
Explore
Mar 18, 2021 · Treatment during a diagnostic procedure. During an upper GI endoscopy, a lower GI endoscopy, a colonoscopy, a flexible sigmoidoscopy, or a laparotomy, a doctor can stop the bleeding in your GI tract. He or she can stop the bleeding by inserting tools through an endoscope, colonoscope, or sigmoidoscope to. inject medicines into the bleeding site. treat the bleeding …
Which drugs are indicated for upper GI bleeding?
May 10, 2021 · Doctors can stop or control upper GI bleeding with medications or use heat or surgery to seal wounds. Treating the underlying condition can then prevent further bleeding.
How do medications treat upper GI bleeding?
Medications for prophylaxis may protect patients from upper GI bleeding. Pharmacologic treatment Aims of antisecretory therapy: Increasing intragastric pH < 6. Treatment of peptic ulcer disease. Control of symptoms. Proton pump inhibitors Omeprazole (Prilosec; AstraZeneca LP, Wilmington, DE) Open in a separate window
What could cause upper GI bleed?
Jul 21, 2021 · The use of antacids has been shown to alter the natural history of patients with acute upper GI bleeding. Patients with significant bleeding should be treated with an 80-mg bolus of PPI followed by a continuous infusion. The typical duration is 72 hours for patients with high-risk lesions visualized on EGD.
What are the symptoms of upper GI?
Apr 28, 2021 · bleeding from the anus. red blood in stool. A serious, significant bleed, especially in the upper GI tract, may cause other symptoms, such as: …
Is upper GI bleeding treatable?
Can you recover from GI bleed?
How do they fix a GI bleed?
- inject medicines into the bleeding site.
- treat the bleeding site and surrounding tissue with a heat probe, an electric current, or a laser.
- close affected blood vessels with a band or clip.
How long does it take to recover from a GI bleed?
What happens if a GI bleed goes untreated?
What is the most common cause of upper GI bleeding?
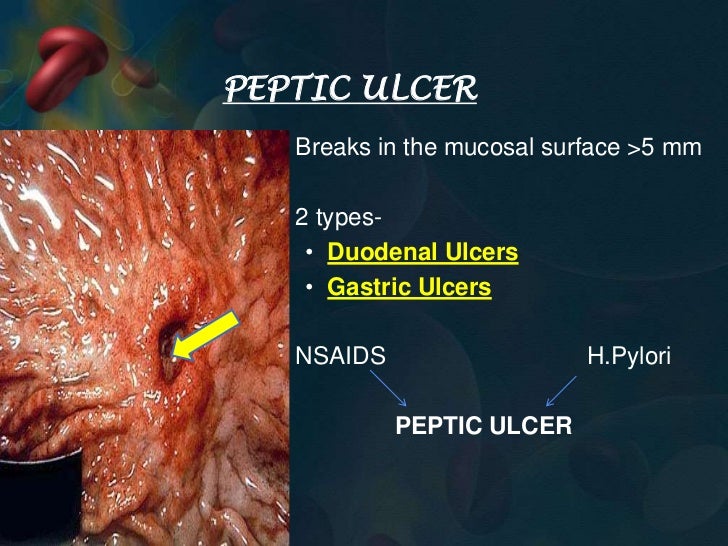
Bleeding peptic ulcers account for the majority of patients presenting with acute upper gastrointestinal (GI) bleeding (UGIB). As previously mentioned, peptic ulcer disease is strongly associated with H pylori infection.Sep 1, 2021
What can cause an upper GI bleed?
- Angiodysplasia. Angiodysplasia is when you have abnormal or enlarged blood vessels in your GI tract. ...
- Benign tumors and cancer. ...
- Colitis. ...
- Colon polyps. ...
- Diverticular disease. ...
- Esophageal varices. ...
- Esophagitis. ...
- Gastritis.
Can a CT scan detect GI bleeding?
What to do if you have a GI bleed?
When you have an upper GI bleed, the first step in treatment is to stabilize your vital signs. This is because, in cases of severe bleeding, you are at risk of potentially going into shock from significant blood loss.
What causes GI bleeding?
The most common cause of upper GI bleeding is peptic ulcers (ulcers in the stomach). These account for 60% of upper GI bleeds. They are more prevalent in individuals who have active H. Pylori infection in their stomachs, so offering antibiotic treatment for this bacteria may be part of the advised treatment plan.
Does aspirin cause GI bleeding?
Therefore, if you are taking one regularly, consider stopping it and/or replacing it with a different medication. Aspirin, which interrupts platelet aggregation and hence worsens any existing bleeds. Talk to your doctor about temporarily stopping this medication until your GI bleed is resolved.
What does it mean when you vomit blood?
Vomiting blood, which may resemble coffee grounds. Black stools with a foul odor. Fresh blood passing through the anus, usually found with stool (this is more likely to indicate lower GI bleeding, but may still be present with upper GI bleeding) Feeling faint and lightheaded, weak.
What to do if you lose blood?
In cases of severe blood loss, the key will be to replace the lost blood and stabilize you medically before moving onto specific diagnosis and treatment options. If you are only losing minimal blood, however, your doctor can proceed straight to diagnosis and treatment.
What does a blood test show?
The blood test will check your hemoglobin levels, which is the molecule in your blood that is responsible for carrying oxygen. Low hemoglobin is diagnostic of "anemia," and the severity of the anemia correlates to the degree of blood lost from the GI bleed.
What is IV fluid?
IV fluids are given in cases of less severe blood loss. They boost your blood volume (the amount of fluid traveling in your circulatory system), but do not directly increase the hemoglobin (or functional oxygen-carrying capacity) of your blood.
Treatment during a diagnostic procedure
During an upper GI endoscopy, a lower GI endoscopy, a colonoscopy, a flexible sigmoidoscopy, or a laparotomy, a doctor can stop the bleeding in your GI tract. He or she can stop the bleeding by inserting tools through an endoscope, colonoscope, or sigmoidoscope to
Medicines
When infections or ulcers cause bleeding in your GI tract, health care professionals prescribe medicines to treat the problem.
Surgery
When a person has severe acute bleeding or bleeding that does not stop, a surgeon may need to perform a laparoscopy or a laparotomy to stop the bleeding.
What is upper GI bleed?
What is an upper GI bleed? Upper GI bleeds occur when part of the upper digestive tract becomes injured or inflamed. A GI bleed is a symptom of another disorder rather than a health condition in itself. Doctors divide GI bleeds into upper and lower bleeds depending on the source of the blood.
Is GI bleeding a medical emergency?
Sudden and severe GI bleeding is a medical emergency, but slower, chronic bleeding can also become serious over time. Anyone who suspects that they have a GI bleed should see a doctor right away.
Where does GI bleeding occur?
Upper gastrointestinal (GI) bleeding refers to bleeding that occurs anywhere in the esophagus, the stomach, or the upper part of the small intestine. It is a symptom of an underlying disorder, and it can be serious.
Can GI bleeding cause anemia?
Chronic GI bleeding is slower bleeding that can last a long time or may come and go. However, it can still lead to significant health complications, such as anemia.
What to do if a doctor suspects bleeding?
If a doctor suspects that bleeding is responsible for a person’s symptoms, they will take a medical history and perform a physical exam. They may then ask questions about the person’s symptoms, as well as their bowel movements and the color of their stool.
How to tell if you have a GI bleed?
The symptoms of a GI bleed can include: black, tarry stool. vom it that is bright red or resembles coffee grounds. stomach cramps. unusually pale skin. feeling faint, dizzy, or tired.
What are the symptoms of a GI bleed?
Acute GI bleeds can also lead to shock, which is a medical emergency. The symptoms include: a rapid pulse. a drop in blood pressure. little to no urination.
Can GI bleeding be treated?
GI bleeding can be due to a number of causes, and treatment will depend on what the bleeding results from. In some cases, doctors may recommend ongoing management of the condition to relieve symptoms. A person needs to contact a doctor if they experience any symptoms of GI bleeding.
What is GI bleeding?
FG Trade/Getty Images. GI bleeding is a type of bleeding that occurs anywhere in the digestive system. It may be due to an injury, infection, or inflammation. The bleeding may appear suddenly and produce a lot of blood, or a person may notice gradual or periodic bleeding. Sudden, heavy bleeding is more immediately dangerous.
Where does GI bleeding occur?
Gastrointestinal (GI) bleeding is bleeding in the digestive tract, anywhere from the throat to the rectum. A person can experience a small loss of blood, such as when a hemorrhoid bleeds, or a hemorrhage, which causes a substantial blood loss. In this article, we discuss GI bleeding, its symptoms, severity, potential causes, risk factors, ...
Is GI bleeding life threatening?
Some types of GI bleeding are life threatening and require prompt treatment. Typically, upper GI bleeds are more dangerous. Trusted Source. than those occurring in the lower part of the digestive tract. Sudden bleeding may produce symptoms of shock, such as blood pressure changes or a rapid pulse.
Can a tumor cause bleeding?
Growths in the digestive tract, including both benign and cancerous tumors, may cause bleeding. Some people also notice other symptoms, such as difficulty swallowing, but not all growths cause symptoms. A person may require surgery to remove the growth.
What are the risk factors for GI bleeding?
Anyone can have a GI bleed, especially if they experience other digestive issues, such as colitis or peptic ulcers. Risk factors for GI bleeding include: using anticoagulants, which are a group of drugs that can thin the blood and may therefore increase bleeding.
What does it mean when you have blood on your toilet paper?
blood on toilet paper or baby wipes after wiping. bleeding from the anus. red blood in stool. A serious, significant bleed, especially in the upper GI tract, may cause other symptoms, such as: little or no urine to pass. a drop in blood pressure . confusion. intense nausea. loss of consciousness.
What are the causes of peptic ulcer bleeding?
H. pylori infection and NSAIDs are the major causes of peptic ulcer bleeding in the United States; therefore, preventive strategies should focus on these etiologies. Smoking and alcohol use impair ulcer healing, and patients should be counseled about smoking cessation and moderation of alcohol use. A systematic review of 41 randomized controlled trials of patients taking NSAIDs found that double-dose H 2 receptor antagonists (relative risk [RR] = 0.44) and PPIs (RR = 0.40) significantly reduced the risk of peptic ulcer bleeding. 27 In patients with a history of peptic ulcer bleeding, aspirin, clopidogrel, and NSAIDs should be avoided if possible. In patients taking aspirin who develop peptic ulcer bleeding, aspirin therapy with PPI therapy should be restarted as soon as the risk of cardiovascular complication is thought to outweigh the risk of rebleeding. 1 A Cochrane review of seven studies of 578 patients with peptic ulcer bleeding concluded that eradication of H. pylori infection reduced the long-term rate of rebleeding (2.9 percent) compared with patients in the noneradication group (20 percent; number needed to treat = 7). 28 In patients with peptic ulcer bleeding associated with H. pylori infection, eradication is essential and should be confirmed by urea breath test, stool antigen test, or biopsy urease test. 1 A repeat upper endoscopy in eight to 12 weeks is recommended for patients with peptic ulcer bleeding secondary to gastric ulcers to assess for healing and to exclude malignancy, and for patients with severe esophagitis to exclude Barrett esophagus.
How many patients have rebleeding?
Despite successful endoscopic therapy, rebleeding can occur in 10 to 20 percent of patients; a second attempt at endoscopic therapy is recommended in these patients. Arteriography with embolization or surgery may be needed if there is persistent and severe bleeding.
Is a duodenal ulcer more common than a gastric ulcer?
In the United States, duodenal ulcers are more common than gastric ulcers. 6 Patients with gastric ulcers (55.1 percent) are hospitalized more often than patients with duodenal ulcers (38.5 percent), but the mortality rate of patients with duodenal ulcers (3.7 percent) is higher than that of patients with gastric ulcers (2.1 percent). 6 Duodenal ulcers are more likely to erode into large vessels, causing more severe bleeding. In a meta-analysis of 16 studies involving 1,633 participants taking NSAIDs, H. pylori infection (odds ratio [OR] = 1.7) and NSAID use (OR = 4.8) increased the risk of upper gastrointestinal bleeding, with this risk increasing further when both factors are present (OR = 6.1). 7 H. pylori adheres to the gastric epithelium and renders the underlying mucosa more vulnerable to damage by producing enzymes and toxins, 8 affecting gastrin levels and acid output. The risk of upper gastrointestinal bleeding varies based on the type of NSAID used ( Table 2). 9
