Are macrolides effective in the treatment of Mycoplasma pneumoniae pneumoniae?
However, clinicians should practice prudent use of macrolide drugs due to the emergence of macrolide-resistant strains of M. pneumoniae. Resistance to macrolides has been emerging in M. pneumoniae since the 2000s. This issue is especially troubling in Asia, where resistance rates have been as high as 90%.
What is the treatment for Mycoplasma pneumoniae?
Treatment. However, if someone develops pneumonia (lung infection) caused by M. pneumoniae, doctors usually prescribe antibiotics as treatment. Antibiotics can help patients recover from the illness faster if started early on. There are several types of antibiotics available to treat pneumonia caused by M. pneumoniae.
Is Mycoplasma pneumoniae resistant to some antibiotics?
Some M. pneumoniae are resistant to some antibiotics used for treatment. Learn more about the potential danger of antibiotic resistance, and how to prevent it at CDC’s Be Antibiotics Aware website.
What is the prognosis of Mycoplasma pneumoniae?
The symptoms and signs of pneumonia usually resolve within a few days without any complications. However, in young children, the infection can be associated with severe pneumonia, and in patients with sickle cell anemia, it may be associated with acute chest syndrome. The immunity after a Mycoplasma pneumoniae infection is short-lived.
See more
Which drug is not recommended for treating pneumonia caused from Mycoplasma pneumoniae?
Clinicians should not prescribe fluoroquinolones and tetracyclines for young children under normal circumstances. Macrolides are generally considered the treatment of choice. However, clinicians should practice prudent use of macrolide drugs due to the emergence of macrolide-resistant strains of M. pneumoniae.
What drug treats Mycoplasma pneumoniae?
Medication Summary The second-generation tetracyclines (doxycycline) and macrolides are the drugs of choice. Macrolide resistance has been reported in several areas of the world, but most experts agree that macrolides are the antibiotics of choice for treating M pneumoniae infections in adults and children.
What is the first line antibiotic for treating Mycoplasma pneumoniae?
Macrolides and related antibiotics are the first-line treatment of M. pneumoniae respiratory tract infections mainly because of their low MIC against the bacteria, their low toxicity and the absence of contraindication in young children.
How long does it take to get rid of Mycoplasma pneumoniae?
How Is Mycoplasma Pneumonia Treated? Oral antibiotics are given, usually for 5 to 14 days, to treat the infection. Improvement usually begins within 1 or 2 days of starting antibiotics, but the cough may last for weeks. Nasal sprays and oral decongestants are often used for nasal symptoms.
Which of the following would you prescribe to treat a person with M pneumoniae?
Macrolides and related antibiotics are the first-line treatment of M. pneumoniae respiratory tract infections mainly because of their low MIC against the bacteria, their low toxicity and the absence of contraindication in young children.
Can you recover from Mycoplasma without antibiotics?
Most people recover very slowly and completely without antibiotics, although antibiotics may speed recovery. Allowed to progress in rare susceptible individuals (the elderly and immune-compromised individuals), mycoplasmas can cause hepatitis, pancreatitis, arthritis, heart disease, anemia, or neurologic disease.
How long does azithromycin take to cure Mycoplasma?
Five-day Azithromycin Treatment Regimen for Mycoplasma genitalium Infection Also Effectively Eradicates Chlamydia trachomatis. Chlamydia trachomatis and Mycoplasma genitalium are the most frequent aetiologies of non-gonococcal urethritis (NGU) (1–3). There are no international management guidelines for M.
How long does Mycoplasma last after treatment?
Variable, usually 2 to 35 days.
What is the best antibiotic for walking pneumonia?
Antibiotics that are used to treat walking pneumonia caused by Mycoplasma pneumoniae include: Macrolide antibiotics: Macrolide drugs are the preferred treatment for children and adults. Macrolides include azithromycin (Zithromax®) and clarithromycin (Biaxin®).
What happens if mycoplasma pneumonia goes untreated?
Complications from Mycoplasma pneumonia Long-term MP is rare, but some research suggests that it could play a role in chronic lung disease. In rare cases, untreated MP can be fatal. Other potential complications of MP include : respiratory failure.
Does mycoplasma pneumonia require isolation?
Because of the endemicity of infection with M pneumoniae in susceptible populations, isolating patients is seldom practical and generally is not recommended.
Is Mycoplasma permanent?
Mycoplasma is forever; once it is in your flock, it is there to stay. The best treatment is prevention.
What is the treatment for M pneumonia?
Most patients with M. pneumoniaepneumonia present in outpatient settings, and treatment is often with empiric antibiotics for atypical pneumonia. Note that many patients may undergo a period of symptomatic management before seeking medical attention and/or receiving antibiotic treatment.
Who is involved in mycoplasma pneumonia?
Mycoplasma pneumonia is often encountered by the primary care provider, nurse practitioner, emergency department physician, and internist. As such, it requires the efforts of an interprofessional team that includes clinicians (MDs, DOs, NPs, and PAs), specialists, nurses, and pharmacists. Cross-disciplinary communication within this interprofessional arrangement will result in better patient outcomes. [Level 5]
Why does mycoplasma pneumoniae slough?
The prolonged refractory cough is considered to be due to inhibition of the ciliary movement.
How is mycoplasma transmitted?
M. pneumoniae is now considered a common cause of community-acquired pneumonia and is transmitted from person to person via respiratory droplets during close contact. It has an incubation period that ranges between 2 to 3 weeks. Like most respiratory pathogens, infection usually occurs during the winter months but can happen year-round. Estimates show that around 1% of the population of the United States is infected annually. Incidence may be much higher since infection can be subclinical or cause milder disease that does not require hospitalization. Outbreaks of mycoplasma infection occur in military recruits, hospitals, nursing homes, and other long-term care facilities. [5][4] Only 5 to 10% of people infected with Mycoplasmadevelop pneumonia. It causes upper and lower respiratory tract infections in all age groups, particularly more than 5 years and less than 40 years of age.
How long does it take to treat M pneumonia?
Azithromycin is the most frequently used antibiotic and is usually prescribed for 5 days (500 mg for the first dose, followed by 250 mg daily for 4 days). Patients receiving doxycycline or fluoroquinolones should be given 7 to 14 days of treatment. [11][12] Macrolide resistance continues to emerge, so if a patient is not responding to macrolides, other antibiotics can be given. Routine antibiotic prophylaxis is not required for the exposed contacts except for those prone to serious mycoplasmal infection, like patients with sickle cell disease or antibody deficiency. For prophylaxis, doxycycline or macrolides are used.
What are the best ways to prevent pneumonia?
Patients need counsel regarding infection prevention. This includes information regarding getting the pneumococcal vaccine, as well as the influenza vaccine, which in addition to helping prevent influenza, can thwart possible complications, such as pneumonia. If the patient smokes, they should receive strong counsel and support to stop, as it can preclude pneumonia and other health concerns. Addressing any underlying conditions (e.g., asthma, diabetes, congestive heart failure) can also help prevent pneumonia.
What are the symptoms of pneumonia?
Chest soreness from coughing is common. Wheezing can also occur. Other respiratory symptoms include pharyngitis, rhinorrhea, and ear pain. Pleural effusion occurs in 15% to 20% of patients who develop pneumonia and may predict increased morbidity and mortality.
How prevalent is macrolide resistance?
Current data suggest that the prevalence of macrolide resistance in M. pneumoniae may be around 10% in the United States, with regional variability. Studies have reported that patients with infections due to macrolide-resistant strains may have fever and cough for a longer duration than patients infected with macrolide-sensitive strains.
Can a doctor prescribe fluoroquinolones for children?
Fluoroquinolones: Adults. Tetracyclines (e.g., doxycycline): Older children and adults. Clinicians should not prescribe fluoroquinolones and tetracyclines for young children under normal circumstances. Macrolides are generally considered the treatment of choice.
Is M. pneumoniae resistant to antibiotics?
Antibiotic Resistance. Resistance to macro lides has been emerging in M. pneumoniae since the 2000s. This issue is especially troubling in Asia, where resistance rates have been as high as 90%. The United States and Europe have also reported macrolide resistance.
Is mycoplasma pneumoniae resistant to penicillin?
pneumoniae with antibiotics. All mycoplasmas lack a cell wall and, therefore, all are inherently resistant to beta-lactam antibiotics (e.g., penicillin).
What is mycoplasma pneumonia?
Mycoplasma pneumoniais a common respiratory pathogen that produces diseases of varied severity ranging from mild upper respiratory tract infection to severe atypical pneumonia. Apart from respiratory tract infections, this organism is also responsible for producing a wide spectrum of non-pulmonary manifestations including neurological, ...
How many patients had M. pneumoniae?
They found atypical bacteria in 56% of chronic, stable asthmatics who had experienced no exacerbations within 3 months of enrollment. Twenty three had M. pneumoniae, two patients had other pathogenic mycoplasma but only one control had mycoplasma in the airways.
What is the main adhesion protein for mycoplasmas?
The major adhesion is P1 adhesin. Cytoadhesion protects mycoplasmas from mucociliary clearance. Hydrogen peroxide is produced locally, which has a cytopathic effect on airway epithelium and cilia and is responsible for persistent cough. Mycoplasma is also being incriminated in the development of autoimmunity which can explain the extra pulmonary involvement. Production of multiple arrays of cytokines and other reactive substances in the pathogenesis[4] of M. pneumoniaelung disease has been a subject of considerable interest during past several years.
What is the most frequent extra pulmonary complications of M. pneumoniaeinfection?
Central nervous system (CNS) manifestations are the most frequent extra-pulmonary complications of M. pneumoniaeinfection and can at times be life threatening.[25]
How common is M. pneumoniae?
M. pneumoniaecauses up to 40% or more of community acquired pneumonia (CAP) cases and as many as 18% of cases requiring hospitalizations in children.[14] Older studies reported M. pneumoniaepneumonia to be somewhat uncommon in children aged less than five years and greatest among school aged children 5-15 years of age with decline after adolescence and on into adulthood.[15] However, the latter studies have documented that M. pneumoniaemay occur endemically and occasionally epidemically in older persons, as well as in children under five years of age. These findings may reflect improved detection abilities that were unavailable in the 1960s and 1970s when the first epidemiological descriptions of M. pneumoniaewere published.
Is M. pneumoniae a pulmonary pathogen?
Although, M. pneumoniaeis a well recognized pulmonary pathogen in the West , information on disease prevalence in our country is sparse due to non-availability of reliable, rapid diagnostic techniques as well as the lack of clinical awareness. A study[10] at a tertiary care center at Delhi reported M. pneumoniaeinfection in 18(24%) of 75 children with CAP using the criteria of culture and/or serology and/or a positive PCR assay on nasopharyngeal aspirate.
Is M. pneumoniae asymptomatic?
M. pneumoniaeis ordinarily mild, and many adult cases may be asymptomatic, whereas this is much less common in children, perhaps reflecting some degree of protective immunity for reinfections. Although most infections occur among outpatients (hence the colloquial term walking pneumonia), M. pneumoniais a significant cause of bacterial pneumonia in adults requiring hospitalization in USA. Marston et al.[19] report that M. pneumoniaewas definitively responsible for 5.4% and possibly responsible for 32.5% of 2776 cases of CAP in hospitalized adults based on complement fixation (CF) test for detection of infections. An additional striking finding of this study was their observation that the incidence of pneumonia due to M. pneumoniaein hospitalized adults increased with age and it was second only to S. pneumoniaein elderly persons.
What is the first line of treatment for M pneumonia?
Macrolides and related antibiotics are the first-line treatment of M. pneumoniaerespiratory tract infections mainly because of their low MIC against the bacteria, their low toxicity and the absence of contraindication in young children.
What is mycoplasma pneumoniae?
Mycoplasma pneumoniaeis responsible for community-acquired respiratory tract infections, such as tracheobronchitis and pneumonia, particularly in school-aged children and young adults. These infections occur both endemically and epidemically at 3-to-7-year intervals worldwide (Atkinson et al., 2008). Numerous extra-respiratory manifestations of ...
What is the rate of macrolide resistance in the USA?
In the USA and Canada, rates have been recently reported between 3.5 and 13.2% (Table (Table2).2). In Europe, rates have remained below 10% except in Italy were a rate of 26% was observed on a small number of M. pneumoniae-positive specimens collected during an outbreak (Chironna et al., 2011).
What antimicrobials are resistant to M. pneumoniae?
pneumoniaeis intrinsically resistant to beta-lactams and to all antimicrobials targeting the cell wall, such as glycopeptides and fosfomycin. M. pneumoniaeis also resistant to polymixins, sulfonamides, trimethoprim, rifampicin and linezolid (Bébéar and Kempf, 2005; Bébéar et al., 2011). Antibiotics with potential activity against M. pneumoniaethat are used in clinical practice include macrolides, lincosamides, streptogramin combinations and ketolides (MLSK), tetracyclines and fluoroquinolones. These drugs achieve high intracellular concentration in mammalian cells and are thereby able to reach intracellular mycoplasmas. The MICs of the main antibiotics belonging to the MLSK group are the lowest against M. pneumoniaecompared with those of the two other classes, except MIC of lincomycin that is high (see MIC of the sensitive reference strain M129 (ATCC 29342) in Table Table1;1; Bébéar et al., 2011). MICs of tetracyclines and fluoroquinolones are about 10 times higher than those of MLSK, but newer fluoroquinolones such as levofloxacin and moxifloxacin show an enhanced activity against M. pneumoniae. Only fluoroquinolones and ketolides have a potential bactericidal action. Other antibiotics such as aminoglycosides and chloramphenicol show some activity against M. pneumoniae(MICs 2–10 μg/ml for chloramphenicol and MIC 4 μg/ml for gentamicin, Bébéar et al., 2011) but are not recommended for M. pneumoniaeinfections.
What antibiotics are used for M. pneumoniae?
MICs of MLSK, tetracycline and fluoroquinolone antibiotics for M. pneumoniaeclinical isolates resistant to macrolides and genetically characterized.
Is there a kit for macrolide resistance?
Currently, this strategy is hampered by the lack of commercially available sensitive kits that detect macrolide resistance-associated mutations. However, such kits are currently in development and may soon become available. They will be useful for routine diagnostics in microbiology laboratories.
Is M. pneumoniaemacrolide resistant?
Nowadays , M. pneumoniaemacrolide resistance rates are extremely high in Asia and remain moderate in Europe and North America. Macrolide resistance detection using accurate molecular methods should be considered in all M. pneumoniae-positive specimens since it has both a direct application in clinical practice and an epidemiological surveillance interest. At the individual level, a rapid detection of resistance-associated mutations would enable the prompt prescription of an alternative antimicrobial regimen, especially in case of persistent or recurrent M. pneumoniaeinfection. At the community level, the high prevalence of macrolide-resistant M. pneumoniaeisolates in Asia underscore the potential for rapid emergence of macrolide resistance within M. pneumoniaein other parts of the world. Thus, further epidemiological studies are needed in Europe and the USA to monitor macrolide resistance rates. Moreover, macrolide stewardship may be needed for restricting the use of these antibiotics, reduce unnecessary antibiotic prescribing, especially in countries with remaining low macrolide resistant rates. In Asia, the epidemiological surveillance of antibiotic resistance would also be of interest to early detect potential selections of fluoroquinolone- and tetracycline-resistant clinical isolates associated with the increasing use of these classes of antibiotics.
What is the treatment for M. pneumoniae?
Treatment may be adjusted according to infection mechanism such as antibiotics, corticosteroids, intravenous immunoglobulin[3,12,13]. Antimicrobial treatment , especially macrolides, may be sufficient for CNS involvement associated with M. pneumoniae, beside the beneficial effect of treatment with steroids this treatment must be considered with direct invasion of CNS by the organism when other causative agents have been excluded. Plasma exchange has also been reported and seemed to be beneficial. In our case series, two patients with encephalitis and transverse myelitis were treated with high dose steroid; the other two patients diagnosed as Guillain-Barre syndrome received intravenous immuneglobulin as did some authors in literature[3,12,13].
What are the consequences of M. pneumoniae?
pneumoniae infections usually resolve completely, but they can result in chronic debilitating deficits in motor or mental function with varying degrees of life threatening complications. Peripheral neurological sequelae such as radiculitis and transverse myelitis are the risk factors for chronic CNS sequels. Mental retardation, brain atrophy, hydrocephalus, epilepsy, visual changes, and global neurologic deficits with brain stem dysfunction and cerebellar ataxia may be seen after encephalitis. More severe neurologic consequences were noted in 20–60% of cases in large patient series. We encountered wide based gait with mild spasticity at lower extremities after mycoplasma encephalitis, and urinary sphincter dysfunction after transverse myelitis. It is important keeping in mind M. pneumoniae with various neurological symptoms.
Is M. pneumoniae a respiratory disease?
M.pneumonia is a respiratory pathogen recognized as a common etiology of upper tract respiratory illness and pneumonia[1,2]. Serologic diagnosis of Mycoplasma is difficult and problematic. The utility of IgM antibodies of M. pneumoniaevaries with age; it is usually positive in acute infection but also may be negative in the course of acute infection or positivity may last for months[1,2]. Central nervous system complications have been reported with Mycoplasma infection. Cerebellar syndrome, polyradiculitis, cranial nerve palsies, aseptic meningitis, meningoencephalitis, acute disseminated encephalomyelitis, coma, optic neuritis, diplopia, mental confusion and, acute psychosis secondary to encephalitis, cranial nerve palsy, brachial plexus neuropathy, ataxia, choreoathetosis, and ascending paralysis (Guillain-Barre syndrome) are neurologic compli-cations seen with M. pneumoniaeinfection[1]. Encephalitis is most frequent extrapulmonary complication of M. pneumoniaemanifested with fever, seizures, meningeal signs, ataxia, focal neurologic deficits, and altered behavior, ranging from minor changes to lethargy in pediatric population[2-4,6-8]. Twenty percent of patients or more with CNS findings have no preceding or concomitant diagnosis of respiratory infection[2-4,6-8]. Among our five cases, two had respiratory symptoms at the beginning of M. pneumoniaeinfection. One of them was diagnosed as encephalitis and second one was diagnosed as Guillain-Barre syndrome with normal CSF protein levels.
Can mycoplasma cause vasculitis?
Central nervous system infections and inflammatory or autoimmune disorders may cause secondary central nervous system vasculitis. Mycoplasma may cause secondary central nervous system vasculitis in children[14]. Neuropsychiatric symptoms, seizures, cerebral infarction or other focal neurologic deficits may be seen with CNS vasculitis secondary to infection by inflammation of the cerebral blood vessels by direct pathogen invasion or due to an immune-mediated response provoked by molecular mimicry, immune complex deposition, secretion of cytokines, and/or super antigen mediated responses[14]. One of our patients with encephalitis also had vasculitis of internal carotid artery and posterior circulation. She had neuropsychiatric manifestations.
What is mycoplasma infection?
Mycoplasma is a bacteria (or germ) that can infect different parts of your body. Which body part is affected--your lungs, skin, or urinary tract, depends on which type of mycloplasma bacteria is causing your infection.#N#All mycloplasma infections have one thing in common though. Unlike other bacteria, mycloplasma do not have cell walls. They are also very small compared to other bacteria. That's important because many antibiotics kill bacteria by weakening those walls. Since mycoplasma bacteria don't have them, some antibiotics, like penicillin, won't work against them.
How many types of mycoplasma are there?
There are about 200 types of mycoplasma bacteria, but most of them are harmless. The ones you may have to worry about are:
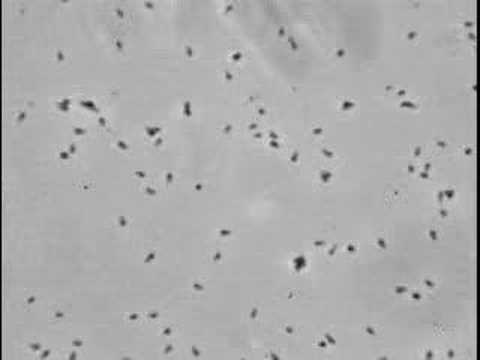
Which body part is affected by mycloplasma?
Which body part is affected--your lungs, skin, or urinary tract, depends on which type of mycloplasma bacteria is causing your infection. All mycloplasma infections have one thing in common though. Unlike other bacteria, mycloplasma do not have cell walls. They are also very small compared to other bacteria.
What is walking pneumonia?
This type causes lung infections. About a third of people who get infected come down with a mild form of pneumonia called " walking pneumonia ." It is referred to as an atypical pneumonia because most people, especially children, will get "tracheobronchitis," a fancy name for a chest cold.
Which is superior to serology for the diagnosis of acute Mycoplasma pneumoniae infection?
Nilsson AC , Björkman P , Persson K. Polymerase chain reaction is superior to serology for the diagnosis of acute Mycoplasma pneumoniae infection and reveals a high rate of persistent infection. BMC Microbiol 2008; 8:93.
What is a mycoplasma?
Mycoplasmas are bacteria and are the smallest free-living organisms.
How many Mycoplasma species are there?
Over 120 named Mycoplasma species exist and 13 Mycoplasma species, 2 Acholeplasma species, and 1 Ureaplasma species have been isolated from humans. However, only four species are well-established human pathogens [ 1 ]:
Is UpToDate a substitute for medical advice?
The content on the UpToDate website is not intended nor recommended as a substitute for medical advice, diagnosis, or treatment. Always seek the advice of your own physician or other qualified health care professional regarding any medical questions or conditions. The use of UpToDate content is governed by the UpToDate Terms of Use. ©2021 UpToDate, Inc. All rights reserved.
Is Mycoplasma pneumoniae a pathogen?
Mycoplasma pneu moniae is one of the smallest free-living organisms and a common bacterial respiratory tract pathogen. Upper respiratory tract infections and acute bronchitis are the most common manifestations of M. pneumoniae infection, but pneumonia can also occur.
What is the best herb for mycoplasma?
Mullein. Mullein is a gentle but powerful herb. It is an anti-bacterial herb and suitable for treating mycoplama. It is especially useful if the mycoplasma infection is in the lungs. Mullein can be taken as a tincture or as a tea. It is easy to take as a tea, sweetened with a little honey.
What is a Mycoplasma Infection?
Mycoplasma are unique form of bacteria that do not have a cell wall. This makes them able to take on different shapes and "hide." They are difficult to test for and can be difficult to treat.
What are the health problems caused by mycoplasma fermentans?
Micoplasma pneumoniae can cause health problems like pneumonia (walking pneumonia), sore throat, fever, blood problems, kidney disease, and joint and muscle diseases. Mycoplasma fermentans can cause pneumonia, TMJ, fibromyalgia, and headaches, among other diseases.
What are the best foods to eat to prevent mycoplasma?
It is important to provide the body with plenty of nutrients and avoid empty calories that depress the immune system. Sugar and processed flour products should be avoided except for special occasions. Fresh fruits and vegetables should be consumed liberally.
Can mycoplasma cause respiratory problems?
The range of symptoms caused by mycoplasma is vast, another factor in making a diagnosis difficult. The bacteria can settle into any number of systems or organs of the body causing a variety of symptoms, including but certainly not limited to, respiratory problems, blood diseases, nervous system diseases, headaches, neurological problems, ...
Can you take serrapeptase on an empty stomach?
Serrapeptase dissolves non-living tissue and has few reported side effects. Serrapeptase should be taken on an empty stomach according to manufacturer's directions.
Is mycoplasma tincture good for urinary tract infections?
For mycoplasma infections that affect the urinary system, this is a wonderful anti-bacterial herb. It is most commonly taken as a tincture.