- Macrolides (e.g., azithromycin): Children and adults
- Fluoroquinolones: Adults
- Tetracyclines (e.g., doxycycline): Older children and adults
What group of antibiotics would Mycoplasma be resistant to?
- Macrolides (e.g., azithromycin): Children and adults
- Fluoroquinolones: Adults
- Tetracyclines (e.g., doxycycline): Older children and adults
What is the strongest antibiotic for pneumonia?
What is the strongest antibiotic for pneumonia? Levofloxacin is rapidly becoming a popular choice in pneumonia; this agent is a fluoroquinolone used to treat CAP caused by S aureus, S pneumoniae (including penicillin-resistant strains), H influenzae, H parainfluenzae, Klebsiella pneumoniae, M catarrhalis, C pneumoniae, Legionella pneumophila, or M pneumoniae.
Does amoxcillin treat mycoplasma pneumonia?
Not really: The organism mycoplasma is not sensitive to amoxicillin.These organisms are resistant to the effects of penicillins and other beta-lactam antibiotics,... Read More Depends: It depends on the cause of the pneumonia. A penicillin sensitive strain of s. Pneumoniae could be effectively treated with amoxicillin. You list "atyp... Read More
Will Cipro treat mycoplasma?
The fluoroquinolone antibiotic Ciprofloxacin, has been used to eliminate mycoplasma from 26 naturally infected cell lines with no evidence of remergence of infection and with no treatment failures. Download to read the full article text References 1. Aula P and Nichols WW (1967) The cytogenetic effects of mycoplasma in human leucocyte cultures.
Which of the following antibiotics is found to be most effective against Mycoplasma?
Tetracyclines, fluoroquinolones, and macrolides are the most effective anti-mycoplasma agents. They are widely used to suppress mycoplasma infection and contamination of cell cultures.
Does azithromycin treat Mycoplasma pneumoniae?
Compared with erythromycin, azithromycin is more effective in the treatment of mycoplasma pneumonia in children. Azithromycin can further shorten the improvement time of clinical symptoms and signs and has few adverse reactions and high safety. It is worth clinical application.
Can ciprofloxacin treat Mycoplasma pneumoniae?
Ciprofloxacin is generally considered as an effective treatment against Mycoplasma pneumoniae based on in-vitro susceptibility to ciprofloxacin. Till date there has been only one case report of its effective use (Masayoshi et al. Antibiotics and Chemotherapy.
Does amoxicillin treat Mycoplasma?
Neither amoxicillin nor amoxicillin clavulanate cover the atypical organisms, Mycoplasma pneumoniae, Chlamydia pneumoniae or Legionella sp.
What is the first line antibiotic for treating Mycoplasma pneumoniae?
Macrolides and related antibiotics are the first-line treatment of M. pneumoniae respiratory tract infections mainly because of their low MIC against the bacteria, their low toxicity and the absence of contraindication in young children.
Does doxycycline treat Mycoplasma?
In this study, we report a 58.9% cure rate after a two-week course of doxycycline on macrolide resistant infections of M.
What is the strongest antibiotic for upper respiratory infection?
Amoxicillin is the preferred treatment in patients with acute bacterial rhinosinusitis. Short-course antibiotic therapy (median of five days' duration) is as effective as longer-course treatment (median of 10 days' duration) in patients with acute, uncomplicated bacterial rhinosinusitis.
What is the best antibiotic to treat pneumonia?
In otherwise uncomplicated pneumonia, azithromycin is the initial drug of choice, as it covers most of the potential etiologic agents, including Mycoplasma species.
Will doxycycline treat pneumonia?
Types of Antibiotics for Pneumonia Healthy adults under 65 years with pneumonia are typically treated with a combination of amoxicillin plus a macrolide like Zithromax (azithromycin) or sometimes a tetracycline like Vibramycin (doxycycline).
What antibiotics treat Mgen?
Mycoplasma genitalium treatment The mainstay of treatment used to be a single dose of an antibiotic, azithromycin. However, longer courses of treatment are needed. Newer medicines like pristinamycin, solithromycin, and sitafloxacin are being tried.
How long does it take for doxycycline to work for Mycoplasma?
Initial empiric therapy for PID, which includes doxycycline 100 mg orally 2 times/day for 14 days, should be provided at the time of presentation for care. If M. genitalium is detected, a regimen of moxifloxacin 400 mg orally once daily for 14 days has been effective in eradicating the organism.
Can Mycoplasma pneumonia go away on its own?
Mycoplasma pnuemoniae infections are generally mild, but some people may need care in a hospital. Most people will recover from an infection caused by Mycoplasma pneumoniae without antibiotics.
What to do if you have pneumonia?
However, if someone develops pneumonia (lung infection) caused by M. pneumoniae, doctors usually prescribe antibiotics. There are several types of antibiotics available to treat pneumonia caused by M. pneumoniae.
What is it called when there are too few red blood cells?
Hemolytic anemia (too few red blood cells, which means fewer cells to deliver oxygen in the body)
Can antibiotics help with pneumonia?
There are several types of antibiotics available to treat pneumonia caused by M. pneumoniae. Antibiotics can help patients recover from the infection faster if started early on. Some M. pneumoniae are resistant to some antibiotics used for treatment.
Can you recover from mycoplasma pneumoniae?
Mycoplasma pnuemoniae infections are generally mild, but some people may need care in a hospital. Most people will recover from an infection caused by Mycoplasma pneumoniae without antibiotics.
Can pneumoniae cause a severe infection?
While M. pneumoniae usually cause mild infections, severe complications can occur that require care in a hospital. M. pneumoniae infections can cause or worsen the following complications:
What antibiotics are used for mycoplasmal pneumonia?
In the treatment of mycoplasmal pneumonia, antimicrobials against M pneumoniae are bacteriostatic, not bactericidal. Tetracycline and erythromycin compounds are very effective. The second-generation tetracyclines (doxycycline) and macrolides are the drugs of choice. [ 52] Macrolide resistance has been reported in several areas of the world, but most experts agree that macrolides are the antibiotics of choice for treating M pneumoniae infections in adults and children. [ 53, 54, 55, 56, 57] If a patient does not respond appropriately to a macrolide, a fluoroquinolone should be added to the treatment regimen. [ 53, 54] Penicillins and cephalosporins are ineffective, because the organism lacks a cell wall.
How much resistance does macrolide have?
Macrolide resistance has been increasing throughout the world, with 0-15% resistance in Europe and the United States, 30% in Israel, and 90-100% in Asia, [ 58] but macrolides remain the mainstay of treatment. If symptoms do not resolve, consider prescribing tetracyclines (doxycycline and minocycline) or fluoroquinolones (levofloxacin). [ 59] .
What is the best antibiotic for M pneumonia?
View full drug information. Azithromycin is a macrolide antibiotic that is very effective against M pneumoniae and may be the most common agent used to treat M pneumoniae given its ease of administration. Clarithromycin (Biaxin, Biaxin XL) View full drug information.
What is doxycycline used for?
Doxycycline is a tetracycline antibiotic that is used to treat susceptible bacterial infections of both gram-positive and gram-negative organisms, as well as infections caused by Mycoplasma, Chlamydophilia, and Rickettsia organisms.
What is an empiric antibiotic?
Empiric antimicrobial therapy must be comprehensive and should cover all likely pathogens in the context of the clinical setting. Erythromycin (E.E.S., Erythrocin, Ery-Tab) View full drug information. Erythromycin is a macrolide antibiotic that is used in the treatment of staphylococcal and streptococcal infections.
Which antibiotic inhibits bacterial protein synthesis?
Doxycycline inhibits bacterial protein synthesis by binding with the 30S subunit and possibly the 50S ribosomal subunit of susceptible bacteria. Levofloxacin (Levaquin) View full drug information. Levofloxacin is a fluoroquinolone antibiotic that can be used to treat Mycoplasma infections.
How does moxifloxacin work?
It works by inhibiting the A subunits of DNA gyrase, resulting in inhibition of bacterial DNA replication and transcription. Moxifloxacin is a fluoroquinolone antibiotic that inhibits the A subunits of DNA gyrase, resulting in inhibition of bacterial DNA replication and tran scription. McCormack WM.
Why is mycoplasma difficult to eradicate?
Mycoplasmas may be difficult to eradicate from human or animal hosts or from cell cultures by antibiotic treatment because of resistance to the antibiotic, or because it lacks cidal activity, or because there is invasion of eukaryotic cells by some mycoplasmas.
How do mycoplasmas develop resistance to antibiotics?
In addition, some may develop resistance, either by gene mutation or by acquisition of a resistance gene, to antibiotics to which they are usually sensitive. Resistance of mycoplasmas to tetracyclines is common and due to acquisition of the tetM gene.
What is the smallest free living microorganism?
Mycoplasmas are the smallest free-living microorganisms, being about 300 nm in diameter. They are bounded by a triple-layered membrane and, unlike conventional bacteria, do not have a rigid cell wall. Hence, they are not susceptible to penicillins and other antibiotics that act on this structure.
Is mycoplasma genitalium resistant to penicillin?
Apart from the penicillins, mycoplasmas are innately resistant to some other antibiotics, for example the rifampicins.
Is eradication of mycoplasma difficult?
Eradication may be particularly difficult in immunosuppressed or immunodeficient individuals, particularly those who are hypogammaglobulinaemic. The regimes that are most likely to be effective in the treatment of respiratory or genitourinary mycoplasmal infections are presented.
Do macrolides kill genital infections?
They are, however, susceptible to a variety of other broad-spectrum antibiotics, most of which only inhibit their multiplication and do not kill them. The tetracyclines have always been in the forefront of antibiotic usage, particularly for genital tract infections, but macrolides are also widely used for respiratory tract infections.
Can antibiotics treat pneumonia?
In contrast, antibiotic treatment of severe cases of M. pneumoniae pneumonia is complicated. The clinical benefit of tetracyclines and fluoroquinolones has been shown in terms of shortening duration of symptoms and rapid defervescence in some reports.
Is mycoplasma pneumoniae a community acquired disease?
Abstract. Mycoplasma pneumoniae is an important cause of community-acquired pneumonia in children and young adolescents. Macrolides are recommended as the first-line therapy however, macrolide resistance rates in M. pneumoniae among children have been increasing substantially.
Is antibiotic resistance based on in vitro activity?
Expert commentary: Antibiotic choice should be based on in vitro activity, clinical efficacy and in consideration of potential adverse events. Macrolide resistance did not contribute to the clinical severity of M. pneumoniae pneumonia, but resistance may be an aggravating factor. Antibiotics may not be required for treatment in mild cases due ...
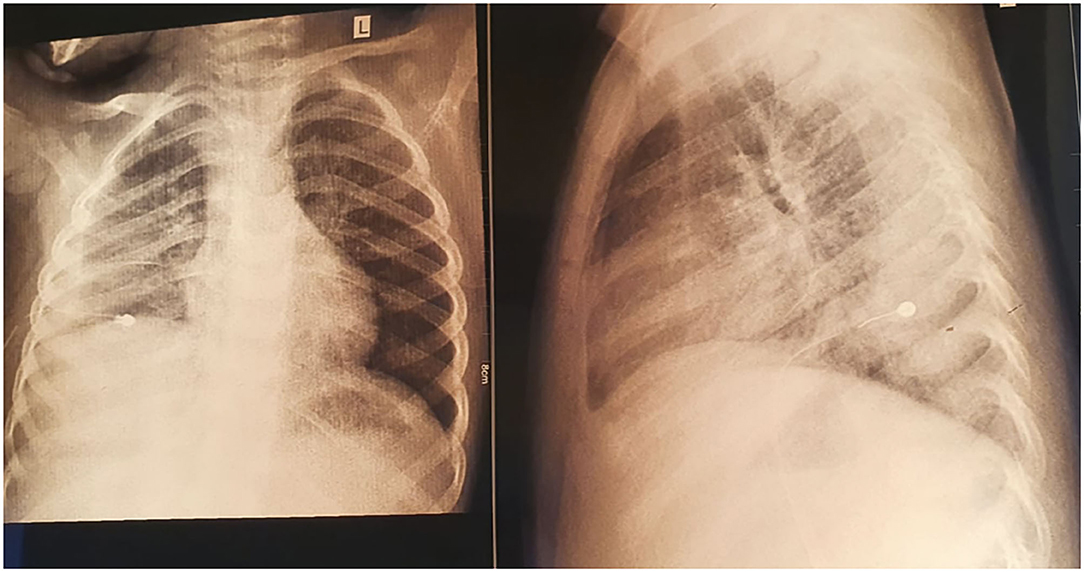
When to use alternative antibiotics after macrolide?
Alternative antibiotics may be considered when patients remain febrile or when chest x-rays show deterioration at least 48-72 hours after macrolide treatment.
What is the cause of LRTI in children?
Read the full abstract... Background: Mycoplasma pneumoniae ( M. pneumoniae) is widely recognised as an important cause of community-acquired lower respiratory tract infection (LRTI) in children. Pulmonary manifestations are typically tracheobronchitis or pneumonia but M. pneumoniae is also implicated in wheezing episodes in both asthmatic ...
What is M. pneumoniae?
Background. M. pneumoniae is a bacterial infection, often responsible for lower respiratory tract infections (LRTIs) in children. The infection can present in a number of different ways and the most common respiratory manifestations are acute bronchitis, pneumonia or wheezing.
Is there evidence that antibiotics are effective in children with LRTI?
Hence, currently, there is insufficient evidence to show conclusively that antibiotics are effective in children with LRTI caused by M. pneumoniae.
Can pneumoniae be self limiting?
The illness is generally self limiting, with symptoms that can last several weeks but may (occasionally) also cause severe pneumonia. Antibiotics are often given to children with M. pneumoniae LRTI. Search date. We searched for trials published and pending as at July 2014. Study characteristics.
Can antibiotics treat respiratory infections?
Antibiotics to treat respiratory infections caused by the bacteria Mycoplasma pneumoniae in children. This review sought to answer the question of whether antibiotics are effective in the treatment of LRTIs caused by the bacteria Mycoplasma pneumoniae ( M. pneumoniae) in children.