
Flushing out the socket. Flushing out the socket can remove any food particles or other debris that may contribute to pain or possible infection. Medicated dressings. Your dentist or oral surgeon may pack the socket with medicated gel or paste and medicated dressings. These can provide relatively fast pain relief.
How to get rid of a swollen socket?
Typically you'll receive instructions and a plastic syringe with a curved tip to squirt water, salt water or a prescription rinse into the socket. You'll likely need to continue the rinse until the socket no longer collects any debris. Once treatment is started, you may soon begin to feel some pain relief.
What to do if you have pain after a tooth extraction?
Make an appointment with your dentist or oral surgeon as soon as possible if you develop new or worsening pain after a tooth extraction.
Can a tooth extraction cause dry socket?
Severe pain following a tooth extraction is often enough for your dentist or oral surgeon to suspect dry socket. He or she will also ask about any other symptoms and examine your mouth to see if you have a blood clot in your tooth socket and whether you have exposed bone.