What is the importance of selective toxicity?
In respect to this, what is selective toxicity and why is it important? An important quality for an antimicrobial drug is selective toxicity, meaning that it selectively kills or inhibits the growth of microbial targets while causing minimal or no harm to the host. Likewise, what allows for selective toxicity in a medication?
What are the new targets for selective toxicity?
Then, the selective toxicity was improved to include targets such as the different ribosomal units that participate in protein synthesis. From there, the targets became the topoisomerase and polymerases that carry out nucleic acid synthesis.
Are there economically valuable uses of selectively toxic agents in veterinary practices?
There have been many economically valuable uses of selectively toxic agents in veterinary practices in spite of the fact that the remedies devised for human illness cannot always be used in veterinary because of their high cost.
What is selective toxicity of antibiotics?
The selective toxicity of antibiotics means that they must be highly effective against the microbe but have minimal or no toxicity to humans. In practice, this is expressed by a drug's therapeutic index (TI) - the ratio of the toxic dose (to the patient) to the therapeutic dose (to eliminate the infection).
How can selective toxicity guide treatment?
An important quality for an antimicrobial drug is selective toxicity, meaning that it selectively kills or inhibits the growth of microbial targets while causing minimal or no harm to the host.
What is selective toxicity?
The selective toxicity may be defined as adverse effect of a chemical to one form of life (cell or organism) without affecting other form of life, even though the two may exist in intimate contact .
What is selective toxicity and why is it important?
The selective toxicity of antibiotics means that they must be highly effective against the microbe but have minimal or no toxicity to humans. In practice, this is expressed by a drug's therapeutic index (TI) - the ratio of the toxic dose (to the patient) to the therapeutic dose (to eliminate the infection).
What is selective toxicity example?
Because human cells do not make peptidoglycan, this mode of action is an excellent example of selective toxicity. Antibiotics that inhibit the cell wall biosynthesis of bacteria include the penicillins (including ampicillin, amoxicillin, and methicillin), cephalosporins, vancomycin, and bacitracin.
What is selective toxicity and why is it important quizlet?
What is selective toxicity and why is it important? Antimicrobial drugs must often act within the host without damaging the host. Unlike disinfectants.
What allows for selective toxicity in a medication quizlet?
Selective toxicity takes advantage of structural differences between host and pathogen. B. To be effective, an antimicrobial agent must be more toxic to the patient than the pathogen.
Which mode of action would be most selectively toxic?
b. High , low.- Because penicillin attacks the cell walls and we do not have cell walls .- Because fungal and parasitic cells have similar structures to eukaryote cells and those antibiotics target human cells . ... -“ 1 thing that can happen is spontaneous mutations in critical chromosomal genes .
What is selective toxicity describe one example of selective toxicity?
The selective toxicity of ß-lactams, for example, is considered to be due to their affinity to penicillin binding proteins (PBPs) and inhibition of biosynthesis of bacterial cell walls, both being unique to prokaryotes [4, 5].
Why is selective toxicity important?
Also know, what is selective toxicity and why is it important? An important quality for an antimicrobial drug is selective toxicity, meaning that it selectively kills or inhibits the growth of microbial targets while causing minimal or no harm to the host .
What does selective toxicity mean in medicine?
37 Votes) The selective toxicity of antibiotics means that they must be highly effective against the microbe but have minimal or no toxicity to humans. In practice, this is expressed by a drug's therapeutic index (TI) - the ratio of the toxic dose (to the patient) to the therapeutic dose (to eliminate the infection).
Antimicrobial Definition
Bacteria, viruses, and other microorganisms are everywhere in the environment. They are even inside of the human body. There are some microorganisms that are desirable in the body, but others are not. Most microorganisms are not harmful to the body, but the ones that are can really wreak havoc in the body.
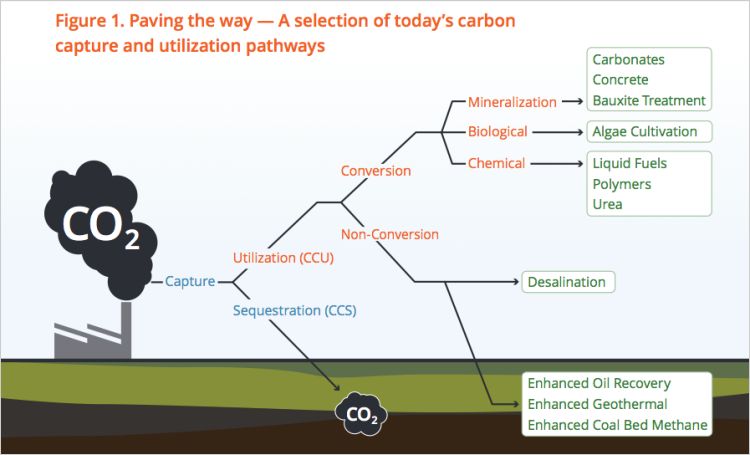
Antimicrobial Agents
As the name suggests, antimicrobial agents are any agents that are used against living microorganisms. These agents come in the form of chemicals that can be used inside of the body and other ones that can be used in the environment.
Antimicrobial Drugs
Scientists had to come up with a way to address the harmful bacteria that enter the body. The problem was that there are many similarities between microorganism cells and human cells.
What is selective toxicity?
Remember that selective toxicity is the specific inhibition of some types of cells but not others. In the case of antimicrobial drugs, we want the drug to be selectively toxic for whatever microorganism is infecting us and not kill our own cells.
Why is selective toxicity easier to achieve for bacteria than for eukaryotic pathogens?
That's because bacteria, being prokaryotes, are very different from our own cells.
Why is selective toxicity advantageous?
It is advantageous because there are less chances of normal human cell to be affected by drug thus leading to lesser side effects (2012).
How to treat heterogeneous cancer?
One way of treating the heterogeneous state of cancer is by administering combinatorial drug therapies. In this method, various drugs are used for targeting different genes and factors. It has been found to be useful in some cases however not in every case, as they mainly target drugs related to cancer dividing cells and not the non-dividing cancerous cells. So therefore future area of research mainly focus on drug development for inhibiting the non-dividing cancer cells (Bhatia et al., 2012).
Is anti-cancer drug toxic?
Most of the anti-cancer drugs are hydrophobic in nature for which we require solubilizing solvent for product formulation. These solvents are toxic in nature and may be harmful if used for chemotherapy. Poor selectivity of anti-cancer drugs may lead to improper functioning of normal human cells and may induce adverse reactions, free radicals, inflammatory factors causing various side effects. Various anti- cancer drugs are unable to enter the cancerous cells due to which their pharmacological activity is inhibited. Thus drug administered to patient may not produce any therapeutic effects and this phenomenon is known as multi-drug resistance.
What are the factors that affect selective toxicity?
It can be concluded that there are three important factors to consider in selective toxicity of a drug, they are the tumour, drug and most especially the host. There have been a lot of improvement with using chemotherapy to manage cancer even though they cause severe side effects and resistance. Other challenges faced are the cost, time involved and the high mortality rate. This has brought about increase in effort of scientists to search for ways for the body to fight cancer tissue and find better cytotoxic agents to fight cancer cells.
Why is chemo important for cancer patients?
This is also important as it gives the possibility of a longer life because it is controlled like a disease that is chronic like diabetes. Last is palliation, which is important when cancer is at an advanced stage. Chemotherapy drugs in this case can be used to relieve symptoms or improve the patients quality of life.
How does chemo work?
In cancerous cells, the checkpoints are damaged causing the cancer cells to continue to grow out of control. Chemotherapy works by damaging the genes present inside the nucleus of cells. Some drugs work by damaging cells when they are beginning to divide or while copies are being made. Chemotherapy drugs cause the cancerous cells to think that their lifespan has finished which leads to apoptosis.
Why are normal cells damaged by chemo?
Normal cells that divide rapidly are damaged by these chemotherapeutic agents because they cannot differentiate between cell reproducing normal tissues and cancer cells as they are not highly selective therefore causing the following side effects (Salmon & Sartorelli, 1998).