Is supersensitivity psychosis a cause of relapse in psychosis?
The first-line treatment for psychotic disorders remains antipsychotic drugs with receptor antagonist properties at D2-like dopamine receptors. However, long-term administration of antipsychotics can upregulate D2 receptors and produce receptor supersensitivity manifested by behavioral supersensitivity to dopamine stimulation in animals, and movement disorders and …
Does supersensitivity psychosis require compliance with antipsychotics?
Mar 21, 2022 · Background: An association between abnormal involuntary movements and psychotic relapse was previously reported in a group of patients compliant with antipsychotic medication (Fallon and Dursun 2011). This was interpreted as the presence of an antipsychotic medication-induced supersensitivity psychosis.
What is supersensitivity psychosis (SSP)?
The Particular Case of Clozapine] [The Concept of Supersensitivity Psychosis. The Particular Case of Clozapine] Abstract Neuroleptics are the main biological treatment for psychotic patients. The brutal withdrawal of a neuroleptic treatment may induce an important aggravation of the psychotic symptoms.
How common is supersensitivity to dopamine in schizophrenia?
Supersensitivity psychosis has emerged as a potential side effect of long-term neuroleptic therapy that may be similar to tardive dyskinesia. Schizophrenic patients …
How is tardive psychosis treated?
Treatment of tardive dyskinesia initially consists of discontinuing the neuroleptic drug as soon as involuntary facial, neck, trunk, or extremity movements are identified in people taking neuroleptic drugs if this is felt to be safe psychiatrically.
What is risperidone used for?
Risperidone is used to treat schizophrenia, bipolar disorder, or irritability associated with autistic disorder.
Which medication will be used to treat psychosis?
Antipsychotic medicines are usually recommended as the first treatment for psychosis. They work by blocking the effect of dopamine, a chemical that transmits messages in the brain.
What is supersensitivity rebound psychosis?
Abstract. Dopamine supersensitivity psychosis (DSP) is observed in patients with schizophrenia under antipsychotic treatment, and it is characterized by rebound psychosis, an uncontrollable psychotic episode following a stable state and tardive dyskinesia.
Can risperidone cause psychosis?
Conclusions: This observation of "on-off" risperidone treatment suggests that risperidone may have worsened both psychiatric and physical manifestations of the mitochondrial disorder in this adolescent.
Why is Risdone prescribed?
Risperidone is used to treat the symptoms of schizophrenia (a mental illness that causes disturbed or unusual thinking, loss of interest in life, and strong or inappropriate emotions) in adults and teenagers 13 years of age and older.
What is the main drug used to treat schizophrenia?
Haloperidol, fluphenazine, and chlorpromazine are known as conventional, or typical, antipsychotics and have been used to treat schizophrenia for years. However, they sometimes have movement-related side effects, such as tremors and dystonia, a condition that causes involuntary muscle contractions.
What is the best antipsychotic medicine?
With respect to the incidence of discontinuation, clozapine was the most effective antipsychotic drug, followed by aripiprazole. As with the survival analysis for time to discontinuation, clozapine and aripiprazole were the top ranked.Nov 19, 2020
How do antipsychotics treat schizophrenia?
Antipsychotics are usually recommended as the initial treatment for the symptoms of an acute schizophrenic episode. They work by blocking the effect of the chemical dopamine on the brain.
What is dopamine supersensitivity psychosis?
Dopamine supersensitivity psychosis is a hypothesis that attempts to explain the phenomenon in which psychosis (e.g. having hallucinations, which can mean hearing or seeing things that other people do not see or hear) occurs despite treatment with escalating doses of antipsychotics.
What is supersensitivity pharmacology?
Disuse supersensitivity, also pharmacological disuse supersensitivity or pharmacological denervation supersensitivity, is the increased sensitivity by a postsynaptic cell because of decreased input by incoming axons, e.g., due to the exposure to an antagonist drug.
Do antipsychotics upregulate dopamine receptors?
While antipsychotic medication may not elevate the density of dopamine D 2 receptors, it has been shown that they can increase the number of dopamine D 2 high receptors in animal studies.
What is the optimal D2 receptor occupancy?
Several studies have proposed an optimal dopamine D2 receptor occupancy by antipsychotics (OOc) to establish optimal pharmacological treatment of schizophrenia. However, there are limitations to the use of the OOc, especially in application to patients with treatment-resistant schizophrenia, including dopamine supersensitivity psychosis (DSP) or late-onset psychosis (LOP). It has been suggested that D2 receptor density is up-regulated by chronic treatment of antipsychotics in DSP, whereas it may be low in LOP owing to age-related reduction. In estimation of the proposed OOc, these alterations have not been taken into account, which may be one of the factors contributing to the limited application of this index. We here hypothesize that there is an optimal range in the number of D2 receptors available for dopamine binding to elicit adequate neurotransmission in the treatment of patients with schizophrenia. We then estimated the OOc under the assumption that the range is constant while D2 density is variable. The results showed that the OOc and plasma level of antipsychotics increase with an increase in the D2 density but decrease with a decrease in the D2 density. That is, if the range of OOc is 65% to 78% in a standard D2 density, it becomes 82% to 89% under 2-fold up-regulated density and 42% to 63% under a 40% reduced density. The results also indicated that the reduction of the plasma antipsychotic level is greater during a given time period in patients with higher D2 density, as they need a higher antipsychotic dose to achieve the raised OOc, which would account for the clinical features of DSP, for example, acute exacerbation after a discontinuation of antipsychotics. On the other hand, in patients with lower D2 density, only a lower antipsychotic dose will achieve the OOc, and a small increase in the dose will result in a greater increase in occupancy and induce extrapyramidal adverse effects more easily. Furthermore, the reduction of the plasma antipsychotic level during the time period is smaller, which prolongs extrapyramidal adverse effects after discontinuation of antipsychotics in LOP. We also attempted to develop a strategy for the prevention and treatment of patients with DSP or LOP by focusing on D2 density.
What is DSP in schizophrenia?
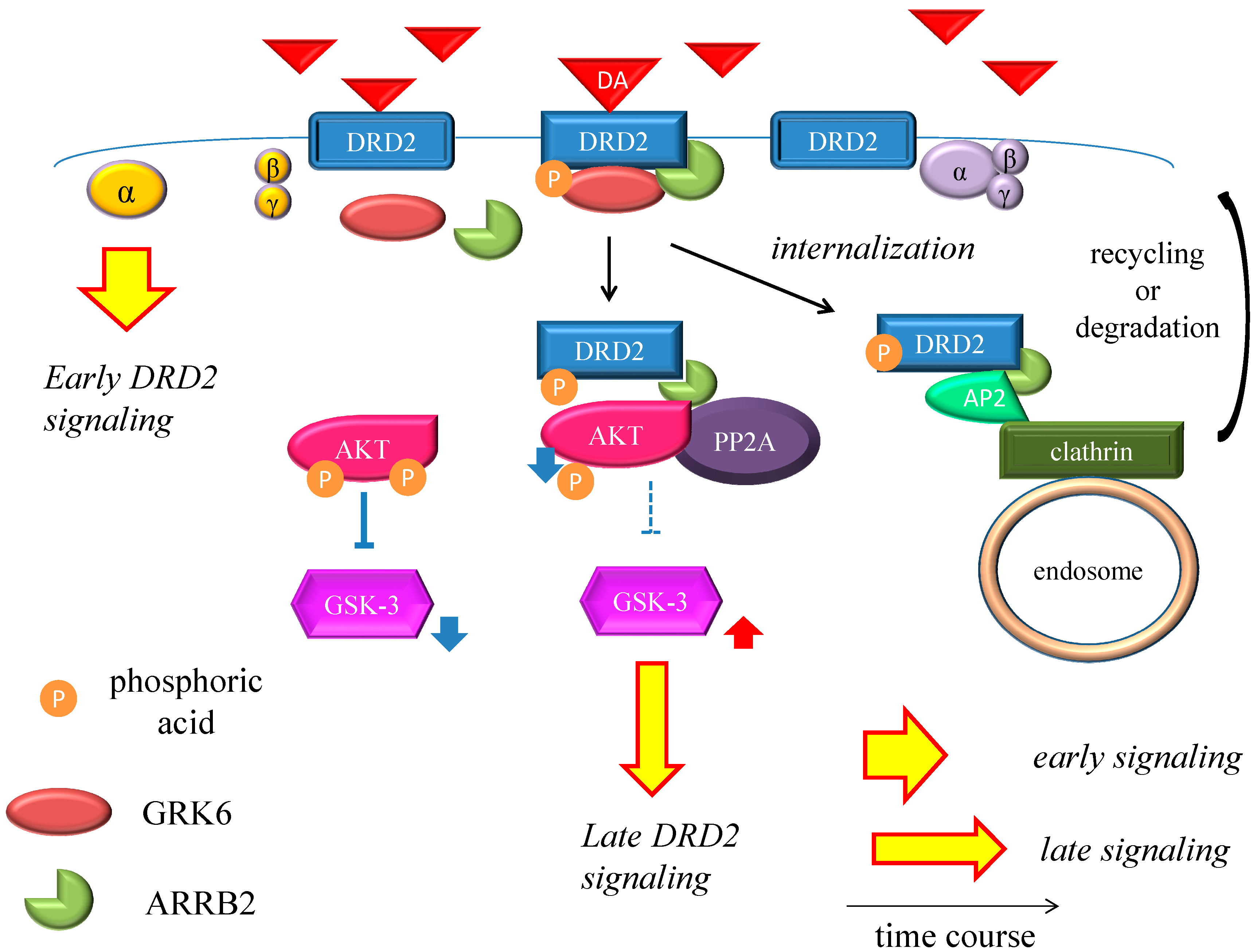
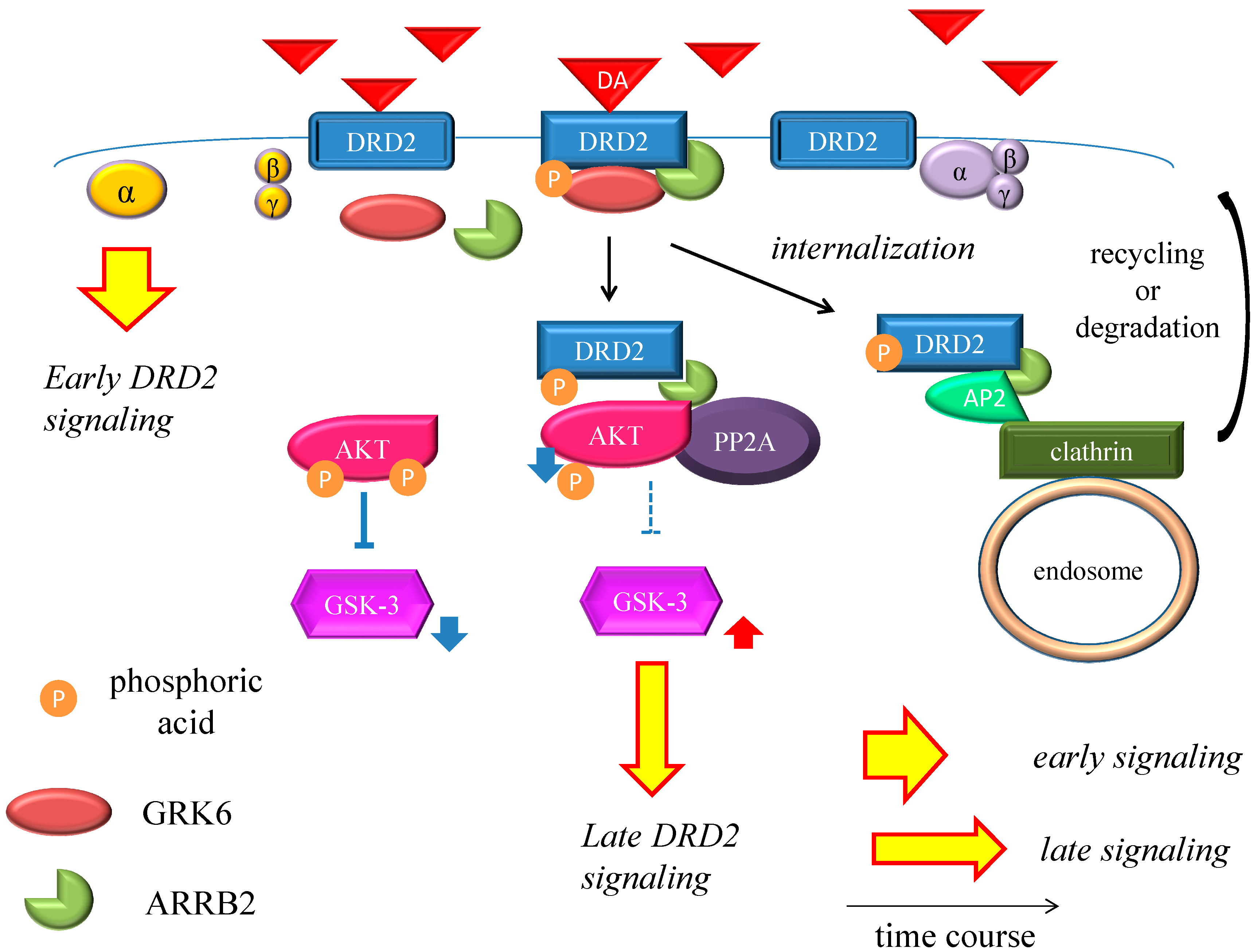
Dopamine supersensitivity psychosis (DSP) is observed in patients with schizophrenia under antipsychotic treatment, and it is characterized by rebound psychosis, an uncontrollable psychotic episode following a stable state and tardive dyskinesia. DSP, first described in patients taking typical antipsychotics in the late 1970s, sometimes appears even in patients who are treated with current atypical antipsychotics. It was recently demonstrated that DSP can have a negative impact on the long-term prognosis of schizophrenia patients and that DSP could be involved in the etiology of some cases of treatment-resistant schizophrenia. Accumulating evidence suggests that an up-regulation of dopamine D2 receptors (DRD2) in the brain caused by long-term exposure to antipsychotics is related to the DSP phenomenon. The present review describes the clinical characteristics and the etiology of DSP in the era of second-generation antipsychotics for patients with schizophrenia. Based on the mechanism of DSP, several potential treatments for patients presenting with a DSP episode or the dopamine supersensitivity state are also discussed.
What is supersensitivity psychosis?
Supersensitivity psychosis is a recognized complication of long-term antipsychotic treatment, in which patients develop new or reemergent psychotic symptoms, generally accompanied by dyskinetic movements, due to prolonged dopamine receptor blockade and resultant supersensitivity. Though it is most closely associated with schizophrenia and the use of typical antipsychotic agents, it has also been documented in patients with other diagnoses, and in those receiving atypical antipsychotics. There is no established treatment for this condition. In this paper, we describe a patient with persistent delusional disorder, jealous type, who developed a supersensitivity psychosis characterized by persecutory delusions, auditory hallucinations, and thought insertion in association with mild tardive dyskinesia. These symptoms resolved completely following six weeks of treatment with the second-generation antipsychotic asenapine, 20 mg/day. The mechanisms and implications of the patient's symptomatology and response are discussed.
What is the first line of treatment for psychotic disorders?
The first-line treatment for psychotic disorders remains antipsychotic drugs with receptor antagonist properties at D2-like dopamine receptors. However, long-term administration of antipsychotics can upregulate D2 receptors and produce receptor supersensitivity manifested by behavioral supersensitivity to dopamine stimulation in animals, and movement disorders and supersensitivity psychosis (SP) in patients. Antipsychotic-induced SP was first described as the emergence of psychotic symptoms with tardive dyskinesia (TD) and a fall in prolactin levels following drug discontinuation. In the era of first-generation antipsychotics, 4 clinical features characterized drug-induced SP: rapid relapse after drug discontinuation/dose reduction/switch of antipsychotics, tolerance to previously observed therapeutic effects, co-occurring TD, and psychotic exacerbation by life stressors. We review 3 recent studies on the prevalence rates of SP, and the link to treatment resistance and psychotic relapse in the era of second-generation antipsychotics (risperidone, paliperidone, perospirone, and long-acting injectable risperidone, olanzapine, quetiapine, and aripiprazole). These studies show that the prevalence rates of SP remain high in schizophrenia (30%) and higher (70%) in treatment-resistant schizophrenia. We then present neurobehavioral findings on antipsychotic-induced supersensitivity to dopamine from animal studies. Next, we propose criteria for SP, which describe psychotic symptoms and co-occurring movement disorders more precisely. Detection of mild/borderline drug-induced movement disorders permits early recognition of overblockade of D2 receptors, responsible for SP and TD. Finally, we describe 3 antipsychotic withdrawal syndromes, similar to those seen with other CNS drugs, and we propose approaches to treat, potentially prevent, or temporarily manage SP.
Is supersensitivity psychosis a side effect of neuroleptic therapy?
Supersensitivity psychosis has emerged as a potential side effect of long-term neuroleptic therapy that may be similar to tardive dyskinesia. Schizophrenic patients with supersensitivity psychosis and considered to be drug-resistant were treated with anti-epileptic medication. Forty-three separate trials were conducted on a total of 35 patients. Over half improved on clinical global impression, some of them considerably. We propose that antiepileptic drugs ameliorate supersensitivity psychosis and so-called "drug-resistant" schizophrenic patients by correcting a pharmacological kindling effect in the limbic system which results from chronic neuroleptic therapy.